Korean J Radiol.
2016 Feb;17(1):127-141. 10.3348/kjr.2016.17.1.127.
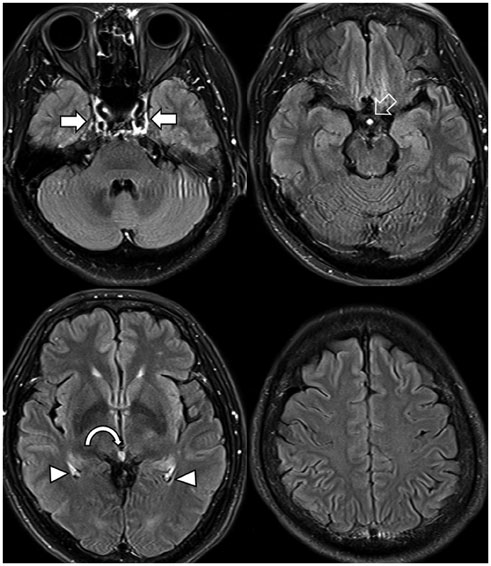
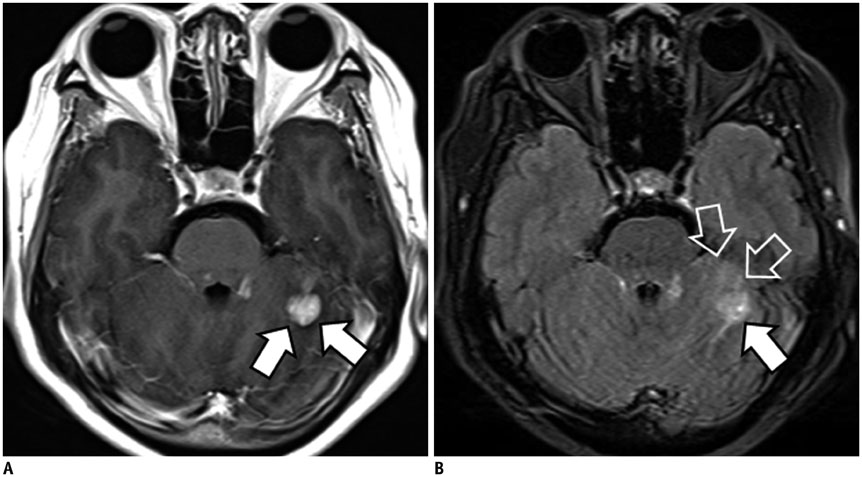
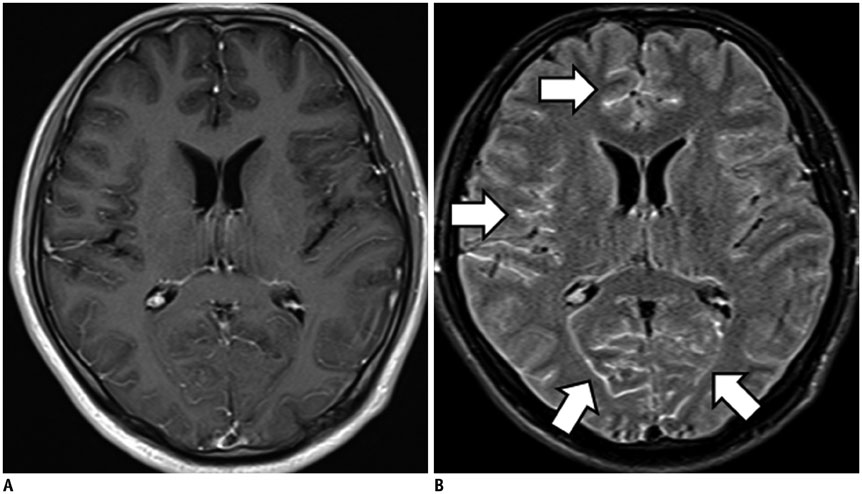
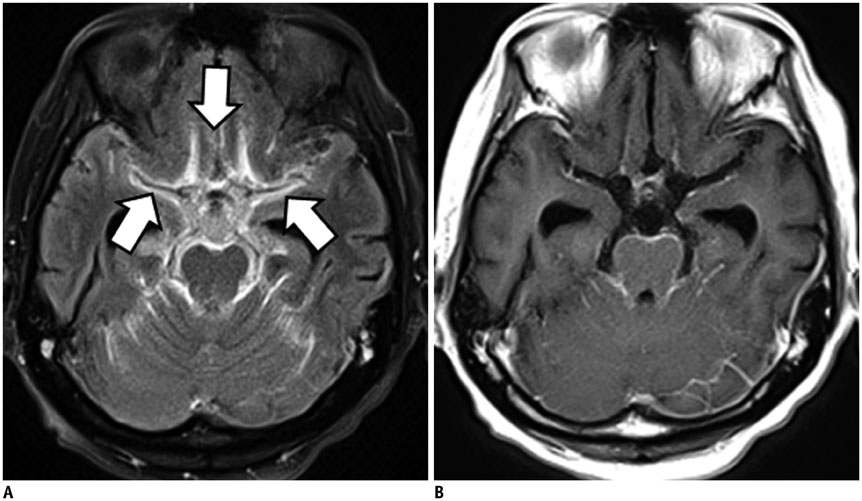
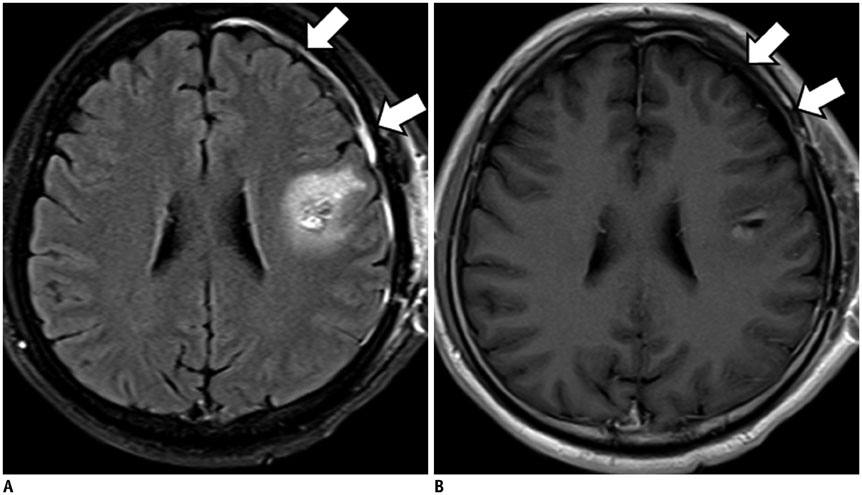
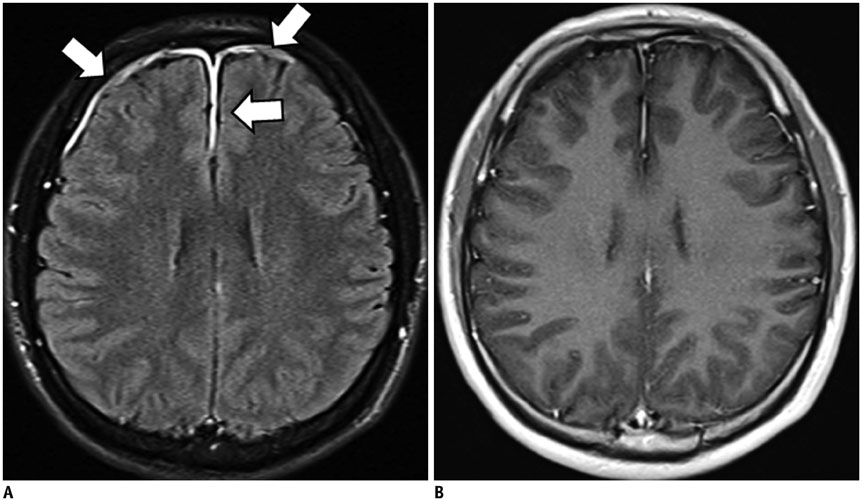
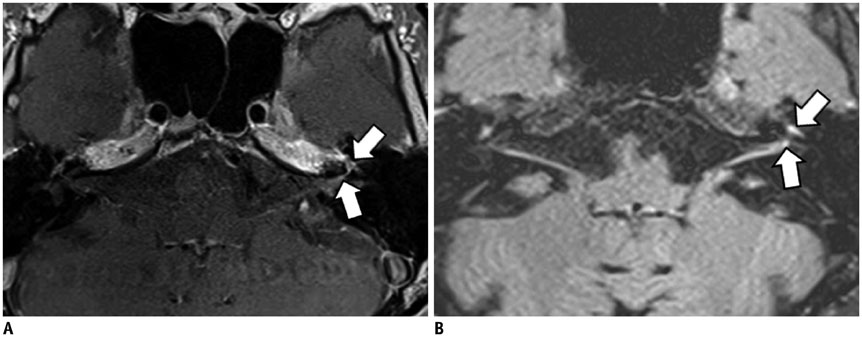
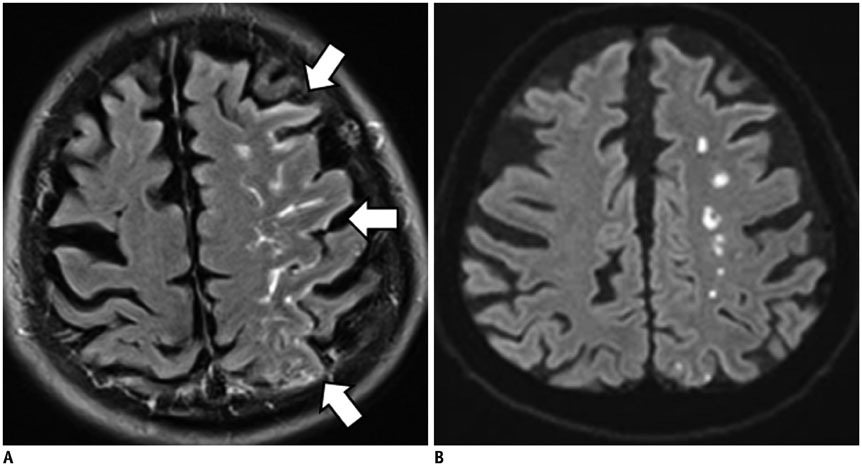
Importance of Contrast-Enhanced Fluid-Attenuated Inversion Recovery Magnetic Resonance Imaging in Various Intracranial Pathologic Conditions
- Affiliations
-
- 1Department of Radiology, Dongguk University Ilsan Hospital, Goyang 10326, Korea. ejl1048@hanmail.net
- 2Department of Radiology, College of Medicine, Kangwon National University, Chuncheon 24289, Korea.
- KMID: 2351172
- DOI: http://doi.org/10.3348/kjr.2016.17.1.127
Abstract
- Intracranial lesions may show contrast enhancement through various mechanisms that are closely associated with the disease process. The preferred magnetic resonance sequence in contrast imaging is T1-weighted imaging (T1WI) at most institutions. However, lesion enhancement is occasionally inconspicuous on T1WI. Although fluid-attenuated inversion recovery (FLAIR) sequences are commonly considered as T2-weighted imaging with dark cerebrospinal fluid, they also show mild T1-weighted contrast, which is responsible for the contrast enhancement. For several years, FLAIR imaging has been successfully incorporated as a routine sequence at our institution for contrast-enhanced (CE) brain imaging in detecting various intracranial diseases. In this pictorial essay, we describe and illustrate the diagnostic importance of CE-FLAIR imaging in various intracranial pathologic conditions.
