Korean J Radiol.
2016 Feb;17(1):69-78. 10.3348/kjr.2016.17.1.69.
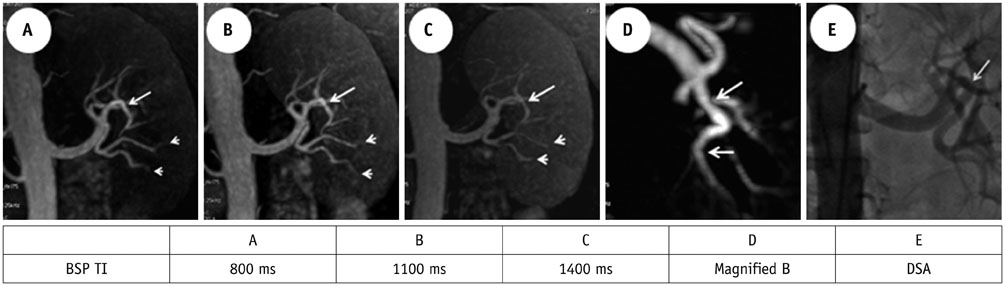
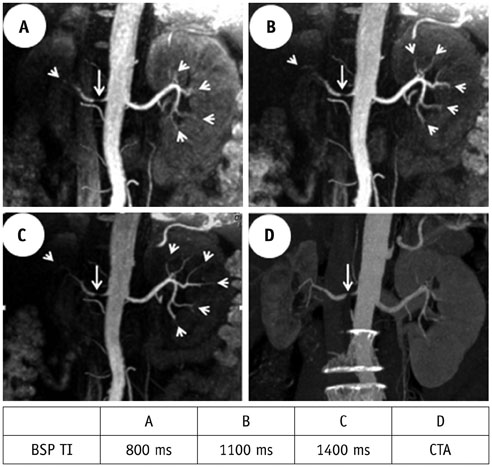
Optimal Blood Suppression Inversion Time Based on Breathing Rates and Heart Rates to Improve Renal Artery Visibility in Spatial Labeling with Multiple Inversion Pulses: A Preliminary Study
- Affiliations
-
- 1Department of Radiology, Xiangya Hospital, Central South University, Changsha 410008, China. liwenzheng0731@163.com
- 2GE Healthcare, Waukesha, WI 53188, USA.
- KMID: 2351165
- DOI: http://doi.org/10.3348/kjr.2016.17.1.69
Abstract
OBJECTIVE
To determine whether an optimal blood suppression inversion time (BSP TI) can boost arterial visibility and whether the optimal BSP TI is related to breathing rate (BR) and heart rate (HR) for hypertension subjects in spatial labeling with multiple inversion pulses (SLEEK).
