J Korean Med Assoc.
2006 Dec;49(12):1097-1109. 10.5124/jkma.2006.49.12.1097.
Current Trend in Metastatic Bone Tumor Treatment
- Affiliations
-
- 1Department of Orthopaedic Surgery, Kyung Hee University College of Medicine, Korea. cshan1129@yahoo.co.kr
- KMID: 2184740
- DOI: http://doi.org/10.5124/jkma.2006.49.12.1097
Abstract
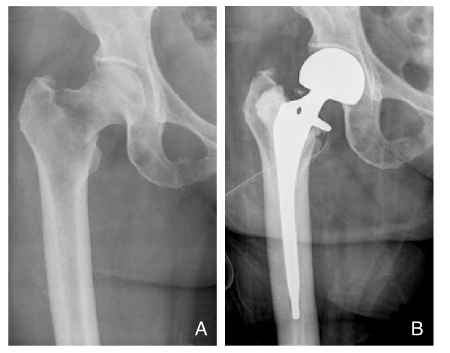
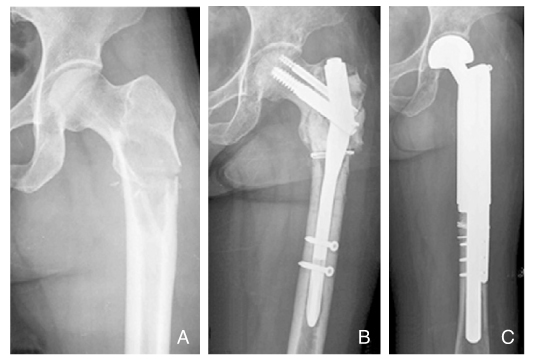
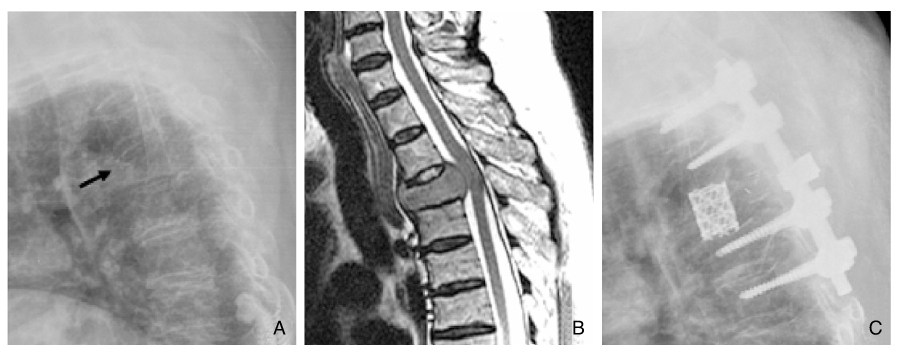
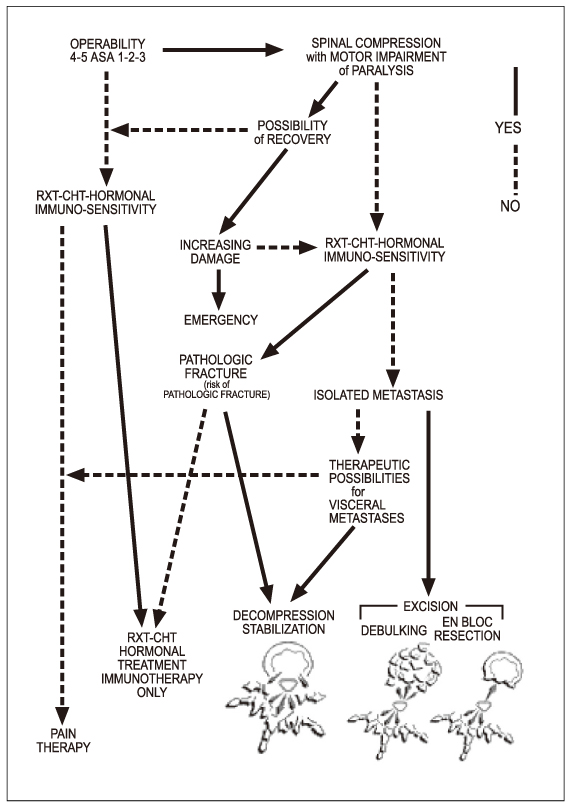
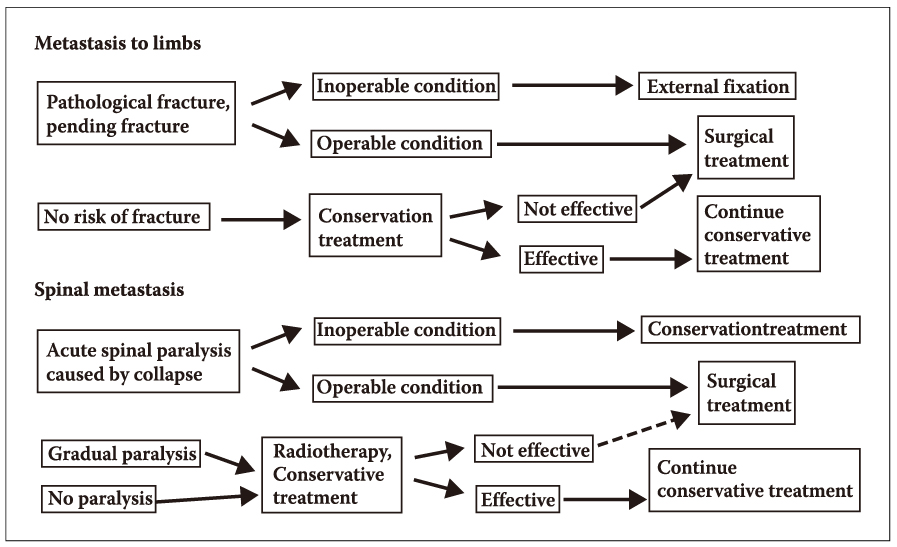
- Metastatic bone tumor is a clinical challenge to most orthopaedic surgeons, and physicians. The bone lesions present pain, can progress to pathologic fractures, and cause neurologic deficits. The adequate treatment for the lesions can mean the difference between good and poor quality of life during their remaining time. The goals of the treatment are relief of pain, preservation of function, and maintenance of independence. In orthopaedic field, the goals include prophylactic fixation of metastatic deposits when there is a risk of fracture, stabilization or reconstruction after pathological fracture, and decompression the spinal cord and nerve roots and/or stabilization the spine. To achieve the goals, we should understand the evaluation methods, a pathogenesis of metastasis and the characters of the specific metastatic site. Finally we should have a knowledge about the treatment strategy and understand what the indications of operative treatment are and which conservative managements is correct for the metastatic bone lesions. It is important to consider the type of primary cancer, location of metastasis, extent of disease, expected patient life span, comorbidities, and level of pain when making treatment recommendations. New discoveries and modifications of existing treatments such as percutaneous stabilization of spinal compression fractures and the use of bisphosphonates may decrease the need for invasive surgical management of metastatic bone lesions in the future. Metastatic bone disease should