MeSH Terms
Figure
Cited by 1 articles
-
Does Multiphasic Contrast Enhanced Fluid Attenuated Inversion Recovery Magnetic Resonance Imaging Enhance the Detectability of Small Intracerebral Metastases?
Jung Hwan Kim, Kyung Sik Yi, Chi-Hoon Choi, Seung Tae Woo, Sang-Hoon Cha
J Korean Soc Radiol. 2018;78(3):179-189. doi: 10.3348/jksr.2018.78.3.179.
Reference
-
1. De Coene B, Hajnal JV, Gatehouse P, Longmore DB, White SJ, Oatridge A, et al. MR of the brain using fluid-attenuated inversion recovery (FLAIR) pulse sequences. AJNR Am J Neuroradiol. 1992; 13:1555–1564.2. Rydberg JN, Hammond CA, Grimm RC, Erickson BJ, Jack CR Jr, Huston J 3rd, et al. Initial clinical experience in MR imaging of the brain with a fast fluid-attenuated inversion-recovery pulse sequence. Radiology. 1994; 193:173–180.3. Hajnal JV, Bryant DJ, Kasuboski L, Pattany PM, De Coene B, Lewis PD, et al. Use of fluid attenuated inversion recovery (FLAIR) pulse sequences in MRI of the brain. J Comput Assist Tomogr. 1992; 16:841–844.4. Essig M, Knopp MV, Schoenberg SO, Hawighorst H, Wenz F, Debus J, et al. Cerebral gliomas and metastases: assessment with contrast-enhanced fast fluid-attenuated inversion-recovery MR imaging. Radiology. 1999; 210:551–557.5. Mathews VP, Caldemeyer KS, Lowe MJ, Greenspan SL, Weber DM, Ulmer JL. Brain: gadolinium-enhanced fast fluid-attenuated inversion-recovery MR imaging. Radiology. 1999; 211:257–263.6. Melhem ER, Bert RJ, Walker RE. Usefulness of optimized gadolinium-enhanced fast fluid-attenuated inversion recovery MR imaging in revealing lesions of the brain. AJR Am J Roentgenol. 1998; 171:803–807.7. Mathews VP, Caldemeyer KS, Ulmer JL, Nguyen H, Yuh WT. Effects of contrast dose, delayed imaging, and magnetization transfer saturation on gadolinium-enhanced MR imaging of brain lesions. J Magn Reson Imaging. 1997; 7:14–22.8. Sage MR, Wilson AJ, Scroop R. Contrast media and the brain. The basis of CT and MR imaging enhancement. Neuroimaging Clin N Am. 1998; 8:695–707.9. Smirniotopoulos JG, Murphy FM, Rushing EJ, Rees JH, Schroeder JW. Patterns of contrast enhancement in the brain and meninges. Radiographics. 2007; 27:525–551.10. Fukuoka H, Hirai T, Okuda T, Shigematsu Y, Sasao A, Kimura E, et al. Comparison of the added value of contrast-enhanced 3D fluid-attenuated inversion recovery and magnetization-prepared rapid acquisition of gradient echo sequences in relation to conventional postcontrast T1-weighted images for the evaluation of leptomeningeal diseases at 3T. AJNR Am J Neuroradiol. 2010; 31:868–873.11. Bozzao A, Floris R, Fasoli F, Fantozzi LM, Colonnese C, Simonetti G. Cerebrospinal fluid changes after intravenous injection of gadolinium chelate: assessment by FLAIR MR imaging. Eur Radiol. 2003; 13:592–597.12. Kim EY, Kim SS, Na DG, Roh HG, Ryoo JW, Kim HK. Sulcal hyperintensity on fluid-attenuated inversion recovery imaging in acute ischemic stroke patients treated with intra-arterial thrombolysis: iodinated contrast media as its possible cause and the association with hemorrhagic transformation. J Comput Assist Tomogr. 2005; 29:264–269.13. Köhrmann M, Struffert T, Frenzel T, Schwab S, Doerfler A. The hyperintense acute reperfusion marker on fluid-attenuated inversion recovery magnetic resonance imaging is caused by gadolinium in the cerebrospinal fluid. Stroke. 