Clin Orthop Surg.
2015 Dec;7(4):476-482. 10.4055/cios.2015.7.4.476.
Patterns of Treatment for Metastatic Pathological Fractures of the Spine: The Efficacy of Each Treatment Modality
- Affiliations
-
- 1Department of Orthopedic Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. spinecjh@gmail.com
- KMID: 2360262
- DOI: http://doi.org/10.4055/cios.2015.7.4.476
Abstract
- BACKGROUND
Metastatic pathological fractures of the spine are a major problem for cancer patients; however, there is no consensus on treatment strategy. The purpose of this study was to evaluate various treatment options by analyzing their patterns for metastatic pathological fractures of the spine.
METHODS
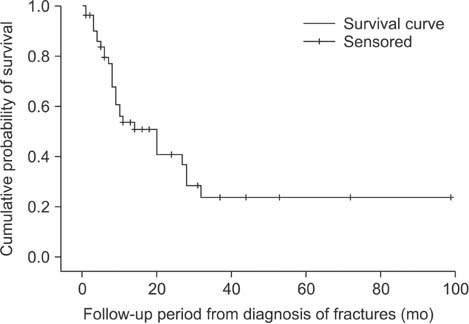
In this study, 54 patients (male:female = 36:18) who were diagnosed with metastatic pathological fractures of spine were recruited. Demographic data, origin of cancer, type of treatment, and results were obtained from electronic medical records. Treatment options were divided into radiotherapy (RT), vertebroplasty (VP) or kyphoplasty (KP), operation (OP), and other treatments. Treatment results were defined as aggravation, no response, fair response, good response, and unknown. The survival time after detection of pathologic fractures was analyzed with the Kaplan-Meier method.
RESULTS
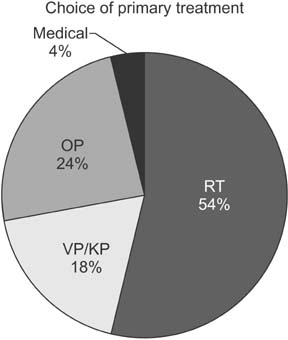
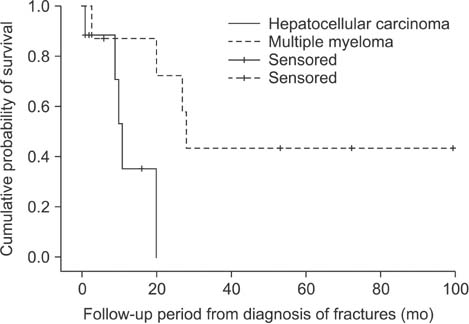
The mean age of the patients was 62.3 years. Hepatocellular carcinoma was the most common cancer of primary origin (n = 9), followed by multiple myeloma (n = 8). RT was the most common primary choice of treatment (n = 29, 53.7%), followed by OP (n = 13, 24.1%), and VP or KP (n = 10, 18.5%). Only 13 of 29 RT cases and 7 of 13 OP cases demonstrated a fair or good response. The mean survival time following detection of pathological spinal fractures was 11.1 months for 29 patients, who died during the study period.
CONCLUSIONS
RT was the most common primary choice of treatment for metastatic pathological fractures of the spine. However, the response rate was suboptimal. Although OP should be considered for the relief of mechanical back pain or neurologic symptoms, care should be taken in determining the surgical indication. VP or KP could be considered for short-term control of localized pain, although the number of cases was too small to confirm the conclusion. It is difficult to determine the superiority of the treatment modalities, hence, a common guideline for the diagnosis and treatment of metastatic pathological fractures of the spine is required.
MeSH Terms
Figure
Reference
-
1. Lee CS, Jung CH. Metastatic spinal tumor. Asian Spine J. 2012; 6(1):71–87.
Article2. Savage P, Sharkey R, Kua T, et al. Malignant spinal cord compression: NICE guidance, improvements and challenges. QJM. 2014; 107(4):277–282.
Article3. L'esperance S, Vincent F, Gaudreault M, et al. Treatment of metastatic spinal cord compression: cepo review and clinical recommendations. Curr Oncol. 2012; 19(6):e478–e490.4. Ha KY, Min CK, Seo JY, et al. Bone cement augmentation procedures for spinal pathologic fractures by multiple myeloma. J Korean Med Sci. 2015; 30(1):88–94.
Article5. Schuster JM, Grady MS. Medical management and adjuvant therapies in spinal metastatic disease. Neurosurg Focus. 2001; 11(6):e3.
