J Korean Soc Radiol.
2016 Dec;75(6):455-465. 10.3348/jksr.2016.75.6.455.
Pulmonary Embolism Overlooked on Chest CT Under the Application of the American College of Radiology Appropriateness Criteria
- Affiliations
-
- 1Department of Radiology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 2Department of Radiology, St. Paul's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. leebae@catholic.ac.kr
- KMID: 2360433
- DOI: http://doi.org/10.3348/jksr.2016.75.6.455
Abstract
- PURPOSE
We retrospectively estimated the frequency and clinical significance of pulmonary embolism (PE) that would have been missed on chest CT scans if the American College of Radiology (ACR) appropriateness criteria were applied and contrast enhanced CT scans were not performed.
MATERIALS AND METHODS
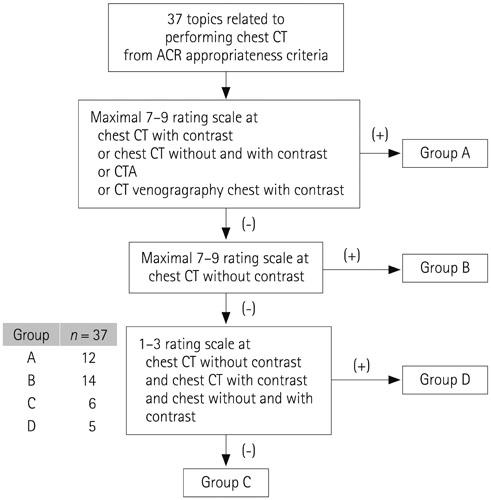
From 2007 to 2014, a total of 696 patients with acute PE were reviewed. The ACR appropriateness criteria relevant to performing a chest CT scan were reorganized into 37 clinical topics (reasons for performing CT). Furthermore, based on the strength of recommendation for CT contrast usage, topics were divided into Group A (appropriate), Group B (not appropriate), Group C (may be appropriate), and Group D (no CT). The patients were assigned into groups and compared for the clinical characteristics and prognostic CT findings.
RESULTS
Four hundred ninety-one patients were assigned into Group A (70.5%), 104 patients were assigned into Group B (14.9%), 101 patients were assigned into Group C (14.5%), and none of the patients were assigned into Group D. Patients in Group C (69.3 ± 14.6 years) were significantly older (p < 0.001) than those in the other groups. The most common reason for performing CT in Group B was screening of pulmonary metastasis (72%).
CONCLUSION
Under circumstances of many pulmonary emboli without clinical suspicion, PE could be overlooked under the application of contrast usage criteria, especially in patients in old age and with underlying malignancy. Such a recommendation can be useful to determine the usage of CT contrast in patients with a complex medical background.
MeSH Terms
Figure
Reference
-
1. Goldhaber SZ, Visani L, De Rosa M. Acute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER). Lancet. 1999; 353:1386–1389.2. Carson JL, Kelley MA, Duff A, Weg JG, Fulkerson WJ, Palevsky HI, et al. The clinical course of pulmonary embolism. N Engl J Med. 1992; 326:1240–1245.3. Moser KM. Venous thromboembolism. Am Rev Respir Dis. 1990; 141:235–249.4. Moon SM, Seon HJ, Baek JM, Lee SJ, Yoon YH, Kim YH. Diagnostic usefulness of dual-energy computed tomography in evaluation of the severity of acute pulmonary thromboembolism. J Korean Soc Radiol. 2015; 72:38–45.5. Park GC, Lee JK. Pulmonary thromboembolism in patients with malignancy. J Korean Soc Radiol. 2014; 71:14–19.6. Dentali F, Ageno W, Becattini C, Galli L, Gianni M, Riva N, et al. Prevalence and clinical history of incidental, asymptomatic pulmonary embolism: a meta-analysis. Thromb Res. 2010; 125:518–522.7. Shteinberg M, Segal-Trabelsy M, Adir Y, Laor A, Vardi M, Bitterman H. Clinical characteristics and outcomes of patients with clinically unsuspected pulmonary embolism versus patients with clinically suspected pulmonary embolism. Respiration. 