Cancer Res Treat.
2016 Oct;48(4):1330-1337. 10.4143/crt.2015.463.
Identification of Prognostic Risk Factors for Transient and Persistent Lymphedema after Multimodal Treatment for Breast Cancer
- Affiliations
-
- 1Research Institute and Hospital, National Cancer Center, Goyang, Korea. radiat@snu.ac.kr
- 2Department of Radiation Oncology, Incheon St Mary's Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea.
- 3Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2356235
- DOI: http://doi.org/10.4143/crt.2015.463
Abstract
- PURPOSE
The purpose of this study is to identify risk factors for transient lymphedema (TLE) and persistent lymphedema (PLE) following treatment for breast cancer.
MATERIALS AND METHODS
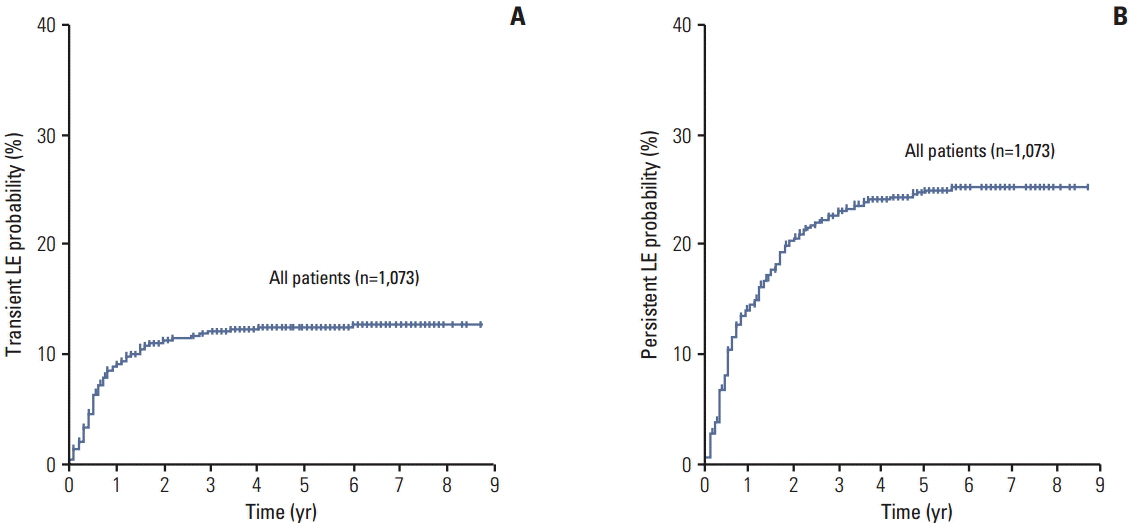
A total of 1,073 patients who underwent curative breast surgery were analyzed. TLE was defined as one episode of arm swelling that had resolved spontaneously by the next follow-up; arm swelling that persisted over two consecutive examinations was considered PLE.
RESULTS
At a median follow-up period of 5.1 years, 370 cases of lymphedema were reported, including 120 TLE (11.2%) and 250 PLE (23.3%). Initial grade 1 swelling was observed in 351 patients, of which 120 were limited to TLE (34%), while the other 231 progressed to PLE (66%). All initial swelling observed in TLE patients was classified as grade 1. In multivariate analysis, chemotherapy with taxane and supraclavicular radiation therapy (SCRT) were associated with development of TLE, whereas SCRT, stage III cancer and chemotherapy with taxane were identified as risk factors for PLE (p < 0.05). The estimated incidence of TLE among initial grade 1 patients was calculated using up to three treatment-related risk factors (number of dissected axillary lymph nodes, SCRT, and taxane chemotherapy). The approximate ratios of TLE and PLE based on the number of risk factors were 7:1 (no factor), 1:1 (one factor), 1:2 (two factors), and 1:3 (three factors).
CONCLUSION
One-third of initial swelling events were transient, whereas the other two-thirds of patients experienced PLE. Estimation of TLE and PLE based on known treatment factors could facilitate prediction of this life-long complication.
MeSH Terms
Figure
Reference
-
References
1. DiSipio T, Rye S, Newman B, Hayes S. Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol. 2013; 14:500–15.
Article2. Cemal Y, Pusic A, Mehrara BJ. Preventative measures for lymphedema: separating fact from fiction. J Am Coll Surg. 2011; 213:543–51.
Article3. Kim M, Kim SW, Lee SU, Lee NK, Jung SY, Kim TH, et al. A model to estimate the risk of breast cancer-related lymphedema: combinations of treatment-related factors of the number of dissected axillary nodes, adjuvant chemotherapy, and radiation therapy. Int J Radiat Oncol Biol Phys. 2013; 86:498–503.
