Yonsei Med J.
2015 Jan;56(1):220-226. 10.3349/ymj.2015.56.1.220.
Epidemiology of Trauma Patients and Analysis of 268 Mortality Cases: Trends of a Single Center in Korea
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Yonsei University Wonju College of Medicine, Wonju, Korea. nicecs@yonsei.ac.kr
- 2Department of Surgery, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 3Department of Emergency Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 4Department of Anesthesiology and Pain Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea.
- KMID: 2352810
- DOI: http://doi.org/10.3349/ymj.2015.56.1.220
Abstract
- PURPOSE
There is an increasing incidence of mortality among trauma patients; therefore, it is important to analyze the trauma epidemiology in order to prevent trauma death. The authors reviewed the trauma epidemiology retrospectively at a regional emergency center of Korea and evaluated the main factors that led to trauma-related deaths.
MATERIALS AND METHODS
A total of 17007 trauma patients were registered to the trauma registry of the regional emergency center at Wonju Severance Christian Hospital in Korea from January 2010 to December 2012.
RESULTS
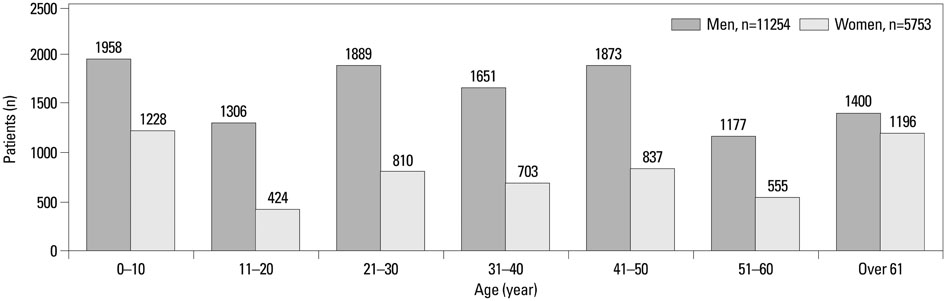
The mean age of patients was 35.2 years old. The most frequent trauma mechanism was blunt injury (90.8%), as well as slip-and-fall down injury, motor vehicle accidents, and others. Aside from 142 early trauma deaths, a total of 4673 patients were admitted for further treatment. The most common major trauma sites of admitted patients were on the extremities (38.4%), followed by craniocerebral, abdominopelvis, and thorax. With deaths of 126 patients during in-hospital treatment, the overall mortality (142 early and 126 late deaths) was 5.6% for admitted patients. Ages > or =55, injury severity score > or =16, major craniocerebral injury, cardiopulmonary resuscitation at arrival, probability of survival <25% calculated from the trauma and injury severity score were independent predictors of trauma mortality in multivariate analysis.
CONCLUSION
The epidemiology of the trauma patients studied was found to be mainly blunt trauma. This finding is similar to previous papers in terms of demographics and mechanism. Trauma patients who have risk factors of mortality require careful management in order to prevent trauma-related deaths.
Keyword
MeSH Terms
-
Adolescent
Adult
Age Distribution
Aged
Aged, 80 and over
Cause of Death
Child
Child, Preschool
Emergency Service, Hospital
Female
*Hospital Mortality
Hospitalization
Humans
Infant
Infant, Newborn
Injury Severity Score
Male
Middle Aged
Republic of Korea/epidemiology
Risk Factors
Survivors
Wounds and Injuries/*epidemiology/*mortality
Young Adult
Figure
Reference
-
1. Gross CP, Anderson GF, Powe NR. The relation between funding by the National Institutes of Health and the burden of disease. N Engl J Med. 1999; 340:1881–1887.
Article2. Laxminarayan R, Mills AJ, Breman JG, Measham AR, Alleyne G, Claeson M, et al. Advancement of global health: key messages from the Disease Control Priorities Project. Lancet. 2006; 367:1193–1208.
Article3. World Health Organization. The World Health Report 2003: Shaping the Future. Geneva: World Health Organization;2003.4. National Emergency Medical Center. Annual Report of Emergency Medicine. Seoul: Ministry for Health, Welfare and Family Affairs;2007-2011.5. Lagarde E. Road traffic injury is an escalating burden in Africa and deserves proportionate research efforts. PLoS Med. 2007; 4:e170.
Article6. Hofman K, Primack A, Keusch G, Hrynkow S. Addressing the growing burden of trauma and injury in low- and middle-income countries. Am J Public Health. 2005; 95:13–17.
