J Korean Ophthalmol Soc.
2016 Nov;57(11):1731-1737. 10.3341/jkos.2016.57.11.1731.
Short-term Effectiveness of Intravitreal Triamcinolone Injection for Refractory Macular Edema Secondary to Branch Retinal Vein Occlusion
- Affiliations
-
- 1Department of Ophthalmology, Yonsei University College of Medicine, Seoul, Korea.
- 2Department of Ophthalmology, National Health Insurance Service Ilsan Hospital, Goyang, Korea. Docchoi73@hanmail.net
- KMID: 2357728
- DOI: http://doi.org/10.3341/jkos.2016.57.11.1731
Abstract
- PURPOSE
To evaluate the short-term efficacy of intravitreal triamcinolone (IVTA) injection for the treatment of macular edema secondary to branch retinal vein occlusion (BRVO) refractory to intravitreal bevacizumab injections.
METHODS
This retrospective, observational study included 23 eyes of 23 patients with macular edema secondary to BRVO. The patients with macular edema unresponsive to 2 or more consecutive monthly intravitreal bevacizumab injections were treated with IVTA. Best-corrected visual acuity (BCVA) and central foveal thickness (CFT) based on optical coherence tomography were evaluated before IVTA and 1 month and 3 months after IVTA injections.
RESULTS
All patients were previously treated with 3.4 ± 1.2 intravitreal bevacizumab injections. The IVTA injection was performed at 4.3 ± 1.7 weeks after the last bevacizumab injection. The logarithm of the minimal angle of resolution (log MAR) BCVA was also decreased from 0.61 ± 0.45 to 0.52 ± 0.35 after 1 month and to 0.58 ± 0.37 after 3 months of IVTA, although without statistical significance (p = 0.114 and 0.412, respectively). Eight eyes (34.8%) showed more than 3 lines improvement of BCVA and 4 eyes (17.4%) showed stable BCVA increasing 2 lines or less. CFT was significantly improved from 512 ± 166 µm to 310 ± 139 µm after 1 month and to 324 ± 159 µm after 3 months of IVTA injections (p = 0.014 and 0.031, respectively).
CONCLUSIONS
IVTA was beneficial in some patients with macular edema secondary to BRVO refractory to intravitreal bevacizumab therapy. This study indicates that IVTA could be considered as a treatment option for refractory macular edema associated with BRVO.
Keyword
