Ann Rehabil Med.
2016 Aug;40(4):592-599. 10.5535/arm.2016.40.4.592.
Botulinum Toxin A Injection into the Subscapularis Muscle to Treat Intractable Hemiplegic Shoulder Pain
- Affiliations
-
- 1Department of Rehabilitation Medicine, National Rehabilitation Center, Seoul, Korea. bbora1114@naver.com
- KMID: 2356644
- DOI: http://doi.org/10.5535/arm.2016.40.4.592
Abstract
OBJECTIVE
To evaluate the beneficial effect of botulinum toxin A (Botox) injection into the subscapularis muscle on intractable hemiplegic shoulder pain.
METHODS
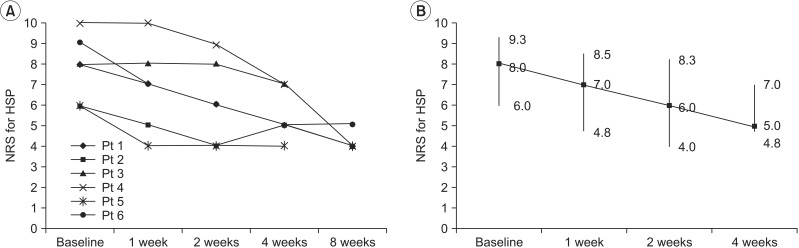
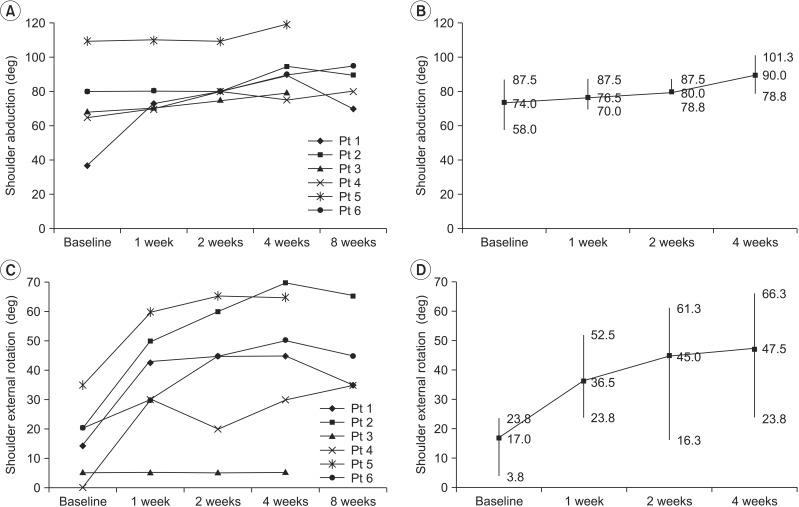
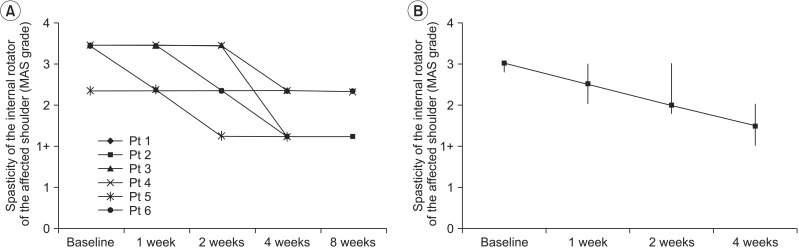
Six stroke patients with intractable hemiplegic shoulder pain were included. Botulinum toxin A was injected into the subscapularis muscle. Intractable hemiplegic shoulder pain was evaluated using an 11-point numerical rating scale. Pain-free range of motion was assessed for shoulder abduction and external rotation. The spasticity of the shoulder internal rotator was measured using the modified Ashworth scale. Assessments were carried out at baseline and at 1, 2, 4, and, if possible, 8 weeks.