2012; 43:259–261.14. Tsuchiya K, Katase S, Yoshino A, Hachiya J. FLAIR MR imaging for diagnosing intracranial meningeal carcinomatosis. AJR Am J Roentgenol. 2001; 176:1585–1588.15. Kremer S, Abu Eid M, Bierry G, Bogorin A, Koob M, Dietemann JL, et al. Accuracy of delayed post-contrast FLAIR MR imaging for the diagnosis of leptomeningeal infectious or tumoral diseases. J Neuroradiol. 2006; 33:285–291.16. Jeon JY, Choi JW, Roh HG, Moon WJ. Effect of imaging time in the magnetic resonance detection of intracerebral metastases using single dose gadobutrol. Korean J Radiol. 2014; 15:145–150.17. Bagheri MH, Meshksar A, Nabavizadeh SA, Borhani-Haghighi A, Ashjazadeh N, Nikseresht AR. Diagnostic value of contrast-enhanced fluid-attenuated inversion-recovery and delayed contrast-enhanced brain MRI in multiple sclerosis. Acad Radiol. 2008; 15:15–23.18. Goo HW, Choi CG. Post-contrast FLAIR MR imaging of the brain in children: normal and abnormal intracranial enhancement. Pediatr Radiol. 2003; 33:843–849.19. Essig M, Schoenberg SO, Debus J, van Kaick G. Disappearance of tumor contrast on contrast-enhanced FLAIR imaging of cerebral gliomas. Magn Reson Imaging. 2000; 18:513–518.20. Terae S, Yoshida D, Kudo K, Tha KK, Fujino M, Miyasaka K. Contrast-enhanced FLAIR imaging in combination with pre- and postcontrast magnetization transfer T1-weighted imaging: usefulness in the evaluation of brain metastases. J Magn Reson Imaging. 2007; 25:479–487.21. Tomura N, Narita K, Takahashi S, Otani T, Sakuma I, Yasuda K, et al. Contrast-enhanced multi-shot echo-planar FLAIR in the depiction of metastatic tumors of the brain: comparison with contrast-enhanced spin-echo T1-weighted imaging. Acta Radiol. 2007; 48:1032–1037.22. Ahn SJ, Chung TS, Chang JH, Lee SK. The added value of double dose gadolinium enhanced 3D T2 fluid-attenuated inversion recovery for evaluating small brain metastases. Yonsei Med J. 2014; 55:1231–1237.23. Ercan N, Gultekin S, Celik H, Tali TE, Oner YA, Erbas G. Diagnostic value of contrast-enhanced fluid-attenuated inversion recovery MR imaging of intracranial metastases. AJNR Am J Neuroradiol. 2004; 25:761–765.24. Sasiadek M, Wojtek P, Sokołwska D, Konopka M, Pieniazek P, Zimny A. Evaluation of contrast-enhanced FLAIR sequence in MR assessment of intracranial tumours. Med Sci Monit. 2004; 10:Suppl 3. 94–100.25. Zhou ZR, Shen TZ, Chen XR, Peng WJ. Diagnostic value of contrast-enhanced fluid-attenuated inversion-recovery MRI for intracranial tumors in comparison with post-contrast T1W spin-echo MRI. Chin Med J (Engl). 2006; 119:467–447.26. Splendiani A, Puglielli E, De Amicis R, Necozione S, Masciocchi C, Gallucci M. Contrast-enhanced FLAIR in the early diagnosis of infectious meningitis. Neuroradiology. 2005; 47:591–598.27. Parmar H, Sitoh YY, Anand P, Chua V, Hui F. Contrast-enhanced flair imaging in the evaluation of infectious leptomeningeal diseases. Eur J Radiol. 2006; 58:89–95.28. Kim HJ. Importance of contrast-enhanced fluid-attenuated inversion recovery imaging to detect paradoxical expansion of tuberculoma. Int J Infect Dis. 2014; 24:37–39.29. Lee JS, Park JK, Kim SH, Jeong SY, Kim BS, Choi G, et al. Usefulness of contrast enhanced FLAIR imaging for predicting the severity of meningitis. J Neurol. 