Korean Circ J.
2016 Nov;46(6):846-850. 10.4070/kcj.2016.46.6.846.
Long-Term Results of Early Surgery versus Conventional Treatment for Infective Endocarditis Trial
- Affiliations
-
- 1Division of Cardiology, Cardiac Surgery, Infectious Disease, Biostatistics, Asan Medical Center, College of Medicine, University of Ulsan, Seoul, Korea. dhkang@amc.seoul.kr
- 2Cardiovascular Center, Seoul National University Hospital, Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2355462
- DOI: http://doi.org/10.4070/kcj.2016.46.6.846
Abstract
- BACKGROUND AND OBJECTIVES
Compared with conventional treatment, early surgery significantly reduced the composite end point of all-cause death and embolic events during hospitalization, but long-term data in this area are lacking. This study sought to compare long-term outcomes of early surgery with a conventional treatment strategy in patients with infective endocarditis (IE) and large vegetations.
SUBJECTS AND METHODS
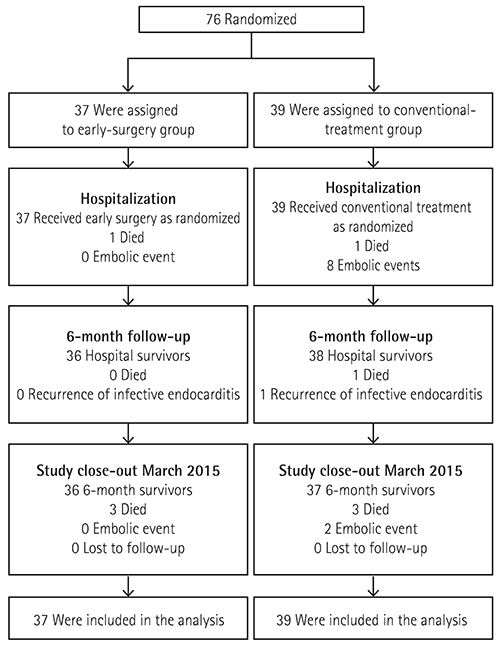
The Early Surgery versus Conventional Treatment in Infective Endocarditis (EASE) trial randomly assigned patients with left-sided IE, severe valve disease and large vegetation to early surgery (37 patients) or conventional treatment groups (39 patients). The pre-specified end points were all-cause death, embolic events, recurrence of IE and repeat hospitalizations due to the development of congestive heart failure occurring during follow-up.
RESULTS
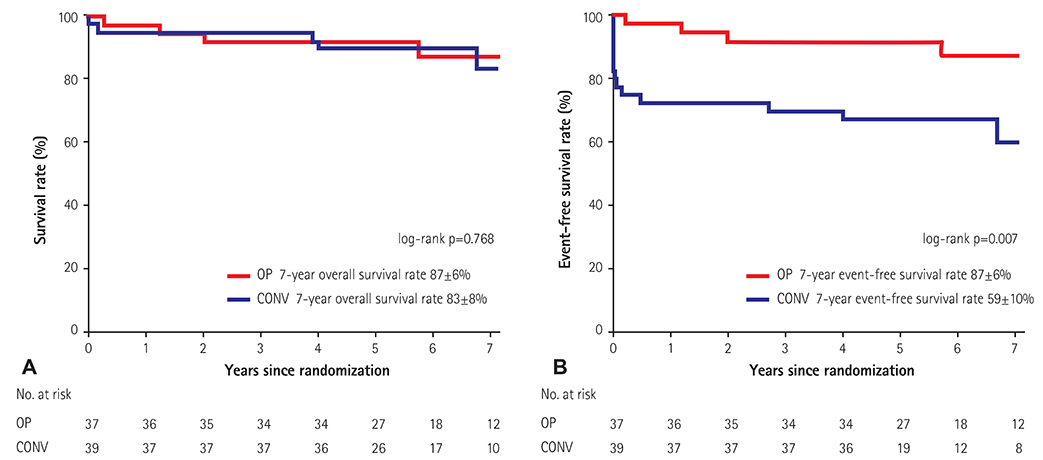
There were no significant differences between the early surgery and the conventional treatment group in all-cause mortality at 4 years (8.1% and 7.7%, respectively; hazard ratio [HR] 1.04; 95% CI, 0.21 to 5.15; p=0.96). The rate of the composite end point of death from any cause, embolic events or recurrence of IE at 4 years was 8.1% in the early surgery group and 30.8% in the conventional treatment group (HR, 0.22; 95% CI, 0.06-0.78; p=0.02). The estimated actuarial rate of end points at 7 years was significantly lower in the early surgery group than in the conventional treatment group (log-rank p=0.007).
