Korean J Radiol.
2016 Feb;17(1):111-116. 10.3348/kjr.2016.17.1.111.
Digital Subtraction Cystography for Detection of Communicating Holes of Spinal Extradural Arachnoid Cysts
- Affiliations
-
- 1Department of Radiology and Center for Imaging Science, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 06351, Korea. jwjwkwon@gmail.com
- 2Department of Medical Device Management and Research, SAIHST, Sungkyunkwan University, Seoul 06351, Korea.
- 3Department of Neurosurgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 06351, Korea.
- KMID: 2351170
- DOI: http://doi.org/10.3348/kjr.2016.17.1.111
Abstract
OBJECTIVE
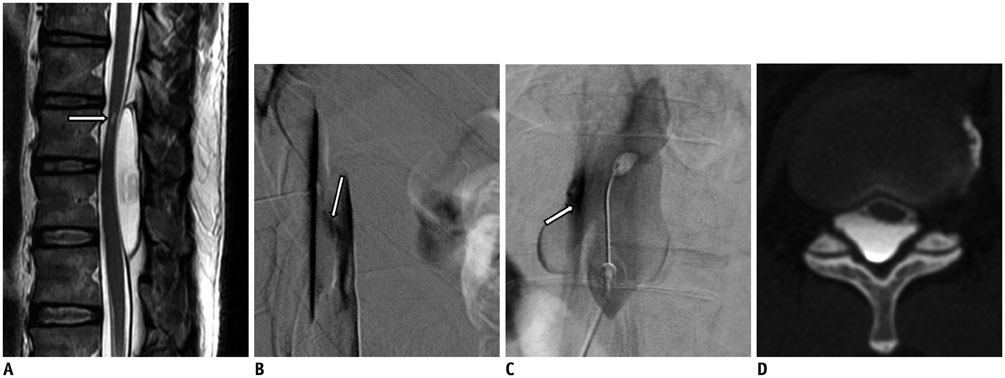
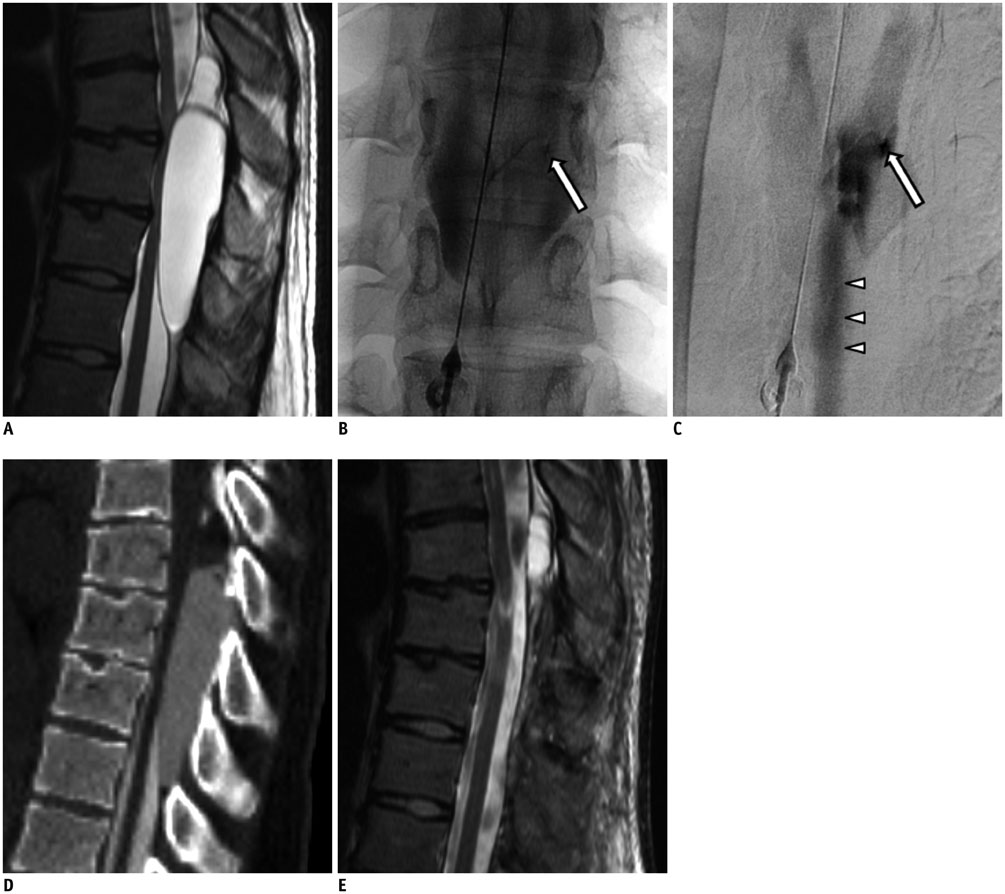
The purpose of this study was to demonstrate the usefulness of digital subtraction cystography to identify communicating holes between a spinal extradural arachnoid cyst (SEAC) and the subarachnoid space prior to cyst removal and hole closure.