RESULTS
Intractable hemiplegic shoulder pain was improved (p=0.004) after botulinum toxin injection into the subscapularis muscle. Restricted shoulder abduction (p=0.003), external rotation (p=0.005), and spasticity of the shoulder internal rotator (p=0.005) were also improved. Improved hemiplegic shoulder pain was correlated with improved shoulder abduction (r=-1.0, p<0.001), external rotation (r=-1.0, p<0.001), and spasticity of the internal rotator (r=1.0, p<0.001).
CONCLUSION
Botulinum toxin A injection into the subscapularis muscle appears to be valuable in the management of intractable hemiplegic shoulder pain.
Keyword
MeSH Terms
Figure
Reference
-
1. Adey-Wakeling Z, Arima H, Crotty M, Leyden J, Kleinig T, Anderson CS, et al. Incidence and associations of hemiplegic shoulder pain poststroke: prospective population-based study. Arch Phys Med Rehabil. 2015; 96:241–247. PMID: 25264111.2. Aras MD, Gokkaya NK, Comert D, Kaya A, Cakci A. Shoulder pain in hemiplegia: results from a national rehabilitation hospital in Turkey. Am J Phys Med Rehabil. 2004; 83:713–719. PMID: 15314536.3. Lo SF, Chen SY, Lin HC, Jim YF, Meng NH, Kao MJ. Arthrographic and clinical findings in patients with hemiplegic shoulder pain. Arch Phys Med Rehabil. 2003; 84:1786–1791. PMID: 14669184.4. Tavora DG, Gama RL, Bomfim RC, Nakayama M, Silva CE. MRI findings in the painful hemiplegic shoulder. Clin Radiol. 2010; 65:789–794. PMID: 20797464.5. Murie-Fernandez M, Carmona Iragui M, Gnanakumar V, Meyer M, Foley N, Teasell R. Painful hemiplegic shoulder in stroke patients: causes and management. Neurologia. 2012; 27:234–244. PMID: 21514698.6. Snels IA, Beckerman H, Lankhorst GJ, Bouter LM. Treatment of hemiplegic shoulder pain in the Netherlands: results of a national survey. Clin Rehabil. 2000; 14:20–27. PMID: 10688341.
Article7. Gamble GE, Barberan E, Laasch HU, Bowsher D, Tyrrell PJ, Jones AK. Poststroke shoulder pain: a prospective study of the association and risk factors in 152 patients from a consecutive cohort of 205 patients presenting with stroke. Eur J Pain. 2002; 6:467–474. PMID: 12413435.
Article8. Singh JA, Mahowald ML, Noorbaloochi S. Intra-articular botulinum toxin A for refractory shoulder pain: a randomized, double-blinded, placebo-controlled trial. Transl Res. 2009; 153:205–216. PMID: 19375681.
Article9. Roosink M, Renzenbrink GJ, Buitenweg JR, Van Dongen RT, Geurts AC, IJzerman MJ. Persistent shoulder pain in the first 6 months after stroke: results of a prospective cohort study. Arch Phys Med Rehabil. 2011; 92:1139–1145. PMID: 21704795.
Article10. Jankovic J. Botulinum toxin in clinical practice. J Neurol Neurosurg Psychiatry. 2004; 75:951–957. PMID: 15201348.
Article11. Lee HS, Oh HS, Shin JH. Paroxysmal autonomic instability with dystonia managed using chemodenervation including alcohol neurolysis and botulinum toxin type a injection: a case report. Ann Rehabil Med. 2015; 39:308–312. PMID: 25932429.
Article12. Yelnik AP, Colle FM, Bonan IV, Vicaut E. Treatment of shoulder pain in spastic hemiplegia by reducing spasticity of the subscapular muscle: a randomised, double blind, placebo controlled study of botulinum toxin A. J Neurol Neurosurg Psychiatry. 2007; 78:845–848. PMID: 17088333.
Article13. Jabbari B. Botulinum neurotoxins in the treatment of refractory pain. Nat Clin Pract Neurol. 2008; 4:676–685. PMID: 19043424.