MeSH Terms
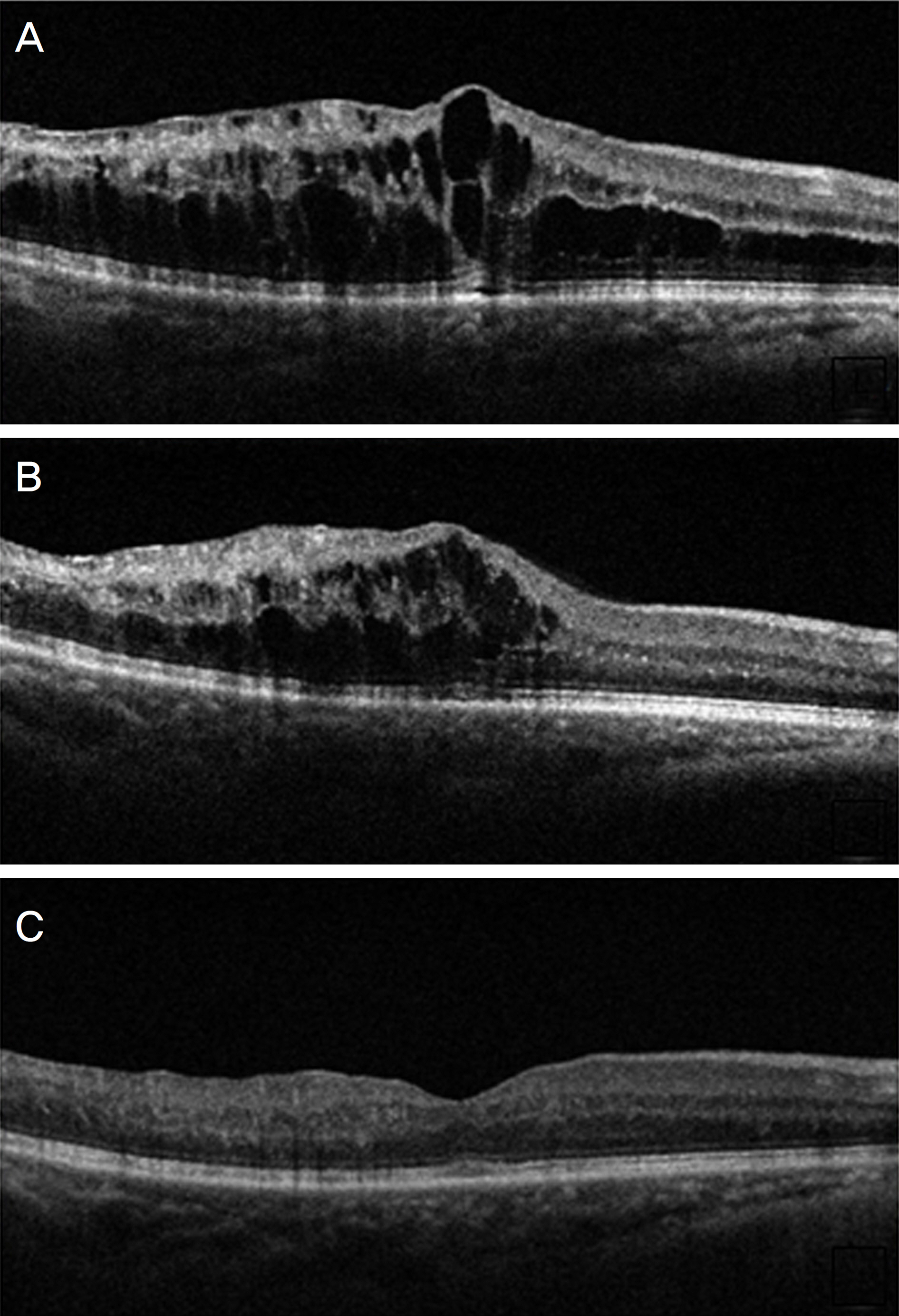
Figure
Cited by 2 articles
-
A Comparison of Three Intravitreal Modalities of Branch Retinal Vein Occlusion Macular Edema
Han Song, Hee Jun Song, Ji Ho Yang, Do Gyun Kim
J Korean Ophthalmol Soc. 2018;59(9):834-841. doi: 10.3341/jkos.2018.59.9.834.Intraocular Pressure: Intravitreal Preservative-free Triamcinolone Injection in Diabetic Macular Edema and Branch Retinal Vein Occlusion
Chan Ho Lee, Young Seung Seo
J Korean Ophthalmol Soc. 2020;61(2):167-174. doi: 10.3341/jkos.2020.61.2.167.
Reference
-
References
1. Rogers SL, McIntosh RL, Lim L, et al. Natural history of branch retinal vein occlusion: an evidence-based systematic review. Ophthalmology. 2010; 117:1094–101.e5.
Article2. Argon laser photocoagulation for macular edema in branch vein occlusion. The Branch Vein Occlusion Study Group. Am J Ophthalmol. 1984; 98:271–82.3. Cekiç O, Chang S, Tseng JJ, et al. Intravitreal triamcinolone abdominal for treatment of macular edema secondary to branch retinal vein occlusion. Retina. 2005; 25:851–5.4. Arnarsson A, Stefánsson E. Laser treatment and the mechanism of edema reduction in branch retinal vein occlusion. Invest Ophthalmol Vis Sci. 2000; 41:877–9.5. Rabena MD, Pieramici DJ, Castellarin AA, et al. Intravitreal abdominal (Avastin) in the treatment of macular edema secondary to branch retinal vein occlusion. Retina. 2007; 27:419–25.6. Guthoff R, Meigen T, Hennemann K, Schrader W. Comparison of bevacizumab and triamcinolone for treatment of macular edema secondary to branch retinal vein occlusion in a pair-matched analysis. Ophthalmologica. 2010; 224:319–24.
Article7. Ding X, Li J, Hu X, et al. Prospective study of intravitreal abdominal acetonide versus bevacizumab for macular edema abdominal to central retinal vein occlusion. Retina. 2011; 31:838–45.8. Demir M, Dirim B, Acar Z, et al. Comparison of the effects of abdominal bevacizumab and triamcinolone acetonide in the treatment of macular edema secondary to central retinal vein occlusion. Indian J Ophthalmol. 2014; 62:279–83.9. Campa C, Alivernini G, Bolletta E, et al. Anti-VEGF therapy for retinal vein occlusions. Curr Drug Targets. 2016; 17:328–36.
