Korean Circ J.
2016 Nov;46(6):768-773. 10.4070/kcj.2016.46.6.768.
Neutrophil Lymphocyte Ratio as a Predictor of Left Ventricular Apical Thrombus in Patients with Myocardial Infarction
- Affiliations
-
- 1Department of Cardiology, Ataturk Training and Research Hospital, Ankara, Turkey. agertem@hotmail.com
- 2Department of Cardiology, Yildirim Beyazit University, Ankara, Turkey.
- KMID: 2355451
- DOI: http://doi.org/10.4070/kcj.2016.46.6.768
Abstract
- BACKGROUND AND OBJECTIVES
In this study, we examined the role of inflammatory parameters in an apical mural thrombus with a reduced ejection fraction due to large anterior myocardial infarction (MI).
SUBJECTS AND METHODS
A total of 103 patients who had suffered from heart failure, 45 of whom had left ventricular apical thrombus (AT) after a large anterior MI, were enrolled in the study. A detailed clinical history was taken of each participant, biochemical inflammatory markers, which were obtained during admission, were analyzed and an echocardiographical and angiographical evaluation of specific parameters were performed.
RESULTS
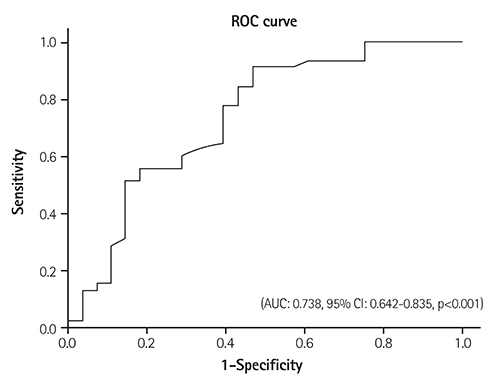
There were no statistically significant differences in terms of age, gender, and history of hypertension, diabetes mellitus, and atrial fibrillation between both groups (p>0.05). Similarly there were no statistically significant differences in terms of biochemical and echocardiographic parameters (p>0.05). However, there were significant differences in terms of neutrophil lymphocyte ratio (p=0.032). After a multivariate regression analysis, neutrophil lymphocyte ratio (NLR) was an independent predictor of thrombus formation (β: 0.296, p=0.024). The NLR >2.74 had a 78% sensivity and 61% specifity in predicting thrombus in patients with a low left ventricular ejection fraction.
CONCLUSION
In this study, neutrophil lymphocyte ratios were significantly higher in patients with apical thrombus.
Keyword
MeSH Terms
Figure
Reference
-
1. Sharma ND, McCullough PA, Philbin EF, et al. Left ventricular thrombus and subsequent thromboembolism in patients with severe systolic dysfunction. Chest. 2000; 117:314–320.2. Schneider C, Bahlmann E, Heuser C, et al. Images in cardiovascular medicine. Unusual biventricular thrombus formation in acute myeloid leukemia and factor V Leiden mutation. Circulation. 2003; 107:e114–e116.3. Thomson SP, Gibbons RJ, Smars PA, et al. Incremental value of the leukocyte differential and the rapid creatine kinase-MB isoenzyme for the early diagnosis of myocardial infarction. Ann Intern Med. 1995; 122:335–341.4. Delewi R, Zijlstra F, Piek JJ. Left ventricular thrombus formation after acute myocardial infarction. Heart. 2012; 98:1743–1749.5. Johannessen KA, Nordrehaug JE, von der Lippe G. Increased occurrence of left ventricular thrombi during early treatment with timolol in patients with acute myocardial infarction. Circulation. 1987; 75:151–155.6. Asinger RW, Mikell FL, Elsperger J, Hodges M. Incidence of leftventricular thrombosis after acute transmural myocardial infarction. Serial evaluation by two-dimensional echocardiography. N Engl J Med. 1981; 305:297–302.7. Visser CA, Kan G, Lie KI, Durrer D. Left ventricular thrombus following acute myocardial infarction: a prospective serial echocardiographic study of 96 patients. Eur Heart J. 1983; 4:333–337.8. Han YC, Yang TH, Kim DI, et al. Neutrophil to Lymphocyte ratio predicts long-term clinical outcomes in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Korean Circ J. 2013; 43:93–99.9. Arruda-Olson AM, Reeder GS, Bell MR, Weston SA, Roger VL. Neutrophilia predicts death and heart failure after myocardial infarction: a community-based study. Circ Cardiovasc Qual Outcomes. 