Article14. Wissel J, Muller J, Dressnandt J, Heinen F, Naumann M, Topka H, et al. Management of spasticity associated pain with botulinum toxin A. J Pain Symptom Manage. 2000; 20:44–49. PMID: 10946168.
Article15. Wu T, Fu Y, Song HX, Ye Y, Dong Y, Li JH. Effectiveness of botulinum toxin for shoulder pain treatment : a systematic review and meta-analysis. Arch Phys Med Rehabil. 2015; 96:2214–2220. PMID: 26189200.16. de Boer KS, Arwert HJ, de Groot JH, Meskers CG, Mishre AD, Arendzen JH. Shoulder pain and external rotation in spastic hemiplegia do not improve by injection of botulinum toxin A into the subscapular muscle. J Neurol Neurosurg Psychiatry. 2008; 79:581–583. PMID: 18408090.
Article17. Lim JY, Koh JH, Paik NJ. Intramuscular botulinum toxin-A reduces hemiplegic shoulder pain: a randomized, double-blind, comparative study versus intraarticular triamcinolone acetonide. Stroke. 2008; 39:126–131. PMID: 18048857.18. Harden RN, Bruehl S, Stanton-Hicks M, Wilson PR. Proposed new diagnostic criteria for complex regional pain syndrome. Pain Med. 2007; 8:326–331. PMID: 17610454.
Article19. Klit H, Finnerup NB, Jensen TS. Central post-stroke pain: clinical characteristics, pathophysiology, and management. Lancet Neurol. 2009; 8:857–868. PMID: 19679277.
Article20. Yelnik AP, Colle FM, Bonan IV. Treatment of pain and limited movement of the shoulder in hemiplegic patients with botulinum toxin A in the subscapular muscle. Eur Neurol. 2003; 50:91–93. PMID: 12944713.
Article21. Rha DW, Han SH, Kim HJ, Won SY, Lee SC. Ultrasound-guided lateral approach for needle insertion into the subscapularis for treatment of spasticity. Arch Phys Med Rehabil. 2012; 93:1147–1152. PMID: 22503934.
Article22. Chang YW, Hughes RE, Su FC, Itoi E, An KN. Prediction of muscle force involved in shoulder internal rotation. J Shoulder Elbow Surg. 2000; 9:188–195. PMID: 10888162.
Article23. Hecht JS. Subscapular nerve block in the painful hemiplegic shoulder. Arch Phys Med Rehabil. 1992; 73:1036–1039. PMID: 1444768.24. Braun RM, West F, Mooney V, Nickel VL, Roper B, Caldwell C. Surgical treatment of the painful shoulder contracture in the stroke patient. J Bone Joint Surg Am. 1971; 53:1307–1312. PMID: 5114694.
Article25. Mense S. Neurobiological basis for the use of botulinum toxin in pain therapy. J Neurol. 2004; 251(Suppl 1):I1–I7. PMID: 14991335.
Article26. Jabbari B, Machado D. Treatment of refractory pain with botulinum toxins: an evidence-based review. Pain Med. 2011; 12:1594–1606. PMID: 21958302.27. Cosgrove AP, Corry IS, Graham HK. Botulinum toxin in the management of the lower limb in cerebral palsy. Dev Med Child Neurol. 1994; 36:386–396. PMID: 8168657.
Article28. Childers MK, Brashear A, Jozefczyk P, Reding M, Alexander D, Good D, et al. Dose-dependent response to intramuscular botulinum toxin type A for upper-limb spasticity in patients after a stroke. Arch Phys Med Rehabil. 2004; 85:1063–1069. PMID: 15241751.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Application of Botulinum Toxin in Pain Management
- Effects of Intra-Articular Injection and Subscapularis Motor Point Block on Painful Hemiplegic Shoulder
- Gait Improvement after Botulinum Toxin Injection in a Patient with Piriformis Muscle Syndrome
- Botulinum Toxin-Type A in Cervical Myofascial Pain Syndrome: A report of 3 cases
- Botulinum Toxin Injection Therapy for Lingual Dystonia: A Case Report