Korean J Ophthalmol.
2016 Oct;30(5):377-381. 10.3341/kjo.2016.30.5.377.
The Relationship between Neutrophil-to-lymphocyte Ratio and Age-related Macular Degeneration
- Affiliations
-
- 1Department of Ophthalmology, Dr. Sami Ulus Maternity and Children's Health and Diseases Training and Research Hospital, Ankara, Turkey. becekurtul@yahoo.com
- KMID: 2353831
- DOI: http://doi.org/10.3341/kjo.2016.30.5.377
Abstract
- PURPOSE
To investigate the possible associations of neutrophil-to-lymphocyte ratio (NLR) and high sensitivity C-reactive protein (hs-CRP) level with age-related macular degeneration (ARMD).
METHODS
Patients were divided to three groups of 40 patients with non-neovascular ARMD (group 1), 40 patients with neovascular ARMD (group 2), and 40 healthy control subjects (group 3). The neutrophil and lymphocyte counts were evaluated using an ABX Pentra DF120/USA biochemical analyzer, and hs-CRP levels were measured using a Beckman Coulter Immage 800. The NLR was measured by dividing neutrophil count by lymphocyte count.
RESULTS
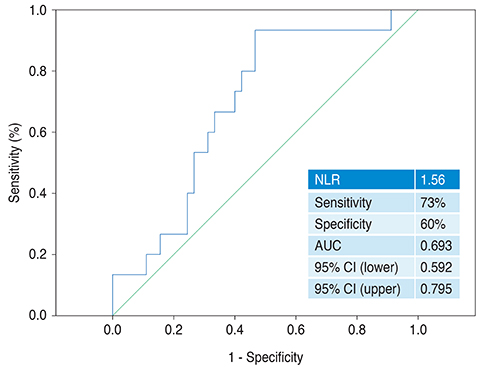
The patients in group 2 were older and more often diabetic than the patients in groups 1 and 3 (p < 0.001 and p < 0.001, respectively). The NLR level was 1.65 ± 0.71 in group 1, 1.98 ± 0.84 in group 2, and 1.46 ± 0.44 in group 3. The hs-CRP value was 1.98 ± 0.251 mg/L in group 1, 3.242 ± 0.211 mg/L in group 2, and 1.145 ± 0.193 mg/L in group 3. Both NLR and hs-CRP values were significantly higher in group 2 compared to group 3 (p = 0.002 and p = 0.002, respectively). In multivariate analysis, NLR remained an independent predictor of neovascular ARMD (odds ratio, 3.882; 95% confidence interval, 1.574 to 9.576; p = 0.003) together with age (p < 0.001), diabetes mellitus (p = 0.041), and hs-CRP (p = 0.018).
CONCLUSIONS
Our study suggests that increased NLR value is independently associated with neovascular ARMD.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Are There Relationships between Seminal Parameters and the Neutrophil-to-Lymphocyte Ratio or the Platelet-to-Lymphocyte Ratio?
Serdar Aykan, Lütfi Canat, Serkan Gönültaş, Hasan Anıl Atalay, Fatih Altunrende
World J Mens Health. 2017;35(1):51-56. doi: 10.5534/wjmh.2017.35.1.51.Male Inflammatory Parameters Are not Useful to Predict the Outcomes of Intracytoplasmic Sperm Injection: Results from a Cross-Sectional Study
Gianmartin Cito, Maria Elisabetta Coccia, Rita Picone, Andrea Cocci, Giorgio Ivan Russo, Tommaso Cai, Giulia Bencini, Rossella Fucci, Elisabetta Micelli, Luciana Criscuoli, Francesco Bertocci, Elena Borrani, Sergio Serni, Marco Carini, Alessandro Natali
World J Mens Health. 2019;37(3):347-354. doi: 10.5534/wjmh.180110.