Article6. Lim BS, Chang UK, Youn SM. Clinical outcomes after percutaneous vertebroplasty for pathologic compression fractures in osteolytic metastatic spinal disease. J Korean Neurosurg Soc. 2009; 45(6):369–374.
Article7. Chong S, Shin SH, Yoo H, et al. Single-stage posterior decompression and stabilization for metastasis of the thoracic spine: prognostic factors for functional outcome and patients' survival. Spine J. 2012; 12(12):1083–1092.
Article8. Hirabayashi H, Ebara S, Kinoshita T, et al. Clinical outcome and survival after palliative surgery for spinal metastases: palliative surgery in spinal metastases. Cancer. 2003; 97(2):476–484.
Article9. Ibrahim A, Crockard A, Antonietti P, et al. Does spinal surgery improve the quality of life for those with extradural (spinal) osseous metastases? An international multicenter prospective observational study of 223 patients: invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2007. J Neurosurg Spine. 2008; 8(3):271–278.
Article10. Yamashita T, Aota Y, Kushida K, et al. Changes in physical function after palliative surgery for metastatic spinal tumor: association of the revised Tokuhashi score with neurologic recovery. Spine (Phila Pa 1976). 2008; 33(21):2341–2346.
Article11. Kwon YM, Kim KS, Kuh SU, Chin DK, Jin BH, Cho YE. Survival rate and neurological outcome after operation for advanced spinal metastasis (Tomita's classification > or = type 4). Yonsei Med J. 2009; 50(5):689–696.
Article12. Fujibayashi S, Neo M, Miyaki K, Nakayama T, Nakamura T. The value of palliative surgery for metastatic spinal disease: satisfaction of patients and their families. Spine J. 2010; 10(1):42–49.
Article13. Dea N, Versteeg A, Fisher C, et al. Adverse events in emergency oncological spine surgery: a prospective analysis. J Neurosurg Spine. 2014; 21(5):698–703.
Article14. Rao PJ, Thayaparan GK, Fairhall JM, Mobbs RJ. Minimally invasive percutaneous fixation techniques for metastatic spinal disease. Orthop Surg. 2014; 6(3):187–195.
Article15. Kim CH, Chung CK, Sohn S, Lee S, Park SB. Less invasive palliative surgery for spinal metastases. J Surg Oncol. 2013; 108(7):499–503.
Article16. Lau D, Leach MR, La Marca F, Park P. Independent predictors of survival and the impact of repeat surgery in patients undergoing surgical treatment of spinal metastasis. J Neurosurg Spine. 2012; 17(6):565–576.
Article17. Hunter GK, Balagamwala EH, Koyfman SA, et al. The efficacy of external beam radiotherapy and stereotactic body radiotherapy for painful spinal metastases from renal cell carcinoma. Pract Radiat Oncol. 2012; 2(4):e95–e100.
Article18. Wu JS, Wong RK, Lloyd NS, et al. Radiotherapy fractionation for the palliation of uncomplicated painful bone metastases: an evidence-based practice guideline. BMC Cancer. 2004; 4:71.19. Schlampp I, Rieken S, Habermehl D, et al. Stability of spinal bone metastases in breast cancer after radiotherapy: a retrospective analysis of 157 cases. Strahlenther Onkol. 2014; 190(9):792–797.
Article20. Bate BG, Khan NR, Kimball BY, Gabrick K, Weaver J. Stereotactic radiosurgery for spinal metastases with or without separation surgery. J Neurosurg Spine. 2015; 22(4):409–415.
Article21. Lee S, Chun M. Pain relief by Cyberknife radiosurgery for spinal metastasis. Tumori. 2012; 98(2):238–242.
Article22. Farrokhi M, Nouraei H, Kiani A. The efficacy of percutaneous vertebroplasty in pain relief in patients with pathological vertebral fractures due to metastatic spinal tumors. Iran Red Crescent Med J. 2012; 14(9):523–530.23. Cheung G, Chow E, Holden L, et al. Percutaneous vertebroplasty in patients with intractable pain from osteoporotic or metastatic fractures: a prospective study using quality-of-life assessment. Can Assoc Radiol J. 2006; 57(1):13–21.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of CRP in Spinal Compression Fractures: Simple vs Malignant metastatic disease
- Thoracolumbar spine fracture patterns, etiologies, and treatment modalities in Jordan
- Current Trend in Metastatic Bone Tumor Treatment
- Metastatic Spinal Tumor
- Benign compression fractures of the spine: signal patterns