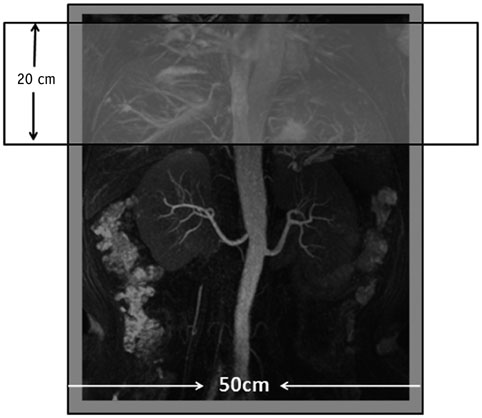
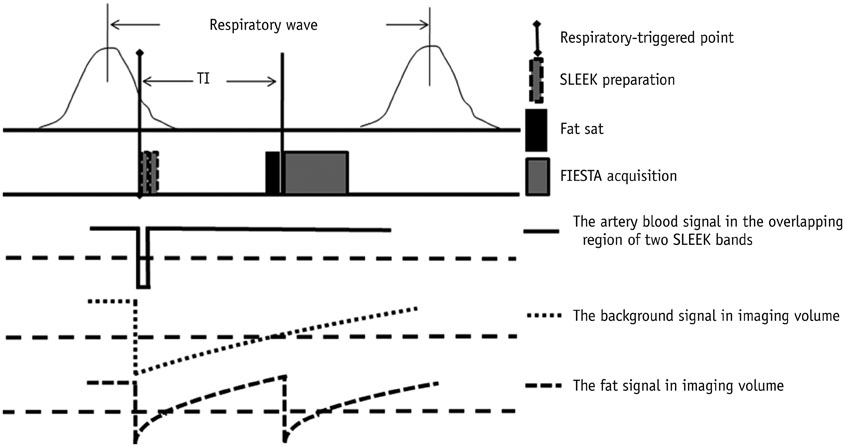
MATERIALS AND METHODS
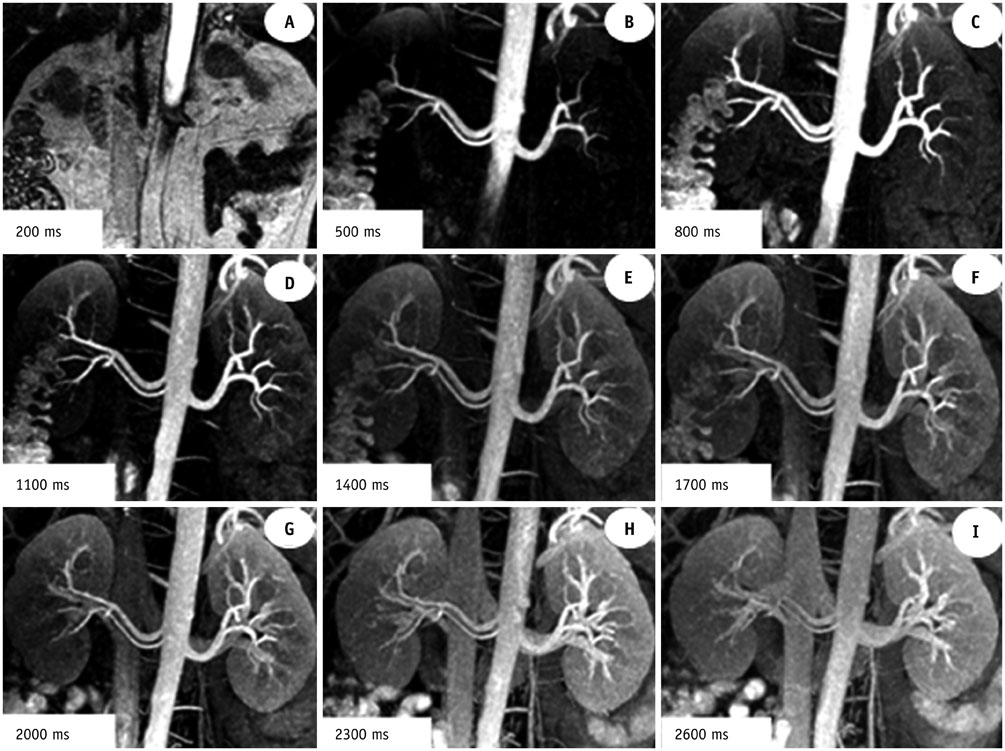
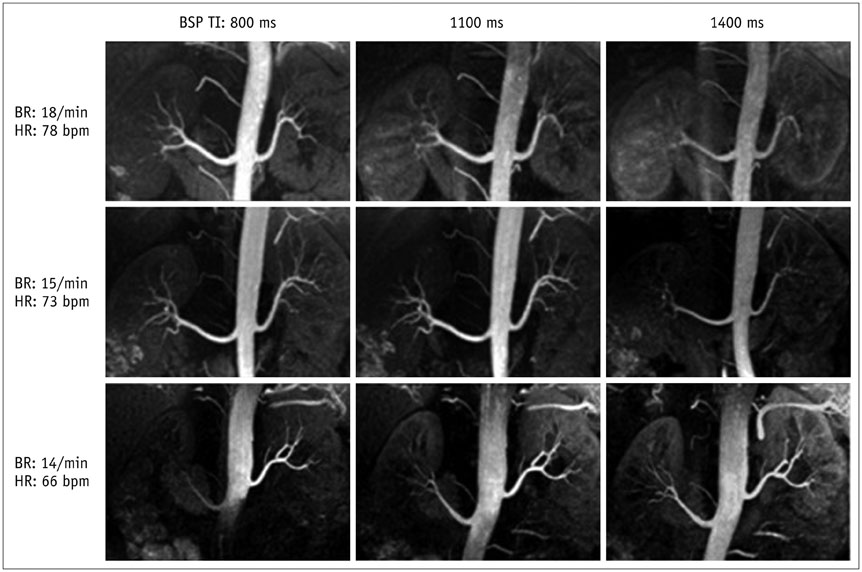
This prospective study included 10 volunteers and 93 consecutive hypertension patients who had undergone SLEEK at 1.5T MRI system. Firstly, suitable BSP TIs for displaying clearly renal artery were determined in 10 volunteers. Secondly, non-contrast enhanced magnetic resonance angiography with the suitable BSP TIs were performed on those hypertension patients. Then, renal artery was evaluated and an optimal BSP TI to increase arterial visibility was determined for each patient. Patients' BRs and HRs were recorded and their relationships with the optimal BSP TI were analyzed.