be approached systematically by multidisciplinary team that has various treatment options, and then quality of life of the patients can be improved during their remaining life span. All the doctors participating in the treatment should try to do their best to get an optimal goal, even though the patients should be informed clearly that the treatments may not be curative.
Keyword
MeSH Terms
Figure
Reference
-
1. Dahlin DC. Bone Tumors: General Aspects and Data on 6,221 Cases. 1978. 3rd ed. Springfield, IL: Charles C Thomas.2. Jemal A, Thomas A, Murray T, Thun M. Cancer statistics, 2002. CA cancer J Clin. 2002. 52:23–47.
Article3. Frassica FJ, Gitelis S, Sim FH. Metastatic bone disease: General principles, pathophysiology, evaluation, and biopsy. Instr Course Lect. 1992. 41:293–300.4. Rougraff BT, Kneisl JS, Simon MA. Skeletal metastases of unknown origin: A prospective study of a diagnotic strategy. J bone Joint Surg Am. 1993. 75:1276–1281.
Article5. Paget S. The distribution of secondary growths in cancer of the breast. Lancet. 1889. 1:571–573.
Article6. Ewing J, editor. Metastasis, in Neoplastic Diseases: A Treatise on Tumor. 1928. 3rd ed. Philadelphia: WB Saunders;77–89.7. Canale ST. Campbell's operative orthopaedics. 2003. 10th ed. Mosby: 848.8. Clohisy DR, Palkert D, Ramnaraine ML, Pekurovsky I, Oursler MJ. Human breast cancer induces osteoclast activation and increases the number of osteoclast at sites of tumor osteolysis. J Orthop Res. 1996. 14:396–402.9. Beals RK, Lawton GD, Snell WE. Prophylactic internal fixation of the femur in metastatic breast cancer. Cancer. 1971. 28:1350–1354.
Article10. Mirels H. Metastatic disease in long bones: A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop. 1989. 249:256–264.
Article11. Katzer A, Meenen NM, Grabbe F, Reuger JM. Surgery of skeletal metastases. Arch Orthop Trauma Surg. 2002. 122:251–258.
Article12. Redmond BJ, Biermann JS, Blasier RB. Interlocking intramedullary nailing of pathological fractures of the shaft of the humerus. J Bone Joint Surg Am. 1996. 78:891–896.