2014; 261:817–822.30. Ahmad A, Azad S, Azad R. Differentiation of Leptomeningeal and Vascular Enhancement on Post-contrast FLAIR MRI Sequence: Role in Early Detection of Infectious Meningitis. J Clin Diagn Res. 2015; 9:TC08–TC12.31. Vaswani AK, Nizamani WM, Ali M, Aneel G, Shahani BK, Hussain S. Diagnostic Accuracy of Contrast-Enhanced FLAIR Magnetic Resonance Imaging in Diagnosis of Meningitis Correlated with CSF Analysis. ISRN Radiol. 2014; 2014:578986.32. Singh SK, Leeds NE, Ginsberg LE. MR imaging of leptomeningeal metastases: comparison of three sequences. AJNR Am J Neuroradiol. 2002; 23:817–821.33. Griffiths PD, Coley SC, Romanowski CA, Hodgson T, Wilkinson ID. Contrast-enhanced fluid-attenuated inversion recovery imaging for leptomeningeal disease in children. AJNR Am J Neuroradiol. 2003; 24:719–723.34. Koide R, Isoo A, Ishii K, Uruha A, Bandoh M. Rheumatoid leptomeningitis: rare complication of rheumatoid arthritis. Clin Rheumatol. 2009; 28:1117–1119.35. Shimada K, Matsui T, Kawakami M, Hayakawa H, Futami H, Michishita K, et al. Diffuse chronic leptomeningitis with seropositive rheumatoid arthritis: report of a case successfully treated as rheumatoid leptomeningitis. Mod Rheumatol. 2009; 19:556–562.36. Matsushima M, Yaguchi H, Niino M, Akimoto-Tsuji S, Yabe I, Onishi K, et al. MRI and pathological findings of rheumatoid meningitis. J Clin Neurosci. 2010; 17:129–132.37. Kamran S, Bener AB, Alper D, Bakshi R. Role of fluid-attenuated inversion recovery in the diagnosis of meningitis: comparison with contrast-enhanced magnetic resonance imaging. J Comput Assist Tomogr. 2004; 28:68–72.38. Meltzer CC, Fukui MB, Kanal E, Smirniotopoulos JG. MR imaging of the meninges. Part I. Normal anatomic features and nonneoplastic disease. Radiology. 1996; 201:297–308.39. Elster AD, DiPersio DA. Cranial postoperative site: assessment with contrast-enhanced MR imaging. Radiology. 1990; 174:93–98.40. Sinclair AG, Scoffings DJ. Imaging of the post-operative cranium. Radiographics. 2010; 30:461–482.41. Kim SC, Park SW, Ryoo I, Jung SC, Yun TJ, Choi SH, et al. Contrast-enhanced FLAIR (fluid-attenuated inversion recovery) for evaluating mild traumatic brain injury. PLoS One. 2014; 9:e102229.42. Kanamalla US, Baker KB, Boyko OB. Gadolinium diffusion into subdural space: visualization with FLAIR MR imaging. AJR Am J Roentgenol. 2001; 176:1604–1605.43. Fink KR, Fink JR. Imaging of brain metastases. Surg Neurol Int. 2013; 4:Suppl 4. S209–S219.44. Barajas RF Jr, Cha S. Imaging diagnosis of brain metastasis. Prog Neurol Surg. 2012; 25:55–73.45. Lee EK, Lee EJ, Kim MS, Park HJ, Park NH, Park S 2nd, et al. Intracranial metastases: spectrum of MR imaging findings. Acta Radiol. 2012; 53:1173–1185.46. Tsuchiya K, Katase S, Yoshino A, Hachiya J. Pre- and postcontrast FLAIR MR imaging in the diagnosis of intracranial meningeal pathology. Radiat Med. 2000; 18:363–368.47. Oguz KK, Cila A. Rim enhancement of meningiomas on fast FLAIR imaging. Neuroradiology. 