Recent Changes in the Incidence of Bronchopulmonary Dysplasia among Very-Low-Birth-Weight Infants in Korea
- Affiliations
-
- 1Department of Pediatrics, CHA University, Seongnam, Korea.
- 2Graduate School of Public Health and Institute of Health and Environment, Seoul National University, Seoul, Korea.
- 3Department of Pediatrics, Chonnam National University Hospital, Gwangju, Korea.
- 4Department of Pediatrics, Seoul National University Bundang Hospital, Seongnam, Korea. beyil@snu.ac.kr
- KMID: 2351140
- DOI: http://doi.org/10.3346/jkms.2015.30.S1.S81
Abstract
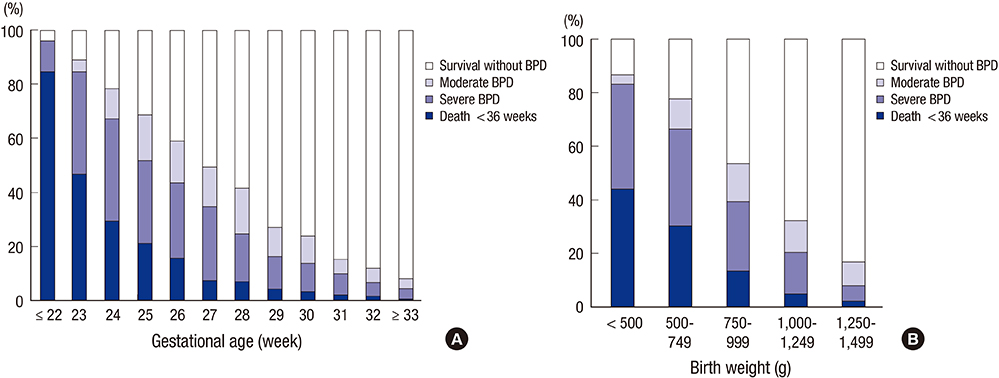
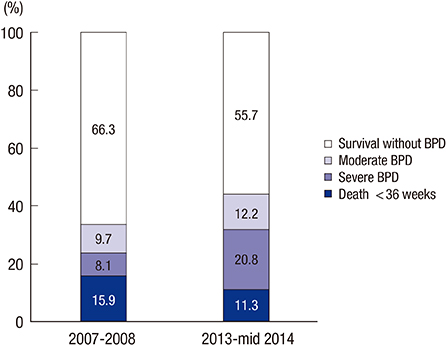
- We investigated the incidence of bronchopulmonary dysplasia (BPD) in very-low-birth-weight (VLBW) infants in Korea using the Korean Neonatal Network (KNN) data. In total, 2,386 VLBW infants born from January 2013 to June 2014 were prospectively registered. BPD was defined as supplemental oxygen or positive pressure support at 36 weeks postmenstrual age (PMA). The overall incidence of BPD was 28.9%, and the overall mortality rate in the neonatal intensive care units (NICUs) was 11.9%. To investigate recent changes in the incidence of BPD among VLBW infants, we compared the BPD rate in the present study with the latest nationwide retrospective survey conducted between 2007 and 2008. For comparison, we selected infants (23-31 weeks of gestation) (n=1,990) to adjust for the same conditions with the previous survey in 2007-2008 (n=3,841). Among the limited data on VLBW infants (23-31 weeks of gestation), the incidence of BPD increased by 85% (from 17.8% to 33.0%) and the mortality rate in the NICU decreased by 31.4% (from 18.8% to 12.9%) compared to those in the study conducted in 2007-2008. The current trend of increase in the incidence of BPD among infants can be attributed to the increase in the survival rate of VLBW infants.
Keyword
MeSH Terms
-
Apgar Score
Bronchopulmonary Dysplasia/*epidemiology/mortality
Databases, Factual
Female
Gestational Age
Humans
Incidence
Infant
Infant Mortality
Infant, Newborn
*Infant, Very Low Birth Weight
Intensive Care Units, Neonatal
Male
Odds Ratio
Republic of Korea/epidemiology
Retrospective Studies
Risk Factors
Survival Rate
Figure
Cited by 3 articles
-
Neonatal Outcomes of Very Low Birth Weight Infants in Korean Neonatal Network from 2013 to 2016
Jang Hoon Lee, O Kyu Noh, Yun Sil Chang,
J Korean Med Sci. 2019;34(5):. doi: 10.3346/jkms.2019.34.e40.Association between Birth Weight and Bronchopulmonary Dysplasia in <32 Weeks of Singleton Infants
Kee Hyun Cho, Jaewoo An, Heui Seung Jo, Kyu Hyung Lee
Perinatology. 2017;28(2):35-40. doi: 10.14734/PN.2017.28.2.35.Two cases of extracorporeal membrane oxygenation for ventilator-dependent infants with bronchopulmonary dysplasia and pulmonary hypertension
Yong Hyuk Jeon, Wonjin Jang, Hye Won Kwon, Sungkyu Cho, Jae Gun Kwak, In Kyung Lee, Kyeong Hun Lee, June Dong Park, Bongjin Lee
Pediatr Emerg Med J. 2024;11(2):91-97. doi: 10.22470/pemj.2023.00878.