RESULTS
The optimal BSP TI was negatively correlated with BR (r1 = -0.536, P1 < 0.001; and r2 = -0.535, P2 < 0.001) and HR (r1 = -0.432, P1 = 0.001; and r2 = -0.419, P2 = 0.001) for 2 readers (kappa = 0.93). For improving renal arterial visibility, BSP TI = 800 ms could be applied as the optimal BSP TI when the 95% confidence interval were 17-19/min (BR1) and 74-82 bpm (HR1) for reader#1 and 17-19/min (BR2) and 74-83 bpm (HR2) for reader#2; BSP TI = 1100 ms while 14-15/min (BR1, 2) and 71-76 bpm (HR1, 2) for both readers; and BSP TI = 1400 ms when 13-16/min (BR1) and 63-68 bpm (HR1) for reader#1 and 14-15/min (BR2) and 64-70 bpm (HR2) for reader#2.
CONCLUSION
In SLEEK, BSP TI is affected by patients' BRs and HRs. Adopting the optimal BSP TI based on BR and HR can improve the renal arterial visibility and consequently the working efficiency.
Keyword
MeSH Terms
Figure
Reference
-
1. Völk M, Strotzer M, Lenhart M, Manke C, Nitz WR, Seitz J, et al. Time-resolved contrast-enhanced MR angiography of renal artery stenosis: diagnostic accuracy and interobserver variability. AJR Am J Roentgenol. 2000; 174:1583–1588.2. Utsunomiya D, Awai K, Tamura Y, Nishiharu T, Urata J, Sakamoto T, et al. 16-MDCT aortography with a low-dose contrast material protocol. AJR Am J Roentgenol. 2006; 186:374–378.3. Nchimi A, Biquet JF, Brisbois D, Reginster P, Bouali K, Saive C, et al. Duplex ultrasound as first-line screening test for patients suspected of renal artery stenosis: prospective evaluation in high-risk group. Eur Radiol. 2003; 13:1413–1419.4. Sadowski EA, Bennett LK, Chan MR, Wentland AL, Garrett AL, Garrett RW, et al. Nephrogenic systemic fibrosis: risk factors and incidence estimation. Radiology. 2007; 243:148–157.5. Lanzman RS, Voiculescu A, Walther C, Ringelstein A, Bi X, Schmitt P, et al. ECG-gated nonenhanced 3D steady-state free precession MR angiography in assessment of transplant renal arteries: comparison with DSA. Radiology. 2009; 252:914–921.6. Mohrs OK, Petersen SE, Schulze T, Zieschang M, Küx H, Schmitt P, et al. High-resolution 3D unenhanced ECG-gated respiratory-navigated MR angiography of the renal arteries: comparison with contrast-enhanced MR angiography. AJR Am J Roentgenol. 2010; 195:1423–1428.7. Tang H, Wang Z, Wang L, Hu X, Wang Q, Li Z, et al. Depiction of transplant renal vascular anatomy and complications: unenhanced MR angiography by using spatial labeling with multiple inversion pulses. Radiology. 2014; 271:879–887.8. Shonai T, Takahashi T, Ikeguchi H, Miyazaki M, Amano K, Yui M. Improved arterial visibility using short-tau inversion-recovery (STIR) fat suppression in non-contrast-enhanced time-spatial labeling inversion pulse (Time-SLIP) renal MR angiography (MRA). J Magn Reson Imaging. 2009; 29:1471–1477.9. Xu JL, Shi DP, Li YL, Zhang JL, Zhu SC, Shen H. Non-enhanced MR angiography of renal artery using inflow-sensitive inversion recovery pulse sequence: a prospective comparison with enhanced CT angiography. Eur J Radiol. 