2003; 45:78–81.48. Oner AY, Tokgöz N, Tali ET, Uzun M, Isik S. Imaging meningiomas: is there a need for post-contrast FLAIR? Clin Radiol. 2005; 60:1300–1305.49. Enokizono M, Morikawa M, Matsuo T, Hayashi T, Horie N, Honda S, et al. The rim pattern of meningioma on 3D FLAIR imaging: correlation with tumor-brain adhesion and histological grading. Magn Reson Med Sci. 2014; 13:251–260.50. Gebarski SS, Telian SA, Niparko JK. Enhancement along the normal facial nerve in the facial canal: MR imaging and anatomic correlation. Radiology. 1992; 183:391–394.51. Hong HS, Yi BH, Cha JG, Park SJ, Kim DH, Lee HK, et al. Enhancement pattern of the normal facial nerve at 3.0 T temporal MRI. Br J Radiol. 2010; 83:118–121.52. Lim HK, Lee JH, Hyun D, Park JW, Kim JL, Lee HY, et al. MR diagnosis of facial neuritis: diagnostic performance of contrast-enhanced 3D-FLAIR technique compared with contrast-enhanced 3D-T1-fast-field echo with fat suppression. AJNR Am J Neuroradiol. 2012; 33:779–783.53. Hyun D, Lim HK, Park JW, Kim JL, Lee HY, Park SC, et al. Enhancement Pattern of the Normal Facial Nerve on Three-Dimensional (3D)-Fluid Attenuated Inversion Recovery (FLAIR) Sequence at 3.0 T MR Units. J Korean Soc Magn Reson Med. 2012; 16:25–30.54. Latour LL, Kang DW, Ezzeddine MA, Chalela JA, Warach S. Early blood-brain barrier disruption in human focal brain ischemia. Ann Neurol. 2004; 56:468–477.55. Dechambre SD, Duprez T, Grandin CB, Lecouvet FE, Peeters A, Cosnard G. High signal in cerebrospinal fluid mimicking subarachnoid haemorrhage on FLAIR following acute stroke and intravenous contrast medium. Neuroradiology. 2000; 42:608–611.56. Warach S, Latour LL. Evidence of reperfusion injury, exacerbated by thrombolytic therapy, in human focal brain ischemia using a novel imaging marker of early blood-brain barrier disruption. Stroke. 2004; 35:11 Suppl 1. 2659–2661.57. Henning EC, Latour LL, Warach S. Verification of enhancement of the CSF space, not parenchyma, in acute stroke patients with early blood-brain barrier disruption. J Cereb Blood Flow Metab. 2008; 28:882–886.58. Kidwell CS, Latour L, Saver JL, Alger JR, Starkman S, Duckwiler G, et al. Thrombolytic toxicity: blood brain barrier disruption in human ischemic stroke. Cerebrovasc Dis. 2008; 25:338–343.59. Barr TL, Latour LL, Lee KY, Schaewe TJ, Luby M, Chang GS, et al. Blood-brain barrier disruption in humans is independently associated with increased matrix metalloproteinase-9. Stroke. 2010; 41:e123–e128.60. Batra A, Latour LL, Ruetzler CA, Hallenbeck JM, Spatz M, Warach S, et al. Increased plasma and tissue MMP levels are associated with BCSFB and BBB disruption evident on post-contrast FLAIR after experimental stroke. J Cereb Blood Flow Metab. 2010; 30:1188–1199.61. Ostwaldt AC, Rozanski M, Schaefer T, Ebinger M, Jungehülsing GJ, Villringer K, et al. Hyperintense acute reperfusion marker is associated with higher contrast agent dosage in acute ischaemic stroke. Eur Radiol. 2015; 25:3161–3166.62. Rozanski M, Ebinger M, Schmidt WU, Hotter B, Pittl S, Heuschmann PU, et al. Hyperintense acute reperfusion marker on FLAIR is not associated with early haemorrhagic transformation in the elderly. Eur Radiol. 