CONCLUSION
There was a substantial benefit in having early surgery for patients with IE and large vegetations whose health was sustained up to 7 years, and late clinical outcome after surgery was excellent in survivors of IE. (EASE clinicaltrials.gov identifier: NCT00750373)
MeSH Terms
Figure
Cited by 1 articles
-
Early Surgery in Valvular Heart Disease
Dae-Hee Kim, Duk-Hyun Kang
Korean Circ J. 2018;48(11):964-973. doi: 10.4070/kcj.2018.0308.
Reference
-
1. Murdoch DR, Corey GR, Hoen B, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med. 2009; 169:463–473.2. Mylonakis E, Calderwood SB. Medical progress: infective endocarditis in adults. N Engl J Med. 2001; 345:1318–1330.3. Hoen B, Duval X. Clinical practice. Infective endocarditis. N Engl J Med. 2013; 368:1425–1433.4. Shih CJ, Chu H, Chao PW, et al. Long-term clinical outcome of major adverse cardiac events in survivors of infective endocarditis: a nationwide population-based study. Circulation. 2014; 130:1684–1691.5. Kang DH, Kim YJ, Kim SH, et al. Early surgery versus conventional treatment for infective endocarditis. N Engl J Med. 2012; 366:2466–2473.6. Bannay A, Hoen B, Duval X, et al. The impact of valve surgery on short- and long-term mortality in left-sided infective endocarditis: do differences in methodological approaches explain previous conflicting results? Eur Heart J. 2011; 32:2003–2015.7. Thuny F, Giorgi R, Habachi R, et al. Excess mortality and morbidity in patients surviving infective endocarditis. Am Heart J. 2012; 164:94–101.8. Ternhag A, Cederström A, Törner A, Westling K. A nationwide cohort study of mortality risk and long-term prognosis in infective endocarditis in Sweden. PLos One. 2013; 8:e67519.9. Mokhles MM, Ciampichetti I, Head SJ, Takkenberg JJ, Bogers AJ. Survival of surgically treated infective endocarditis: a comparison with the general Dutch population. Ann Thorac Surg. 2011; 91:1407–1412.10. Li JS, Sexton DJ, Mick N, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000; 30:633–638.11. Bonow RO, Carabello BA, Kanu C, et al. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): developed in collaboration with the Society of Cardiovascular Anesthesiologists: endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. Circulation. 2006; 114:e84–e231.12. Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis: diagnosis, antimicrobial therapy, and management of complications: a statement for healthcare professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, and the Councils on Clinical Cardiology, Stroke, and Cardiovascular Surgery and Anesthesia, American Heart Association: endorsed by the Infectious Diseases Society of America. Circulation. 2005; 111:e394–e434.13. Habib G, Hoen B, Tornos P, et al. Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): the Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC). Eur Heart J. 2009; 30:2369–2413.14. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014; 63:e57–e185.15. Kang DH. Timing of surgery in infective endocarditis. Heart. 2015; 101:1786–1791.16. Freedman B. Equipoise and the ethics of clinical research. N Engl J Med. 1987; 317:141–145.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Active Infective Endocarditis with Vegetation of Right Atrium in Patient with End-stage Renal Disease
- Surgical Management of Infective Endocarditis Complicated by Embolic Stroke: Early versus Delayed Surgery
- Splenic Rupture Complicated by Infective Endocarditis
- Pyogenic Arthritis of the Shoulder in Patient with Infective Endocarditis: A Case Report
- A Case of Infective Endocarditis in Pregnancy