Article10. Lim HB, Kim MS, Jo YJ, Kim JY. Prediction of retinal ischemia in branch retinal vein occlusion: spectraldomain optical coherence tomography study. Invest Ophthalmol Vis Sci. 2015; 56:6622–9.
Article11. Campochiaro PA, Bhisitkul RB, Shapiro H, Rubio RG. Vascular endothelial growth factor promotes progressive retinal non-perfusion in patients with retinal vein occlusion. Ophthalmology. 2013; 120:795–802.
Article12. Park SP, Ahn JK, Mun GH. Aqueous vascular endothelial growth factor levels are associated with serous macular detachment abdominal to branch retinal vein occlusion. Retina. 2010; 30:281–6.13. Koss MJ, Naser H, Sener A, et al. Combination therapy in diabetic macular oedema and retinal vein occlusion-past and present. Acta Ophthalmol. 2012; 90:580–9.14. Noma H, Funatsu H, Yamasaki M, et al. Aqueous humour levels of cytokines are correlated to vitreous levels and severity of macular oedema in branch retinal vein occlusion. Eye (Lond). 2008; 22:42–8.
Article15. Fonollosa A, Garcia-Arumi J, Santos E, et al. Vitreous levels of in-terleukine-8 and monocyte chemoattractant protein-1 in macular oedema with branch retinal vein occlusion. Eye (Lond). 2010; 24:1284–90.
Article16. Sohn HJ, Han DH, Lee DY, Nam DH. Changes in aqueous abdominal after intravitreal triamcinolone versus bevacizumab for abdominal oedema in branch retinal vein occlusion. Acta Ophthalmol. 2014; 92:e217–24.17. Shroff D, Mehta DK, Arora R, et al. Natural history of macular abdominal in recent-onset branch retinal vein occlusion: an optical abdominal tomography study. Int Ophthalmol. 2008; 28:261–8.18. Kim M, Kim Y, Lee SJ. Comparison of aqueous concentrations of angiogenic and in fl ammatory cytokines based on optical abdominal tomography patterns of diabetic macular edema. Indian J Ophthalmol. 2015; 63:312–7.19. Noma H, Funatsu H, Mimura T, Shimada K. Comparison of the abdominal of intravitreal triamcinolone acetonide for cystoid macular edema with versus without serous retinal detachment in branch abdominal vein occlusion: influence on macular sensitivity and morphology. BMC Ophthalmol. 2012; 12:39.
Article20. Qi HP, Bi S, Wei SQ, et al. Intravitreal versus subtenon abdominal acetonide injection for diabetic macular edema: a abdominalatic review and meta-analysis. Curr Eye Res. 2012; 37:1136–47.21. Choudhry S, Ghosh S. Intravitreal and posterior subtenon abdominal acetonide in idiopathic bilateral uveitic macular oedema. Clin Experiment Ophthalmol. 2007; 35:713–8.22. Cardillo JA, Melo LA Jr, Costa RA, et al. Comparison of abdominal versus posterior abdominal's capsule injection of triamcinolone acetonide for diffuse diabetic macular edema. Ophthalmology. 2005; 112:1557–63.23. Hirose M, Matsumiya W, Honda S, Nakamura M. Efficacy and abdominal prognostic factors of intravitreal bevacizumab as needed for macular edema secondary to central retinal vein occlusion. Clin Ophthalmol. 2014; 8:2301–5.24. Jaissle GB, Szurman P, Feltgen N, et al. Predictive factors for functional improvement after intravitreal bevacizumab therapy for macular edema due to branch retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2011; 249:183–92.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effectiveness of Intravitreal Triamcinolone Injection for the Treatment of Macular Edema
- Intravitreal Triamcinolone Versus Bevacizumab for Treatment of Macular Edema Secondary to Branch Retinal Vein Occlusion
- Effectiveness of Intravitreal Preservative-free Triamcinolone Injection for Refractory Macular Edema Secondary to Retinal Vein Occlusion
- Combined Therapy of Intravitreal Bevacizumab and Posterior Subtenon Triamcinolone Injection in Macular Edema with Branch Retinal Vein Occlusion
- Combined Low Dose Bevacizumab-triamcinolone versus Bevacizumab Single Intravitreal Injection for Branch Retinal Vein Occlusion