2009; 2:656–662.10. Rudiger A, Burckhardt OA, Harpes P, Müller SA, Follath F. The relative lymphocyte count on hospital admission is a risk factor for longterm mortality in patients with acute heart failure. Am J Emerg Med. 2006; 24:451–454.11. Looney MR, Su X, Van Ziffle JA, Lowell CA, Matthay MA. Neutrophils and their Fc gamma receptors are essential in a mouse model of transfusion-related acute lung injury. J Clin Invest. 2006; 116:1615–1623.12. Rapaport SI, Rao LV. The tissue factor pathway: how it has become a "prima ballerina". Thromb Haemost. 1995; 74:7–17.13. Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification. Eur J Echocardiogr. 2006; 7:79–108.14. Roberts WC, Siegel RJ, McManus BM. Idiopathic dilated cardiomyopathy: analysis of 152 necropsy patients. Am J Cardiol. 1987; 60:1340–1355.15. Bakalli A, Georgievska-Ismail L, Koçinaj D, Musliu N, Krasniqi A, Pllana E. Prevalence of left chamber cardiac thrombi in patients with dilated left ventricle at sinus rhythm: the role of transesophageal echocardiography. J Clin Ultrasound. 2013; 41:38–45.16. Papa A, Emdin M, Passino C, Michelassi C, Battaglia D, Cocci F. Predictive value of elevated neutrophil-lymphocyte ratio on cardiac mortality in patients with stable coronary artery disease. Clin Chim Acta. 2008; 395:27–31.17. Momiyama Y, Kawaguchi A, Kajiwara I, et al. Prognostic value of plasma high-sensitivity C-reactive protein levels in Japanese patients with stable coronary artery disease: the Japan NCVC-Collaborative Inflammation Cohort (JNIC) Study. Atherosclerosis. 2009; 207:272–276.18. Doğdu O, Akpek M, Yarlıoğlueş M, et al. Relationship between hematologic parameters and left ventricular systolic dysfunction in stable patients with multi-vessel coronary artery disease. Turk Kardiyol Dern Ars. 2012; 40:706–713.19. Jala VR, Haribabu B. Leukotrienes and atherosclerosis: new roles for old mediators. Trends Immunol. 2004; 25:315–322.20. Ommen SR, Hodge DO, Rodeheffer RJ, McGregor CG, Thomson SP, Gibbons RJ. Predictive power of the relative lymphocyte concentration in patients with advanced heart failure. Circulation. 1998; 97:19–22.21. Horne BD, Anderson JL, John JM, et al. Which white blood cell subtypes predict increased cardiovascular risk? J Am Coll Cardiol. 2005; 45:1638–1643.22. Doğan M, Akyel A, Cimen T, et al. Relationship between neutrophilto-lymphocyte ratio and saphenous vein graft disease in patients with coronary bypass. Clin Appl Thromb Hemost. 2015; 21:25–29.23. Tokgoz S, Kayrak M, Akpinar Z, et al. Neutrophil lymphocyte ratio as a predictor of stroke. J Stroke Cerebrovasc Dis. 2013; 22:1169–1174.24. Yilmaz M, Tenekecioglu E, Arslan B, et al. White blood cell subtypes and neutrophil-lymphocyte ratio in prediction of coronary thrombus formation in non-ST-segment elevated acute coronary syndrome. Clin Appl Thromb Hemost. 2015; 21:446–452.25. Gazi E, Bayram B, Gazi S, et al. Prognostic Value of the Neutrophil-Lymphocyte Ratio in Patients With ST-Elevated Acute Myocardial Infarction. Clin Appl Thromb Hemost. 2015; 21:155–159.26. Yayla Ç, Canpolat U, Akyel A, et al. Association Between Platelet to Lymphocyte Ratio and Saphenous Vein Graft Disease. Angiology. 2016; 67:133–138.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Incidence of Left Ventricular Thrombus after Acute Myocardial Infarction
- Surgical Removal of a Pedunculated Left Ventricular thrombus
- Major Trauma induced Left Ventricular Thrombus after Acute Myocardial Infarction
- Neutrophil-to-Lymphocyte Ratio at Emergency Room Predicts Mechanical Complications of ST-segment Elevation Myocardial Infarction
- Ventricular Remodeling after Acute Myocardial Infarction