Korean J Pain.
2016 Oct;29(4):255-261. 10.3344/kjp.2016.29.4.255.
Analysis of thoracic epidurography and correlating factors affecting the extent of contrast medium spread
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Keimyung University Dongsan Hospital, School of Medicine, Daegu, Korea. swon13@daum.net
- KMID: 2354218
- DOI: http://doi.org/10.3344/kjp.2016.29.4.255
Abstract
- BACKGROUND
Thoracic epidural anesthesia is frequently used to maintain intraoperative and postoperative analgesia. Frequently, 3 ml of local anesthetic is used as a test dose, or for intermittent epidural injection. We assessed the extent of the spread of 3 ml of contrast medium in the thoracic epidural space and attempted to identify any correlating factors affecting the epidurography.
METHODS
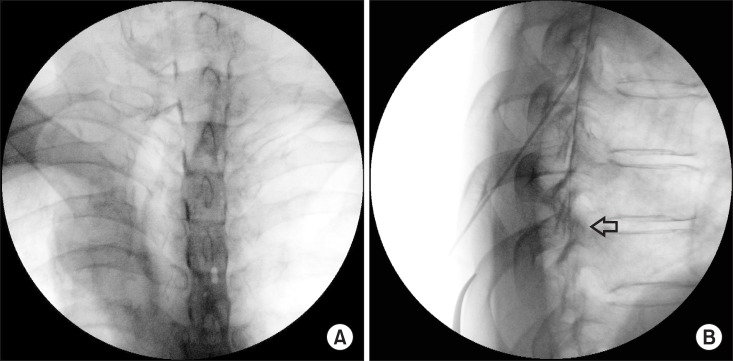
A total of 70 patients were enrolled in the study, and thoracic epidural catheterizations were performed under fluoroscopic guidance. Using 3 ml of contrast medium, epidurography was evaluated to confirm the number of spinal segments covered by the contrast medium. Correlation analysis was performed between patient characteristics (sex, age, body mass index, weight, height, and location of catheter tip) and the extent of the contrast spread.
RESULTS
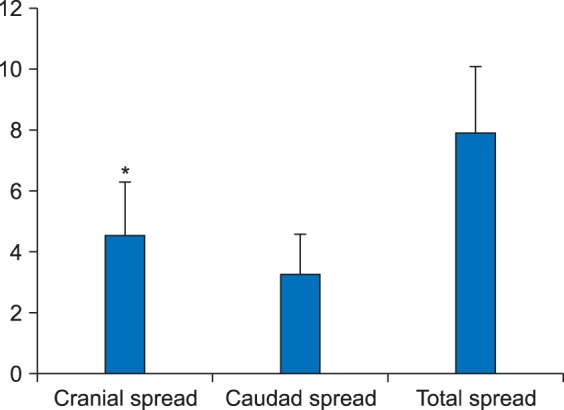
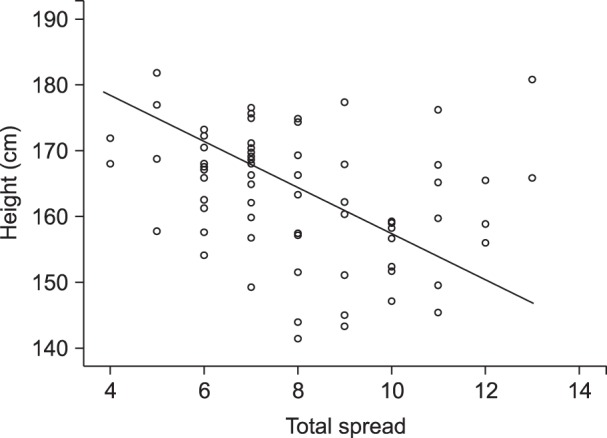
The mean number of vertebral segments evaluated by contrast medium was 7.9 ± 2.2 using 3 ml of contrast medium. The contrast spread in the cranial direction showed more extensive distribution than that in the caudal direction, with statistical significance (P < 0.01). Patient height demonstrated a negative correlation with the extent of distribution of contrast medium (r = −0.311, P < 0.05).
CONCLUSIONS
Thoracic epidurography using 3 ml of contrast medium results in coverage of a mean of 7.9 ± 2.2 spinal segments, with more extensive cranial spread, and patient height showed a weak negative correlation with the distribution of contrast medium.