Article13. Damron TA, Sim FH, Shives TC, An KN, Rock MG, Pritchard DJ. Intercalary spacers in the treatment of segmentally destructive diaphyseal humeral lesions in disseminated malignancies. Clin Othop. 1996. 324:233–243.
Article14. Dijkstra S, Stapert J, Boxma H, Wiggers T. Treatment of pathological fractures of the humeral shaft due to bone metastases: A comparison of intramedullay locking nail and plate osteosynthesis with adjunctive bone cement. Eur J Surg Oncol. 1996. 22:621–626.
Article15. Harrington KD. The management of acetabular insufficiency secondary to metastatic malignant disease. J Bone Joint Surg Am. 1981. 63:653–664.
Article16. Marco RA, Sheth DS, Boland PJ, et al. Functional and oncological outcome of acetabular reconstruction for the treatment of metastatic disease. J Bone Joint Surg Am. 2000. 82:642–651.
Article17. Vena VE, Hsu J, Rosier RN, O'Keefe RJ. Pelvic reconstruction for severe periacetabular metastatic disease. Clin Orthop. 1999. 362:171–180.
Article18. Yazawa Y, Frassica FJ, Chao EY, Pritchard DJ, Sim FH, Shives TC. Metastatic bone disease: A study of the surgical treatment of 166 pathologic humeral and femoral fractures. Clin Orthop. 1990. 251:213–219.19. Lane JM, Sculco TP, Zolan S. Treatment of pathological fractures of the hip by endoprosthetic replacement. J Bone Joint Surg Am. 1980. 62:954–959.
Article20. Papagelopoulos PJ, Galanis EC, Greipp PR, Sim FH. Prosthetic hip replacement for pathologic or impending pathologic fractures in myeloma. Clin Orthop. 1997. 341:192–205.
Article21. Behr JT, Dobozi WR, Badrinath K. The treatment of pathologic and impending pathologic fractures of the proximal femur in the elderly. Clin Orthop. 1985. 198:173–178.
Article22. Ward WG, Spang J, Howe D, Gordan S. Femoral recon nails for metastatic disease: Indications, technique, and results. Am J Orthop. 2000. 29:S9. 34–42.23. Weikert DR, Schwartz HS. Intramedullary nailing for impending pathological subtrochanteric fractures. J Bone Joint Surg Br. 1991. 73:668–670.
Article24. Favorito PJ, McGrath BE. Impending or completed pathologic femur fracruters treated with intramedullary hip screws. Orthopedics. 2001. 24:359–363.
Article25. Sim FH, Chao EY. Hip salvage by proximal femoral replacement. J Bone Joint Surg Am. 1981. 63:1228–1239.
Article26. Healey JH, Lane JM. Treatment of pathologic fractures of the distal femur with the Zickel supracondylar nail. Clin Orthop. 1990. 250:216–220.
Article27. De Geeter K, Reynders P, Samson I, Broos PL. Metastatic fractures of the tibia. Acta Orthop Belg. 2001. 67:54–59.28. Hattrup SJ, Amadio PC, Sim FH, Lombardi RM. Metastatic tumors of the foot and ankle. Foot Ankle. 1988. 8:243–247.
Article29. Boland PJ, Lane JM, Sundaresan N. Metastatic disease of the spine. Clin Orthop. 1982. 169:95–102.
Article30. Suen KC, Lau LL, Yermakov V. Cancer and old age. An autopsy study of 3,535 patients over 65 years old. Cancer. 1974. 33:1164–1168.
Article31. Galasko CS, Sylvester BS. Back pain in patients treated for malignant tumours. Clin Oncol. 1978. 4:273–283.32. Gilbert RW, Kim JH, Posner JB. Epidural spinal cord compression from metastatic tumor: Diagnosis and treatment. Ann Neurol. 1978. 3:40–51.
Article33. Weill A, Chiras J, Simon JM, Rose M, Sola-Martinez T, Enkaoua E. Spinal metastases: Indications for and results of percutaneous injection of acrylic surgical cement. Radiology. 1996. 199:241–247.
Article34. Harrington KD. Metastatic disease of the spine. J Bone Joint Surg Am. 1986. 68:1110–1115.
Article35. Arcangeli G, Micheli A, Arcangeli F, et al. The responsiveness of bone metastases to radiotherapy: The effect of site, histology and radiation dose on pain relief. Radiolther Oncol. 1989. 14:95–101.
Article36. Coleman RE. Management of bone metastases. Oncologist. 2000. 5:463–470.
Article37. Crawford ED, Eisenberger MA, McLeod DG, et al. A controlled trial of leuprolide with and without flutamide in prostatic carcinoma. N Engl J Med. 1989. 321:419–424.
Article38. Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T. Surgical strategy for spinal metastases. Spine. 2000. 01. 26:298–306.
Article