2011; 80:e57–e63.10. Utsunomiya D, Miyazaki M, Nomitsu Y, Komeda Y, Okigawa T, Urata J, et al. Clinical role of non-contrast magnetic resonance angiography for evaluation of renal artery stenosis. Circ J. 2008; 72:1627–1630.11. Parienty I, Rostoker G, Jouniaux F, Piotin M, Admiraal-Behloul F, Miyazaki M. Renal artery stenosis evaluation in chronic kidney disease patients: nonenhanced time-spatial labeling inversion-pulse three-dimensional MR angiography with regulated breathing versus DSA. Radiology. 2011; 259:592–601.12. Maki JH, Wilson GJ, Eubank WB, Glickerman DJ, Millan JA, Hoogeveen RM. Navigator-gated MR angiography of the renal arteries: a potential screening tool for renal artery stenosis. AJR Am J Roentgenol. 2007; 188:W540–W546.13. Liu X, Berg N, Sheehan J, Bi X, Weale P, Jerecic R, et al. Renal transplant: nonenhanced renal MR angiography with magnetization-prepared steady-state free precession. Radiology. 2009; 251:535–542.14. Clemente A, Macchi V, Porzionato A, Stecco C, De Caro R, Morra A. CTA and 2D-3D post-processing: radiological signs of fibromuscular dysplasia of renal artery. Surg Radiol Anat. 2009; 31:25–29.15. Sabharwal R, Vladica P, Coleman P. Multidetector spiral CT renal angiography in the diagnosis of renal artery fibromuscular dysplasia. Eur J Radiol. 2007; 61:520–527.16. Fraioli F, Catalano C, Bertoletti L, Danti M, Fanelli F, Napoli A, et al. Multidetector-row CT angiography of renal artery stenosis in 50 consecutive patients: prospective interobserver comparison with DSA. Radiol Med. 2006; 111:459–468.17. Pei Y, Shen H, Li J, Zhang H, Xia L, Wang L, et al. Evaluation of renal artery in hypertensive patients by unenhanced MR angiography using spatial labeling with multiple inversion pulses sequence and by CT angiography. AJR Am J Roentgenol. 2012; 199:1142–1148.18. Dinter DJ, Buesing KA, Diehl SJ, Neff KW. Blood volume flow quantification of the brain-supplying circulation in fibromuscular dysplasia using 2D cine phase-contrast MRI. Br J Radiol. 2009; 82:459–467.19. Vasbinder GB, Maki JH, Nijenhuis RJ, Leiner T, Wilson GJ, Kessels AG, et al. Motion of the distal renal artery during three-dimensional contrast-enhanced breath-hold MRA. J Magn Reson Imaging. 2002; 16:685–696.20. Hori M, Shiraga N, Watanabe Y, Aoki S, Isono S, Yui M, et al. Time-resolved three-dimensional magnetic resonance digital subtraction angiography without contrast material in the brain: Initial investigation. J Magn Reson Imaging. 2009; 30:214–218.21. Momen A, Handly B, Kunselman A, Leuenberger UA, Sinoway LI. Influence of sex and active muscle mass on renal vascular responses during static exercise. Am J Physiol Heart Circ Physiol. 2006; 291:H121–H126.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Practical Considerations of Arterial Spin Labeling MRI for Measuring the Multi-slice Perfusion in the Human Brain
- Spontaneous Restoration of Unrecognized Uterine Inversion
- Left Gastric Vein Visualization with Hepatopetal Flow Information in Healthy Subjects Using Non-Contrast-Enhanced Magnetic Resonance Angiography with Balanced Steady-State Free-Precession Sequence and Time-Spatial Labeling Inversion Pulse
- Incidence and Karyotypes According to Each Chromosome in 13 Cases with Inversion
- A Potential Diagnostic Pitfall in the Differentiation of Hemorrhagic and Fatty Lesions Using Short Inversion Time Inversion Recovery: a Case Report