Keyword
MeSH Terms
Figure
Reference
-
1. Zhang D, Fujiwara R, Iseri T, Nagahama S, Kakishima K, Kamata M, et al. Distribution of contrast medium epidurally injected at thoracic and lumbar vertebral segments. J Vet Med Sci. 2013; 75:663–666. PMID: 23292108.
Article2. Gessler F, Mutlak H, Tizi K, Senft C, Setzer M, Seifert V, et al. Postoperative patient-controlled epidural analgesia in patients with spondylodiscitis and posterior spinal fusion surgery. J Neurosurg Spine. 2016; 24:965–970. PMID: 26849711.
Article3. Nishimori M, Low JH, Zheng H, Ballantyne JC. Epidural pain relief versus systemic opioid-based pain relief for abdominal aortic surgery. Cochrane Database Syst Rev. 2012; CD005059. PMID: 22786494.
Article4. Pöpping DM, Elia N, Marret E, Remy C, Tramèr MR. Protective effects of epidural analgesia on pulmonary complications after abdominal and thoracic surgery: a meta-analysis. Arch Surg. 2008; 143:990–999. PMID: 18936379.
Article5. Kim SH, Yoon KB, Yoon DM, Kim CM, Shin YS. Patient-controlled epidural analgesia with ropivacaine and fentanyl: experience with 2,276 surgical patients. Korean J Pain. 2013; 26:39–45. PMID: 23342206.
Article6. Park SK, Choi YS, Choi SW, Song SW. A comparison of three methods for postoperative pain control in patients undergoing arthroscopic shoulder surgery. Korean J Pain. 2015; 28:45–51. PMID: 25589946.
Article7. Windisch O, Heidegger CP, Giraud R, Morel P, Bühler L. Thoracic epidural analgesia: a new approach for the treatment of acute pancreatitis? Crit Care. 2016; 20:116. PMID: 27141977.
Article8. Visser WA, Lee RA, Gielen MJ. Factors affecting the distribution of neural blockade by local anesthetics in epidural anesthesia and a comparison of lumbar versus thoracic epidural anesthesia. Anesth Analg. 2008; 107:708–721. PMID: 18633056.
Article9. Yokoyama M, Hanazaki M, Fujii H, Mizobuchi S, Nakatsuka H, Takahashi T, et al. Correlation between the distribution of contrast medium and the extent of blockade during epidural anesthesia. Anesthesiology. 2004; 100:1504–1510. PMID: 15166571.
Article10. Kim YC, Lim YJ, Lee SC. Spreading pattern of epidurally administered contrast medium in rabbits. Acta Anaesthesiol Scand. 1998; 42:1092–1095. PMID: 9809094.
Article11. Iwata Y, Hamai Y, Koyama T. Anesthetic management of nonintubated video-assisted thoracoscopic surgery using epidural anesthesia and dexmedetomidine in three patients with severe respiratory dysfunction. J Anesth. 2016; 30:324–327. PMID: 26758074.
Article12. Kim KS, Shin SS, Kim TS, Jeong CY, Yoon MH, Choi JI. Fluoroscopically guided cervical interlaminar epidural injections using the midline approach: an analysis of epidurography contrast patterns. Anesth Analg. 2009; 108:1658–1661. PMID: 19372351.
Article13. Huang CH. Effect of cervical epidural blockade with 2% lidocaine plus epinephrine on respiratory function. Acta Anaesthesiol Taiwan. 2007; 45:217–222. PMID: 18251242.14. Groeben H. Epidural anesthesia and pulmonary function. J Anesth. 2006; 20:290–299. PMID: 17072694.
Article15. Lee CJ, Jeon Y, Lim YJ, Bahk JH, Kim YC, Lee SC, et al. The influence of neck flexion and extension on the distribution of contrast medium in the high thoracic epidural space. Anesth Analg. 2007; 104:1583–1586. PMID: 17513662.
Article16. Saitoh K, Hirabayashi Y, Shimizu R, Mitsuhata H, Fukuda H. Extensive extradural spread in the elderly may not relate to decreased leakage through intervertebral foramina. Br J Anaesth. 1995; 75:688–691. PMID: 8672314.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spreading pattern of contrast medium in the high thoracic epidural space in rabbits: the effect of neck flexion and extension
- Preliminary study on contrast flow analysis of thoracic transforaminal epidural block
- An Analysis of Pattern of Transforaminal Epidurography
- Spreading Pattem of Epidurally - Administered Contrast Media in Rabbits
- Incidence of inadvertent intercostal or epidural spread during thoracic sympathetic ganglion block