Reference
-
1. Subramani S, Khor SE, Livingstone BI, Kulkarni UV. Serum uric acid levels and its association with age-related macular degeneration (ARMD). Med J Malaysia. 2010; 65:36–40.2. Coral K, Raman R, Rathi S, et al. Plasma homocysteine and total thiol content in patients with exudative age-related macular degeneration. Eye (Lond). 2006; 20:203–207.3. Rodrigues EB. Inflammation in dry age-related macular degeneration. Ophthalmologica. 2007; 221:143–152.4. Anderson DH, Mullins RF, Hageman GS, Johnson LV. A role for local inflammation in the formation of drusen in the aging eye. Am J Ophthalmol. 2002; 134:411–431.5. Boekhoorn SS, Vingerling JR, Witteman JC, et al. C-reactive protein level and risk of aging macula disorder: the Rotterdam Study. Arch Ophthalmol. 2007; 125:1396–1401.6. Kaya MG. Inflammation and coronary artery disease: as a new biomarker neutrophil/lymphocyte ratio. Turk Kardiyol Dern Ars. 2013; 41:191–192.7. Guthrie GJ, Charles KA, Roxburgh CS, et al. The systemic inflammation-based neutrophil-lymphocyte ratio: experience in patients with cancer. Crit Rev Oncol Hematol. 2013; 88:218–230.8. Musat O, Ochinciuc U, Gutu T, et al. Pathophysiology and treatment of ARMD. Oftalmologia. 2012; 56:45–50.9. Danulescu R, Costin D. The assessment of treatment efficacy in age related macular degeneration by evaluating the oxidative stress markers and OCT measurements. Rev Med Chir Soc Med Nat Iasi. 2013; 117:328–333.10. Swanson MW, McGwin G Jr. Anti-inflammatory drug use and age-related macular degeneration. Optom Vis Sci. 2008; 85:947–950.11. Becerra EM, Morescalchi F, Gandolfo F, et al. Clinical evidence of intravitreal triamcinolone acetonide in the management of age-related macular degeneration. Curr Drug Targets. 2011; 12:149–172.12. Amrite AC, Kompella UB. Celecoxib inhibits proliferation of retinal pigment epithelial and choroid-retinal endothelial cells by a cyclooxygenase-2-independent mechanism. J Pharmacol Exp Ther. 2008; 324:749–758.13. Turkmen K, Ozcicek F, Ozcicek A, et al. The relationship between neutrophil-to-lymphocyte ratio and vascular calcification in end-stage renal disease patients. Hemodial Int. 2014; 18:47–53.14. Ahsen A, Ulu MS, Yuksel S, et al. As a new inflammatory marker for familial Mediterranean fever: neutrophil-to-lymphocyte ratio. Inflammation. 2013; 36:1357–1362.15. Seddon JM, Gensler G, Milton RC, et al. Association between C-reactive protein and age-related macular degeneration. JAMA. 2004; 291:704–710.16. Seddon JM, Gensler G, Klein ML, Milton RC. C-reactive protein and homocysteine are associated with dietary and behavioral risk factors for age-related macular degeneration. Nutrition. 2006; 22:441–443.17. Nowak M, Swietochowska E, Wielkoszynski T, et al. Homocysteine, vitamin B12, and folic acid in age-related macular degeneration. Eur J Ophthalmol. 2005; 15:764–767.18. Mehryar M, Farvardin M, Hosseini H, Aslani M. Potential role of uric acid in the molecular pathogenesis of age-related macular degeneration. Med Hypotheses. 2006; 66:793–795.19. Ulu SM, Dogan M, Ahsen A, et al. Neutrophil-to-lymphocyte ratio as a quick and reliable predictive marker to diagnose the severity of diabetic retinopathy. Diabetes Technol Ther. 2013; 15:942–947.20. Ilhan N, Daglioglu MC, Ilhan O, et al. Assessment of neutrophil/lymphocyte ratio in patients with age-related macular degeneration. Ocul Immunol Inflamm. 2014; 07. 02. 1–4.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship between Age-Related Macular Degeneration and Hyperuricemia Based on the 7th and 8th Korea National Health and Nutrition Examination Survey
- Clinical Significance of Preoperative Inflammatory Parameters in Gastric Cancer Patients
- Relationships Between Schizophrenia Severity and Inflammatory Biomarker: Neutrophil/Lymphocyte Ratio, Monocyte/Lymphocyte Ratio, Platelet/Lymphocyte Ratio
- Association between Copper–Zinc Ratio in Hair and Neutrophil–Lymphocyte Ratio within the Context of a Normal White Blood Cell Count among Overweight or Obese Korean Individuals: A Pilot Study
- Hereditary Macular Degeneration which Involved A Brother and Sister of One Family