Article7. National Police Agency. Annual report of traffic accident in Korea 2006. Seoul: National Police Agency;2006.8. Moshiro C, Heuch I, Astrøm AN, Setel P, Hemed Y, Kvåle G. Injury morbidity in an urban and a rural area in Tanzania: an epidemiological survey. BMC Public Health. 2005; 5:11.
Article9. Demircan A, Keles A, Gurbuz N, Bildik F, Aygencel SG, Dogan NO, et al. Forensic emergency medicine - six-year experience of 13823 cases in a university emergency department. Turk J Med Sci. 2008; 38:567–575.10. Mishra B, Sinha Mishra ND, Sukhla S, Sinha A. Epidemiological study of road traffic accident cases from Western Nepal. Indian J Community Med. 2010; 35:115–121.
Article11. Polinder S, Haagsma JA, Toet H, van Beeck EF. Epidemiological burden of minor, major and fatal trauma in a national injury pyramid. Br J Surg. 2012; 99:Suppl 1. 114–121.
Article12. Bulut M, Koksal O, Korkmaz A, Turan M, Ozguc H. Childhood falls: characteristics, outcome, and comparison of the Injury Severity Score and New Injury Severity Score. Emerg Med J. 2006; 23:540–545.
Article13. Lallier M, Bouchard S, St-Vil D, Dupont J, Tucci M. Falls from heights among children: a retrospective review. J Pediatr Surg. 1999; 34:1060–1063.
Article14. Hingson R, Winter M. Epidemiology and consequences of drinking and driving. Alcohol Res Health. 2003; 27:63–78.15. Matthews ML, Moran AR. Age differences in male drivers’ perception of accident risk: the role of perceived driving ability. Accid Anal Prev. 1986; 18:299–313.
Article16. Murray CJL, Lopez AD. Global and regional descriptive epidemiology of disability: incidence, prevalence, health expectancies and years lived with disability. In : Murray CJL, Lopez AD, editors. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries and risk factors in 1990 and projected to 2020. Boston: Harvard University Press;1996. p. 201–246.17. Scheffer AC, Schuurmans MJ, van Dijk N, van der Hooft T, de Rooij SE. Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing. 2008; 37:19–24.
Article18. Mohan D. Childhood injuries in India: extent of the problem and strategies for control. Indian J Pediatr. 1986; 53:607–615.
Article19. Elechi EN, Etawo SU. Pilot study of injured patients seen in the University of Port Harcourt Teaching Hospital, Nigeria. Injury. 1990; 21:234–238.
Article20. Baker CC, Oppenheimer L, Stephens B, Lewis FR, Trunkey DD. Epidemiology of trauma deaths. Am J Surg. 1980; 140:144–150.
Article21. Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. 1997; 349:1498–1504.
Article22. World Health Organization. Preventing Injuries and Violence. A Guide for Ministries of Health. Geneva: World Health Organization;2007. p. 6–9.23. Sogut O, Sayhan MB, Gokdemir MT, Boleken ME, Al B, Kose R, et al. Analysis of Hospital Mortality and Epidemiology in Trauma Patient: A Multi-Center Study. J Curr Surg. 2011; 1:19–24.24. Sanddal TL, Esposito TJ, Whitney JR, Hartford D, Taillac PP, Mann NC, et al. Analysis of preventable trauma deaths and opportunities for trauma care improvement in utah. J Trauma. 2011; 70:970–977.
Article25. Blair E, Topuzlu C, Davis JH. Delayed or missed diagnosis in blunt chest trauma. J Trauma. 1971; 11:129–145.
Article26. LoCicero J 3rd, Mattox KL. Epidemiology of chest trauma. Surg Clin North Am. 1989; 69:15–19.
Article27. Tan WT, Choy JM, Foo JM. A 5-year profile of trauma admissions to the surgical intensive care unit of a tertiary hospital in Singapore. Ann Acad Med Singapore. 2010; 39:363–367.28. Agalar F, Cakmakci M, Sayek I. Factors effecting mortality in urban vertical free falls: evaluation of 180 cases. Int Surg. 1999; 84:271–274.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epidemiology of Facial Bone Fractures During the Coronavirus Disease 2019 Pandemic: A Single Korean Level I Trauma Center Study
- Characteristics of Korean Trauma Patients: A Single-center Analysis Using the Korea Trauma Database
- Mortality Trends in Chest-Abdominal Trauma Patients Before and After the Establishment of Trauma Centers in South Korea
- Epidemiology of Pelvic Ring Fractures in a Level 1 Trauma Center in the Netherlands
- Injury Severity Scores and Quality Assurance of Traumatic Care