2010; 20:2990–2996.63. Ogami R, Nakahara T, Hamasaki O, Araki H, Kurisu K. Cerebrospinal fluid enhancement on fluid attenuated inversion recovery images after carotid artery stenting with neuroprotective balloon occlusions: hemodynamic instability and blood-brain barrier disruption. Cardiovasc Intervent Radiol. 2011; 34:936–941.64. Wilkinson ID, Griffiths PD, Hoggard N, Cleveland TJ, Gaines PA, Venables GS. Unilateral leptomeningeal enhancement after carotid stent insertion detected by magnetic resonance imaging. Stroke. 2000; 31:848–851.65. Michel E, Liu H, Remley KB, Martin AJ, Madison MT, Kucharczyk J, et al. Perfusion MR neuroimaging in patients undergoing balloon test occlusion of the internal carotid artery. AJNR Am J Neuroradiol. 2001; 22:1590–1596.66. Merino JG, Latour LL, Tso A, Lee KY, Kang DW, Davis LA, et al. Blood-brain barrier disruption after cardiac surgery. AJNR Am J Neuroradiol. 2013; 34:518–523.67. Okamura T, Ishibashi N, Zurakowski D, Jonas RA. Cardiopulmonary bypass increases permeability of the blood-cerebrospinal fluid barrier. Ann Thorac Surg. 2010; 89:187–194.68. Seo DW, Na DG, Na DL, Moon SY, Hong SB. Subcortical hypointensity in partial status epilepticus associated with nonketotic hyperglycemia. J Neuroimaging. 2003; 13:259–263.69. Bathla G, Policeni B, Agarwal A. Neuroimaging in patients with abnormal blood glucose levels. AJNR Am J Neuroradiol. 2014; 35:833–840.70. Arsenault TM, King BF, Marsh JW Jr, Goodman JA, Weaver AL, Wood CP, et al. Systemic gadolinium toxicity in patients with renal insufficiency and renal failure: retrospective analysis of an initial experience. Mayo Clin Proc. 1996; 71:1150–1154.71. Rai AT, Hogg JP. Persistence of gadolinium in CSF: a diagnostic pitfall in patients with end-stage renal disease. AJNR Am J Neuroradiol. 2001; 22:1357–1361.72. Maramattom BV, Manno EM, Wijdicks EF, Lindell EP. Gadolinium encephalopathy in a patient with renal failure. Neurology. 2005; 64:1276–1278.73. Morris JM, Miller GM. Increased signal in the subarachnoid space on fluid-attenuated inversion recovery imaging associated with the clearance dynamics of gadolinium chelate: a potential diagnostic pitfall. AJNR Am J Neuroradiol. 2007; 28:1964–1967.74. Ong EM, Yeh IB. High signal in the cerebrospinal fluid following prior gadolinium administration in a patient with renal impairment. Singapore Med J. 2007; 48:e296–e298.75. Shellock FG, Kanal E. Safety of magnetic resonance imaging contrast agents. J Magn Reson Imaging. 1999; 10:477–484.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Contrast-enhanced Fast Fluid-attenuated Inversion Recovery MR Imaging in Patients with Brain Tumors
- Does Multiphasic Contrast Enhanced Fluid Attenuated Inversion Recovery Magnetic Resonance Imaging Enhance the Detectability of Small Intracerebral Metastases?
- Early Diagnosis of Aseptic Meningitis in Ramsay Hunt Syndrome on 10-Minute Delayed CE 3D FLAIR Image: a Case Report
- Comparison of Fluid-Attenuated Inversion-Recovery Magnetic Resonance Imaging with Computed Tomography in Acute Intraventricular Hemorrhage
- Reversible Cerebral Vasoconstriction Syndrome Presenting as Transient Vessel Wall Enhancement on Contrast-Enhanced Fluid-Attenuated Inversion Recovery Images: A Case Report and Literature Review