Article4. Kilbreath SL, Lee MJ, Refshauge KM, Beith JM, Ward LC, Simpson JM, et al. Transient swelling versus lymphoedema in the first year following surgery for breast cancer. Support Care Cancer. 2013; 21:2207–15.
Article5. Tsai RJ, Dennis LK, Lynch CF, Snetselaar LG, Zamba GK, Scott-Conner C. The risk of developing arm lymphedema among breast cancer survivors: a meta-analysis of treatment factors. Ann Surg Oncol. 2009; 16:1959–72.
Article6. Brennan MJ. Lymphedema following the surgical treatment of breast cancer: a review of pathophysiology and treatment. J Pain Symptom Manage. 1992; 7:110–6.
Article7. Park SH, Kim JC, Lee JE, Park IK. Virtual lymph node analysis to evaluate axillary lymph node coverage provided by tangential breast irradiation. Radiat Oncol J. 2015; 33:50–6.
Article8. Jung SY, Shin KH, Kim M, Chung SH, Lee S, Kang HS, et al. Treatment factors affecting breast cancer-related lymphedema after systemic chemotherapy and radiotherapy in stage II/III breast cancer patients. Breast Cancer Res Treat. 2014; 148:91–8.
Article9. Kim M, Park IH, Lee KS, Ro J, Jung SY, Lee S, et al. Breast cancer-related lymphedema after neoadjuvant chemotherapy. Cancer Res Treat. 2015; 47:416–23.
Article10. Gartner R, Jensen MB, Kronborg L, Ewertz M, Kehlet H, Kroman N. Self-reported arm-lymphedema and functional impairment after breast cancer treatment: a nationwide study of prevalence and associated factors. Breast. 2010; 19:506–15.11. Harris SR, Hugi MR, Olivotto IA, Levine M; Steering Committee for Clinical Practice Guidelines for the Care and Treatment of Breast Cancer. Clinical practice guidelines for the care and treatment of breast cancer: 11. Lymphedema. CMAJ. 2001; 164:191–9.12. McLaughlin SA, Wright MJ, Morris KT, Giron GL, Sampson MR, Brockway JP, et al. Prevalence of lymphedema in women with breast cancer 5 years after sentinel lymph node biopsy or axillary dissection: objective measurements. J Clin Oncol. 2008; 26:5213–9.
Article13. Werner RS, McCormick B, Petrek J, Cox L, Cirrincione C, Gray JR, et al. Arm edema in conservatively managed breast cancer: obesity is a major predictive factor. Radiology. 1991; 180:177–84.
Article14. Norman SA, Localio AR, Potashnik SL, Simoes Torpey HA, Kallan MJ, Weber AL, et al. Lymphedema in breast cancer survivors: incidence, degree, time course, treatment, and symptoms. J Clin Oncol. 2009; 27:390–7.
Article15. Lee MJ, Beith J, Ward L, Kilbreath S. Lymphedema following taxane-based chemotherapy in women with early breast cancer. Lymphat Res Biol. 2014; 12:282–8.
Article16. Dominick SA, Madlensky L, Natarajan L, Pierce JP. Risk factors associated with breast cancer-related lymphedema in the WHEL Study. J Cancer Surviv. 2013; 7:115–23.
Article17. Ahmed RL, Schmitz KH, Prizment AE, Folsom AR. Risk factors for lymphedema in breast cancer survivors, the Iowa Women's Health Study. Breast Cancer Res Treat. 2011; 130:981–91.
Article18. Coen JJ, Taghian AG, Kachnic LA, Assaad SI, Powell SN. Risk of lymphedema after regional nodal irradiation with breast conservation therapy. Int J Radiat Oncol Biol Phys. 2003; 55:1209–15.19. Bar Ad V, Cheville A, Solin LJ, Dutta P, Both S, Harris EE. Time course of mild arm lymphedema after breast conservation treatment for early-stage breast cancer. Int J Radiat Oncol Biol Phys. 2010; 76:85–90.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rapid Lymphedema Progression in Breast Cancer Patient with Previous Forearm Fracture
- The Risk Factors of Lymphedema after Breast Cancer Surgery
- Risk Factors for Developing Upper Limb Lymphedema following Breast Cancer Surgery
- A Survey of the Status of Awareness of Lymphedema in Breast Cancer Patients in Busan-Gyeongnam, Korea
- The Risk Factors Associated with Lymphedema after Axillary Dissection for Breast Cancer