Intest Res.
2016 Oct;14(4):314-321. 10.5217/ir.2016.14.4.314.
Narrow-band imaging with magnifying endoscopy for Peyer's patches is useful in predicting the recurrence of remissive patients with ulcerative colitis
- Affiliations
-
- 1Department of Gastroenterology and Hepatology, Osaka University Graduate School of Medicine, Osaka, Japan. hiijima@gh.med.osaka-u.ac.jp
- 2Department of Therapeutics for Inflammatory Bowel Diseases, Osaka University Graduate School of Medicine, Osaka, Japan.
- 3Department of Gastroenterology, Sumitomo Hospital, Osaka, Japan.
- 4Department of Gastroenterological Surgery, Osaka University Graduate School of Medicine, Osaka, Japan.
- 5Department of Gastroenterology, Osaka Rosai Hospital, Osaka, Japan.
- KMID: 2354949
- DOI: http://doi.org/10.5217/ir.2016.14.4.314
Abstract
- BACKGROUND/AIMS
Peyer's patches (PPs) are aggregates of lymphoid follicles that are mainly located in the distal ileum; they play a major role in mucosal immunity. We recently reported that patients with ulcerative colitis (UC) have alterations in PPs that can be detected using narrow-band imaging with magnifying endoscopy (NBI-ME). However, the usefulness of NBI-ME in UC treatment as a whole is still unknown.
METHODS
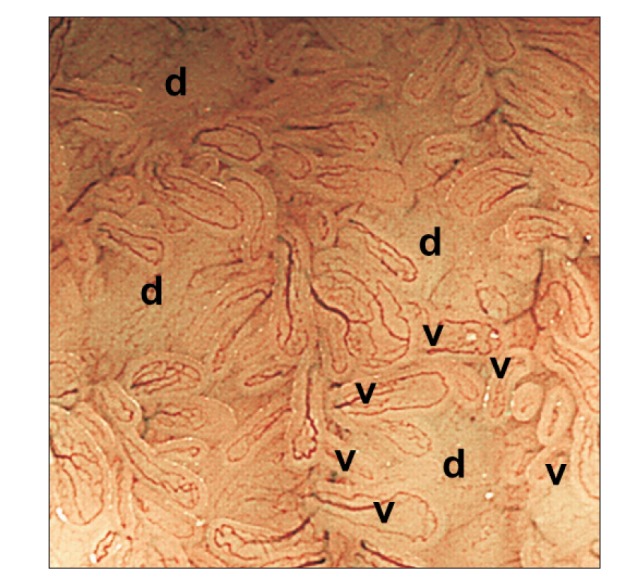
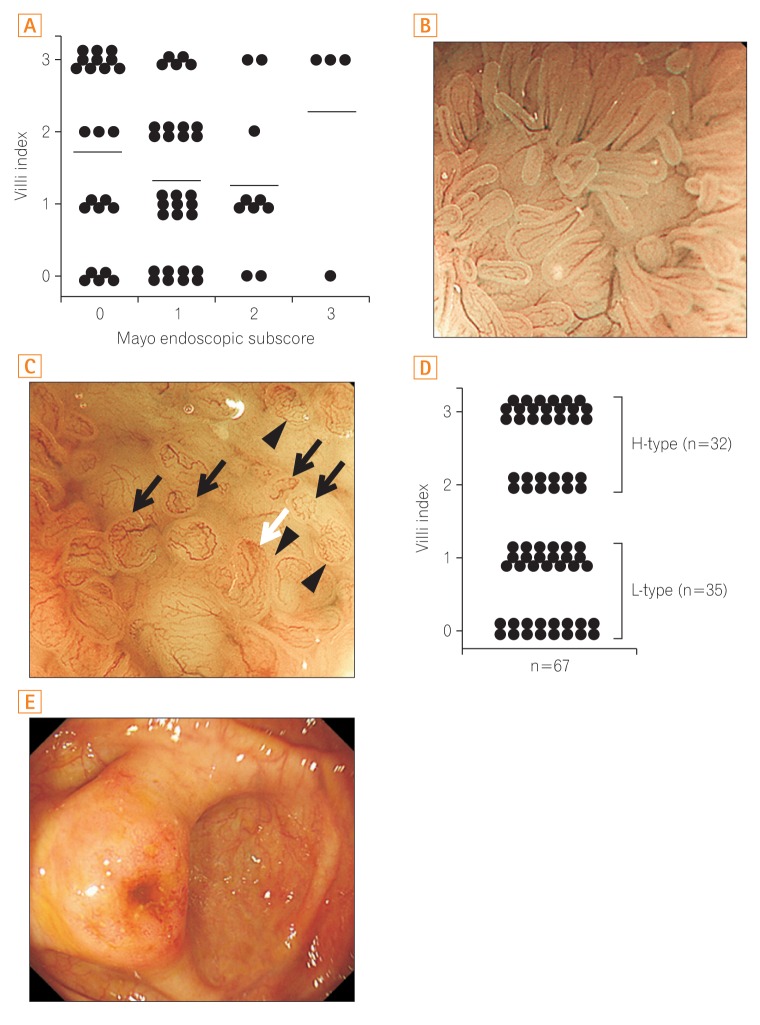
We collected NBI-ME images of PPs from 67 UC patients who had undergone ileocolonoscopy. We evaluated changes in the villi using the "villi index," which is based on three categories: irregular formation, hyperemia, and altered vascular network pattern. The patients were divided into two groups on the basis of villi index: low (L)- and high (H)-types. We then determined the correlation between morphological alteration of the PPs and various clinical characteristics. In 52 patients who were in clinical remission, we also analyzed the correlation between NBI-ME findings of PPs and clinical recurrence.
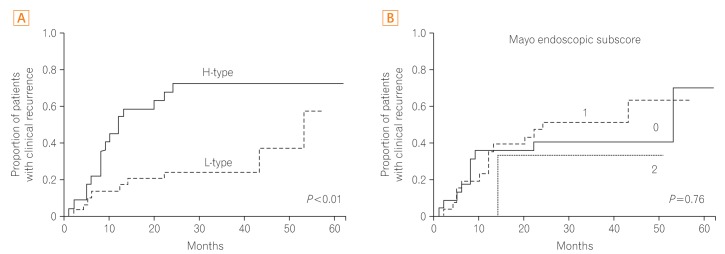
