J Breast Cancer.
2014 Jun;17(2):184-187.
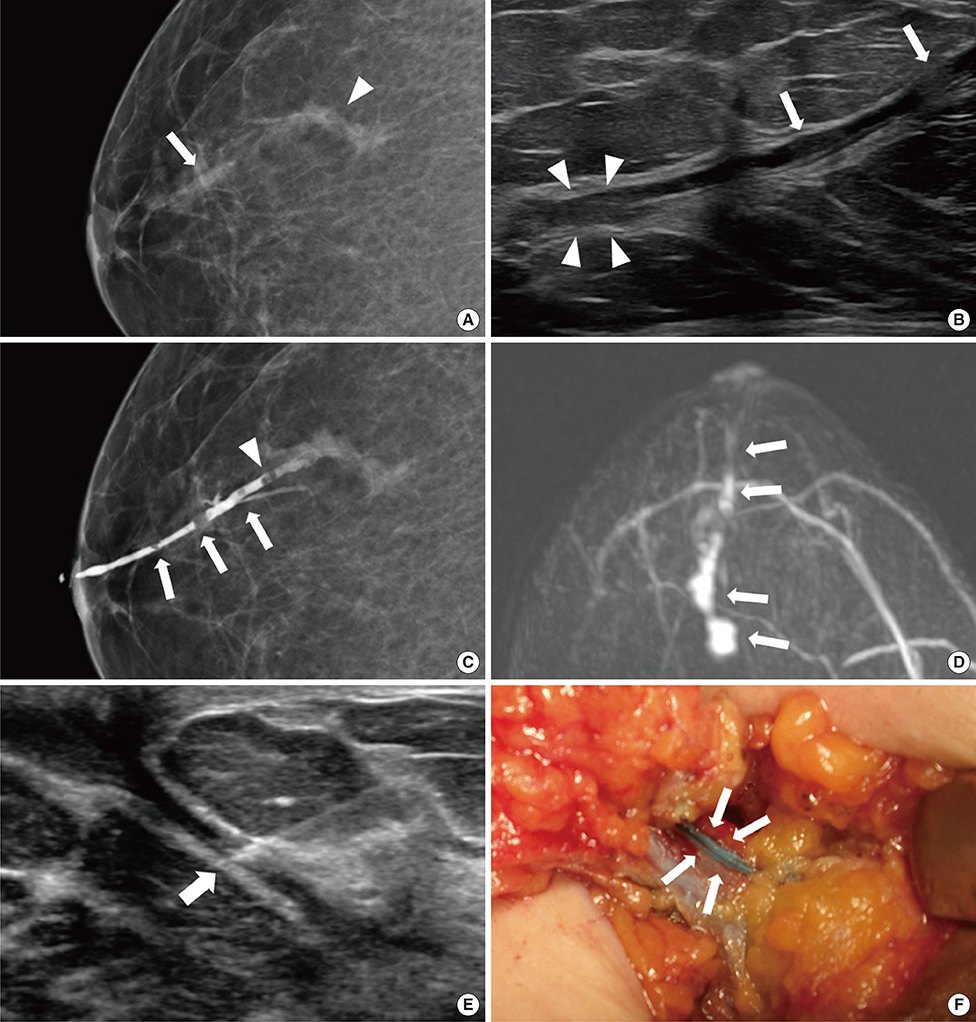
Microdochectomy Assisted by Ultrasound-Guided Indigo Carmine Staining of Intraductal Lesions: A Case Report
- Affiliations
-
- 1Department of Radiology, Dongguk University Ilsan Hospital, Dongguk University College of Medicine, Goyang, Korea. dbkim@dumc.or.kr
- 2Department of Surgery, Dongguk University Ilsan Hospital, Dongguk University College of Medicine, Goyang, Korea.
Abstract
- Spontaneous bloody nipple discharge from a single duct is a significant clinical problem. When performing preoperative marking of the discharging duct, it is sometimes difficult to identify the duct owing to intermittent discharge. Precise preoperative marking of the discharging duct and intraductal lesions is very important to avoid unnecessary wide excision of breast tissue or failure to remove the cause of nipple discharge. We herein present a case of preoperative ultrasound-guided indigo carmine staining in a patient with no discharge on the day of surgery. When a dilated duct is visualized on ultrasound, the targeted duct can be localized using indigo carmine staining, and it is possible to perform a precise minimal volume microdochectomy.
Keyword
Figure
Reference
-
1. Saarela AO, Kiviniemi HO, Rissanen TJ. Preoperative methylene blue staining of galactographically suspicious breast lesions. Int Surg. 1997; 82:403–405.2. Hahn M, Fehm T, Solomayer EF, Siegmann KC, Hengstmann AS, Wallwiener D, et al. Selective microdochectomy after ductoscopic wire marking in women with pathological nipple discharge. BMC Cancer. 2009; 9:151.
Article3. Ferris-James DM, Iuanow E, Mehta TS, Shaheen RM, Slanetz PJ. Imaging approaches to diagnosis and management of common ductal abnormalities. Radiographics. 2012; 32:1009–1030.
Article4. Rissanen T, Reinikainen H, Apaja-Sarkkinen M. Breast sonography in localizing the cause of nipple discharge: comparison with galactography in 52 patients. J Ultrasound Med. 2007; 26:1031–1039.5. Rissanen T, Typpö T, Tikkakoski T, Turunen J, Myllymäki T, Suramo I. Ultrasound-guided percutaneous galactography. J Clin Ultrasound. 1993; 21:497–502.
Article6. Hussain S, Lui DM. Ultrasound guided percutaneous galactography. Eur J Radiol. 1997; 24:163–165.
Article7. Dinkel HP, Trusen A, Gassel AM, Rominger M, Lourens S, Müller T, et al. Predictive value of galactographic patterns for benign and malignant neoplasms of the breast in patients with nipple discharge. Br J Radiol. 2000; 73:706–714.
Article8. Koskela A, Berg M, Pietiläinen T, Mustonen P, Vanninen R. Breast lesions causing nipple discharge: preoperative galactography-aided stereotactic wire localization. AJR Am J Roentgenol. 2005; 184:1795–1798.
Article9. Sharma N, Huston TL, Simmons RM. Intraoperative intraductal injection of methylene blue dye to assist in major duct excision. Am J Surg. 2006; 191:553–554.
Article10. Dillon MF, Mohd Nazri SR, Nasir S, McDermott EW, Evoy D, Crotty TB, et al. The role of major duct excision and microdochectomy in the detection of breast carcinoma. BMC Cancer. 2006; 6:164.
Article11. Jo YY, Lee MG, Yun SY, Lee KC. Profound hypotension after an intradermal injection of indigo carmine for sentinel node mapping. J Breast Cancer. 2013; 16:127–128.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hypotension in patients administered indigo carmine containing impurities: A case report
- Cardiac arrest from intravenous indigo carmine during laparoscopic surgery: A case report
- Detection of Polyps Including Adenomas in the Ascending Colon by Cap-assisted Chromocolonoscopy with Indigo Carmine
- Profound Hypotension after an Intradermal Injection of Indigo Carmine for Sentinel Node Mapping
- Extreme Hypotension Followed by an Intravenous Indigo Carmine Injection during a Radical Prostatectomy: A case report