MATERIALS AND METHODS
Six patients with SEAC were enrolled in this retrospective study. Digital subtraction cystography and subsequent CT myelography were performed for every patient. The presence and location of the communicating holes on cystography were documented. We evaluated the MRI characteristics of the cysts, including location, size, and associated spinal cord compression; furthermore, we reviewed cystographic images, CT myelograms, procedural reports, and medical records for analysis. If surgery was performed after cystography, intraoperative findings were compared with preoperative cystography.
RESULTS
The location of the communicating hole between the arachnoid cyst and the subarachnoid space was identified by digital subtraction cystography in all cases (n = 6). Surgical resection of SEAC was performed in 4 patients, and intraoperative location of the communicating hole exactly corresponded to the preoperative identification.
CONCLUSION
Fluoroscopic-guided cystography for SEAC accurately demonstrates the presence and location of dural defects. Preoperative digital subtraction cystography is useful for detection of a communicating hole between a cyst and the subarachnoid space.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Surgical Treatment of Ten Adults with Spinal Extradural Meningeal Cysts in the Thoracolumbar Spine
Feifan Xu, Fengzeng Jian, Liang Li, Jian Guan, Zan Chen
J Korean Neurosurg Soc. 2021;64(2):238-246. doi: 10.3340/jkns.2020.0244.
Reference
-
1. Liu JK, Cole CD, Kan P, Schmidt MH. Spinal extradural arachnoid cysts: clinical, radiological, and surgical features. Neurosurg Focus. 2007; 22:E6.2. McCrum C, Williams B. Spinal extradural arachnoid pouches. Report of two cases. J Neurosurg. 1982; 57:849–852.3. Congia S, Coraddu M, Tronci S, Nurchi G, Fiaschi A. Myelographic and MRI appearances of a thoracic spinal extradural arachnoid cyst of the spine with extra- and intraspinal extension. Neuroradiology. 1992; 34:444–446.4. Ishibe T, Senzoku F, Ikeda N, Kamba Y, Mikawa Y. Detection of the communicating hole(s) of spinal extradural arachnoid cysts using time-spatial labeling inversion pulse magnetic resonance imaging. Spine (Phila Pa 1976). 2014; 39:E1394–E1397.5. Rimmelin A, Clouet PL, Salatino S, Kehrli P, Maitrot D, Stephan M, et al. Imaging of thoracic and lumbar spinal extradural arachnoid cysts: report of two cases. Neuroradiology. 1997; 39:203–206.6. Doita M, Nishida K, Miura J, Takada T, Kurosaka M, Fujii M. Kinematic magnetic resonance imaging of a thoracic spinal extradural arachnoid cyst: an alternative suggestion for exacerbation of symptoms during straining. Spine (Phila Pa 1976). 2003; 28:E229–E233.7. Tomii M, Mizuno J, Takeda M, Matsushima T, Itoh Y, Numazawa S, et al. Thoracolumbar extradural arachnoid cyst--three surgical case reports. Neurol Med Chir (Tokyo). 2013; 53:129–133.8. Neo M, Koyama T, Sakamoto T, Fujibayashi S, Nakamura T. Detection of a dural defect by cinematic magnetic resonance imaging and its selective closure as a treatment for a spinal extradural arachnoid cyst. Spine (Phila Pa 1976). 2004; 29:E426–E430.9. Miyamoto M, Kim K, Matsumoto R, Isobe M, Isu T. Utility of preoperative magnetic resonance imaging myelography for identifying dural defects in patients with spinal extradural arachnoid cysts: case report. Neurosurgery. 2006; 59:E941. discussion E941.10. Funao H, Nakamura M, Hosogane N, Watanabe K, Tsuji T, Ishii K, et al. Surgical treatment of spinal extradural arachnoid cysts in the thoracolumbar spine. Neurosurgery. 2012; 71:278–284. discussion 28411. Yoshida H, Takai K, Taniguchi M. Leakage detection on CT myelography for targeted epidural blood patch in spontaneous cerebrospinal fluid leaks: calcified or ossified spinal lesions ventral to the thecal sac. J Neurosurg Spine. 2014; 21:432–441.12. Qi W, Zhao L, Fang J, Chang X, Xu Y. Clinical characteristics and treatment strategies for idiopathic spinal extradural arachnoid cysts: a single-center experience. Acta Neurochir (Wien). 2015; 157:539–545.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Symptomatic Large Spinal Extradural Arachnoid Cyst: A Case Report
- Multiple Extradural Arachnoid Cyst : A Case Report
- Surgical Management of Thoracic Spinal Extradural Arachnoid Cysts: A Case Report
- Extradural Spinal Arachnoid Cyst as a Cause of Cauda Equina Syndrome in a Child
- A Case of a Thoracic Spinal Intradural Arachnoid Cyst with Chest Pain