Clin Orthop Surg.
2015 Dec;7(4):515-518. 10.4055/cios.2015.7.4.515.
Unique Imaging Features of Spinal Neurenteric Cyst
- Affiliations
-
- 1Department of Orthopaedic Surgery, Chung-Ang University College of Medicine, Seoul, Korea. ksong70@cau.ac.kr
- 2Department of Pathology, Chung-Ang University College of Medicine, Seoul, Korea.
- KMID: 2360268
- DOI: http://doi.org/10.4055/cios.2015.7.4.515
Abstract
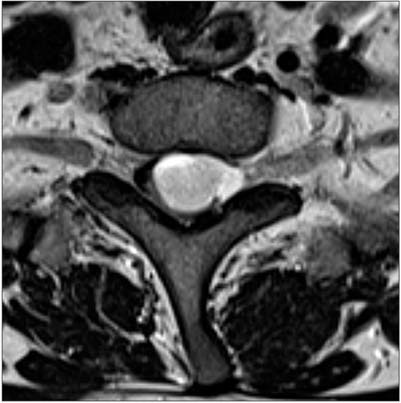
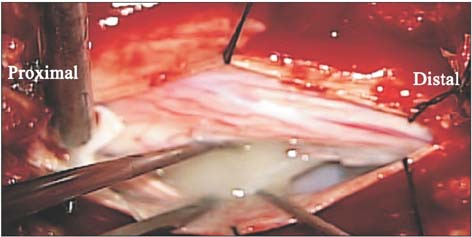
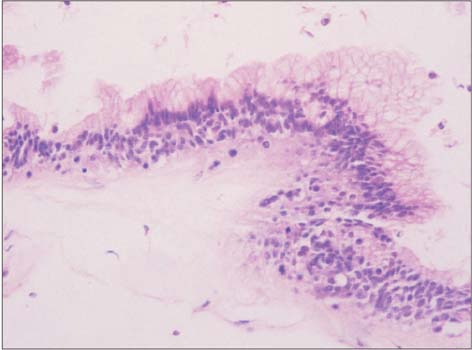
- A 50-year-old male presented with acutely progressed paraplegia. His magnetic resonance imaging demonstrated two well-demarcated components with opposite signals in one cystic lesion between the T1- and T2-weighted images at the T1 spine level. The patient showed immediately improved neurological symptoms after surgical intervention and the histopathological exam was compatible with a neurenteric cyst. On operation, two different viscous drainages from the cyst were confirmed. A unique similarity of image findings was found from a review of the pertinent literature. The common findings of spinal neurenteric cyst include an isointense or mildly hyperintense signal relative to cerebrospinal fluid for both T1- and T2-weighted images. However, albeit rarer, the signals of some part of the cyst could change into brightly hyperintensity on T1-weighted images and hypointensity on T2-weighted images due to the differing sedimentation of the more viscous contents in the cyst.
MeSH Terms
Figure
Reference
-
1. Ziu M, Vibhute P, Vecil GG, Henry J. Isolated spinal neurenteric cyst presenting as intramedullary calcified cystic mass on imaging studies: case report and review of literature. Neuroradiology. 2010; 52(2):119–123.
Article2. Agrawal D, Suri A, Mahapatra AK, Sharma MC. Intramedullary neurenteric cyst presenting as infantile paraplegia: a case and review. Pediatr Neurosurg. 2002; 37(2):93–96.
Article3. Chang IC. Thoracic neurenteric cyst in a middle aged adult presenting with Brown-Sequard syndrome. Spine (Phila Pa 1976). 2003; 28(24):E515–E518.
Article4. de Oliveira RS, Cinalli G, Roujeau T, Sainte-Rose C, Pierre-Kahn A, Zerah M. Neurenteric cysts in children: 16 consecutive cases and review of the literature. J Neurosurg. 2005; 103:6 Suppl. 512–523.
Article5. Jhawar SS, Mahore A, Goel A. Intramedullary spinal neurenteric cyst with fluid-fluid level. J Neurosurg Pediatr. 2012; 9(5):542–545.
Article6. Muzumdar D, Bhatt Y, Sheth J. Intramedullary cervical neurenteric cyst mimicking an abscess. Pediatr Neurosurg. 2008; 44(1):55–61.
Article7. Paolini S, Ciappetta P, Domenicucci M, Guiducci A. Intramedullary neurenteric cyst with a false mural nodule: case report. Neurosurgery. 2003; 52(1):243–245.
Article8. Hicdonmez T, Steinbok P. Spontaneous hemorrhage into spinal neurenteric cyst. Childs Nerv Syst. 2004; 20(6):438–442.
Article9. Alyas F, Lee J, Ahmed M, Connell D, Saifuddin A. Prevalence and diagnostic significance of fluid-fluid levels in softtissue neoplasms. Clin Radiol. 2007; 62(8):769–774.
Article