RESULTS
The time to clinical recurrence was significantly shorter in remissive UC patients with H-type PPs than in those with L-type PPs (P<0.01). Moreover, PP alterations were not correlated with age, sex, disease duration, clinical activity, endoscopic score, or extent of disease involvement. Multivariate analysis revealed that the existence of H-type PPs was an independent risk factor for clinical recurrence (hazard ratio, 3.3; P<0.01).
CONCLUSIONS
UC patients with morphological alterations in PPs were at high risk of clinical relapse. Therefore, to predict the clinical course of UC, it may be useful to evaluate NBI-ME images of PPs.
MeSH Terms
Figure
Cited by 1 articles
-
Can narrow-band imaging of Peyer's patches predict the recurrence of ulcerative colitis?
Yoon Jae Kim
Intest Res. 2016;14(4):295-296. doi: 10.5217/ir.2016.14.4.295.
Reference
-
1. Iijima H, Takahashi I, Kiyono H. Mucosal immune network in the gut for the control of infectious diseases. Rev Med Virol. 2001; 11:117–133. PMID: 11262530.
Article2. Van Kruiningen HJ, West AB, Freda BJ, Holmes KA. Distribution of Peyer's patches in the distal ileum. Inflamm Bowel Dis. 2002; 8:180–185. PMID: 11979138.
Article3. Leone V, Chang EB, Devkota S. Diet, microbes, and host genetics: the perfect storm in inflammatory bowel diseases. J Gastroenterol. 2013; 48:315–321. PMID: 23475322.
Article4. MacDonald TT, Spencer J, Viney JL, Williams CB, Walker-Smith JA. Selective biopsy of human Peyer's patches during ileal endoscopy. Gastroenterology. 1987; 93:1356–1362. PMID: 3500086.
Article5. Annese V, Daperno M, Rutter MD, et al. European evidence basedconsensus for endoscopy in inflammatory bowel disease. J Crohns Colitis. 2013; 7:982–1018. PMID: 24184171.
Article6. Hiyama S, Iijima H, Shinzaki S, et al. Narrow band imaging with magnifying endoscopy for Peyer's patches in patients with inflammatory bowel disease. Digestion. 2013; 87:269–280. PMID: 23774764.