2012; 84:492–500.8. Falanga A, Russo L. Epidemiology, risk and outcomes of venous thromboembolism in cancer. Hamostaseologie. 2012; 32:115–125.9. Qanadli SD, El Hajjam M, Vieillard-Baron A, Joseph T, Mesurolle B, Oliva VL, et al. New CT index to quantify arterial obstruction in pulmonary embolism: comparison with angiographic index and echocardiography. AJR Am J Roentgenol. 2001; 176:1415–1420.10. Bankier AA, Janata K, Fleischmann D, Kreuzer S, Mallek R, Frossard M, et al. Severity assessment of acute pulmonary embolism with spiral CT: evaluation of two modified angiographic scores and comparison with clinical data. J Thorac Imaging. 1997; 12:150–158.11. Araoz PA, Gotway MB, Harrington JR, Harmsen WS, Mandrekar JN. Pulmonary embolism: prognostic CT findings. Radiology. 2007; 242:889–897.12. Bach AG, Schmoll HJ, Beckel C, Behrmann C, Spielmann RP, Wienke A, et al. Pulmonary embolism in oncologic patients: frequency and embolus burden of symptomatic and unsuspected events. Acta Radiol. 2014; 55:45–53.13. Sandhu R, Pan CX, Wun T, Harvey D, Zhou H, White RH, et al. The incidence of venous thromboembolism and its effect on survival among patients with primary bladder cancer. Cancer. 2010; 116:2596–2603.14. Shinagare AB, Guo M, Hatabu H, Krajewski KM, Andriole K, Van den Abbeele AD, et al. Incidence of pulmonary embolism in oncologic outpatients at a tertiary cancer center. Cancer. 2011; 117:3860–3866.15. Khorana AA, Francis CW, Culakova E, Kuderer NM, Lyman GH. Frequency, risk factors, and trends for venous thromboembolism among hospitalized cancer patients. Cancer. 2007; 110:2339–2346.16. Chew HK, Wun T, Harvey D, Zhou H, White RH. Incidence of venous thromboembolism and its effect on survival among patients with common cancers. Arch Intern Med. 2006; 166:458–464.17. Lee AY, Levine MN. Venous thromboembolism and cancer: risks and outcomes. Circulation. 2003; 107:23 Suppl 1. I17–I21.18. Thodiyil PA, Kakkar AK. Variation in relative risk of venous thromboembolism in different cancers. Thromb Haemost. 2002; 87:1076–1077.19. Levitan N, Dowlati A, Remick SC, Tahsildar HI, Sivinski LD, Beyth R, et al. Rates of initial and recurrent thromboembolic disease among patients with malignancy versus those without malignancy. Risk analysis using Medicare claims data. Medicine (Baltimore). 1999; 78:285–291.20. Piechowiak EI, Peter JF, Kleb B, Klose KJ, Heverhagen JT. Intravenous iodinated contrast agents amplify DNA radiation damage at CT. Radiology. 2015; 275:692–697.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Acute Pulmonary Embolism Accompanying Greater Saphenous Vein Thrombosis
- Pulmonary Bone Cement Embolism: CT Angiographic Evaluation with Material Decomposition Using Gemstone Spectral Imaging
- A Cerebral Air Embolism That Developed Following Defecation in a Patient with Extensive Pulmonary Tuberculosis: A Case Report
- Expert Opinion Questionnaire About Chest CT Scan Using A Negative Pressure Isolation Strecher in COVID-19 Patients: Image Quality and Infection Risk
- The Interobserver Agreement between Residents and Experienced Radiologists for Detecting Pulmonary Embolism and DVT with Using CT Pulmonary Angiography and Indirect CT Venography