Article7. Podolsky DK. Inflammatory bowel disease (1). N Engl J Med. 1991; 325:928–937. PMID: 1881418.8. Podolsky DK. Inflammatory bowel disease (2). N Engl J Med. 1991; 325:1008–1016. PMID: 1886623.9. Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis: a randomized study. N Engl J Med. 1987; 317:1625–1629. PMID: 3317057.
Article10. Cornes JS. Number, size, and distribution of Peyer's patches in the human small intestine. Part I: the development of Peyer's patches. Gut. 1965; 6:225–229. PMID: 18668776.
Article11. Nishio Y, Ando T, Maeda O, et al. Pit patterns in rectal mucosa assessed by magnifying colonoscope are predictive of relapse in patients with quiescent ulcerative colitis. Gut. 2006; 55:1768–1773. PMID: 16682428.
Article12. Jauregui-Amezaga A, López-Cerón M, Aceituno M, et al. Accuracy of advanced endoscopy and fecal calprotectin for prediction of relapse in ulcerative colitis: a prospective study. Inflamm Bowel Dis. 2014; 20:1187–1193. PMID: 24874457.
Article13. Ishii H, Isomoto H, Shikuwa S, et al. Peyer's patches in the terminal ileum in ulcerative colitis: magnifying endoscopic findings. J Clin Biochem Nutr. 2010; 46:111–118. PMID: 20216943.
Article14. Gono K, Obi T, Yamaguchi M, et al. Appearance of enhanced tissue features in narrow-band endoscopic imaging. J Biomed Opt. 2004; 9:568–577. PMID: 15189095.
Article15. Kashida H. Usage of narrow band imaging system in the colorectum. Intest Res. 2009; 7:1–7.16. Sands BE. Biomarkers of inflammation in inflammatory bowel disease. Gastroenterology. 2015; 149:1275–1285.e2. PMID: 26166315.17. Liverani E, Scaioli E, Digby RJ, Bellanova M, Belluzzi A. How to predict clinical relapse in inflammatory bowel disease patients. World J Gastroenterol. 2016; 22:1017–1033. PMID: 26811644.18. Henriksen M, Jahnsen J, Lygren I, et al. C-reactive protein: a predictive factor and marker of inflammation in inflammatory bowel disease. Results from a prospective population-based study. Gut. 2008; 57:1518–1523. PMID: 18566104.19. Ardizzone S, Maconi G, Russo A, Imbesi V, Colombo E, Bianchi Porro G. Randomised controlled trial of azathioprine and 5-aminosalicylic acid for treatment of steroid dependent ulcerative colitis. Gut. 2006; 55:47–53. PMID: 15972298.
Article20. Colombel JF, Rutgeerts P, Reinisch W, et al. Early mucosal healing with infliximab is associated with improved long-term clinical outcomes in ulcerative colitis. Gastroenterology. 2011; 141:1194–1201. PMID: 21723220.
Article21. Boal Carvalho P, Dias de Castro F, Rosa B, Moreira MJ, Cotter J. Mucosal healing in ulcerative colitis: when zero is better. J Crohns Colitis. 2016; 10:20–25. PMID: 26438714.22. Haskell H, Andrews CW Jr, Reddy SI, et al. Pathologic features and clinical significance of "backwash" ileitis in ulcerative colitis. Am J Surg Pathol. 2005; 29:1472–1481. PMID: 16224214.
Article23. Park SH, Loftus EV Jr, Yang SK. Appendiceal skip inflammation and ulcerative colitis. Dig Dis Sci. 2014; 59:2050–2057. PMID: 24705639.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Can narrow-band imaging of Peyer's patches predict the recurrence of ulcerative colitis?
- Clinical Usefulness of Magnifying Chromoendoscopy and Magnifying Narrow Band Imaging Endoscopy for Predicting the Submucosal Invasion of Early Colorectal Cancers
- Usefulness of Narrow-Band Imaging in Endoscopic Submucosal Dissection of the Stomach
- Interobserver Agreement in Using Magnifying Narrow Band Imaging System
- Application of artificial intelligence for diagnosis of early gastric cancer based on magnifying endoscopy with narrow-band imaging