Reference
-
1. de Kleine MJ, den Ouden AL, Kollée LA, Ilsen A, van Wassenaer AG, Brand R, Verloove-Vanhorick SP. Lower mortality but higher neonatal morbidity over a decade in very preterm infants. Paediatr Perinat Epidemiol. 2007; 21:15–25.2. Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR, Bauer CR, Donovan EF, Korones SB, Laptook AR, et al. Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol. 2007; 196:147.e1–147.e8.3. Hahn WH, Chang JY, Chang YS, Shim KS, Bae CW. Recent trends in neonatal mortality in very low birth weight Korean infants: in comparison with Japan and the USA. J Korean Med Sci. 2011; 26:467–473.4. Soll RF. Prophylactic natural surfactant extract for preventing morbidity and mortality in preterm infants. Cochrane Database Syst Rev. 2000; CD000511.5. Jobe AH. Antenatal associations with lung maturation and infection. J Perinatol. 2005; 25:S31–S35.6. Van Marter LJ. Epidemiology of bronchopulmonary dysplasia. Semin Fetal Neonatal Med. 2009; 14:358–366.7. Kinsella JP, Greenough A, Abman SH. Bronchopulmonary dysplasia. Lancet. 2006; 367:1421–1431.8. Majnemer A, Riley P, Shevell M, Birnbaum R, Greenstone H, Coates AL. Severe bronchopulmonary dysplasia increases risk for later neurological and motor sequelae in preterm survivors. Dev Med Child Neurol. 2000; 42:53–60.9. Chang YS, Ahn SY, Park WS. Committee on Program and Planning and Advisory Committee of Korean Neonatal Network. The establishment of the Korean Neonatal Network (KNN). Neonatal Med. 2013; 20:169–178.10. Choi CW, Kim BI, Kim EK, Song ES, Lee JJ. Incidence of bronchopulmonary dysplasia in Korea. J Korean Med Sci. 2012; 27:914–921.11. Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001; 163:1723–1729.12. Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, Wrage LA, Poole K. National Institutes of Child Health and Human Development Neonatal Research Network. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005; 116:1353–1360.13. Sweet DG, Carnielli V, Greisen G, Hallman M, Ozek E, Plavka R, Saugstad OD, Simeoni U, Speer CP, Vento M, et al. European consensus guidelines on the management of neonatal respiratory distress syndrome in preterm infants--2013 update. Neonatology. 2013; 103:353–368.14. Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, Hale EC, Newman NS, Schibler K, Carlo WA, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010; 126:443–456.15. Ancel PY, Goffinet F, Kuhn P, Langer B, Matis J, Hernandorena X, Chabanier P, Joly-Pedespan L, Lecomte B, Vendittelli F, et al. Survival and morbidity of preterm children born at 22 through 34 weeks' gestation in France in 2011: results of the EPIPAGE-2 cohort study. JAMA Pediatr. 2015; 169:230–238.16. Isayama T, Lee SK, Mori R, Kusuda S, Fujimura M, Ye XY, Shah PS. Canadian Neonatal Network. Neonatal Research Network of Japan. Comparison of mortality and morbidity of very low birth weight infants between Canada and Japan. Pediatrics. 2012; 130:e957–e965.17. Farstad T, Bratlid D, Medbø S, Markestad T. Norwegian Extreme Prematurity Study Group. Bronchopulmonary dysplasia - prevalence, severity and predictive factors in a national cohort of extremely premature infants. Acta Paediatr. 2011; 100:53–58.18. Laughon MM, Langer JC, Bose CL, Smith PB, Ambalavanan N, Kennedy KA, Stoll BJ, Buchter S, Laptook AR, Ehrenkranz RA, et al. Prediction of bronchopulmonary dysplasia by postnatal age in extremely premature infants. Am J Respir Crit Care Med. 2011; 183:1715–1722.19. Ambalavanan N, Walsh M, Bobashev G, Das A, Levine B, Carlo WA, Higgins RD. NICHD Neonatal Research Network. Intercenter differences in bronchopulmonary dysplasia or death among very low birth weight infants. Pediatrics. 2011; 127:e106–e116.20. Eriksson L, Haglund B, Odlind V, Altman M, Ewald U, Kieler H. Perinatal conditions related to growth restriction and inflammation are associated with an increased risk of bronchopulmonary dysplasia. Acta Paediatr. 2015; 104:259–263.21. Zhang H, Fang J, Su H, Chen M. Risk factors for bronchopulmonary dysplasia in neonates born at </= 1500 g (1999-2009). Pediatr Int. 2011; 53:915–920.22. Klinger G, Sirota L, Lusky A, Reichman B. Bronchopulmonary dysplasia in very low birth weight infants is associated with prolonged hospital stay. J Perinatol. 2006; 26:640–644.23. Chess PR, D'Angio CT, Pryhuber GS, Maniscalco WM. Pathogenesis of bronchopulmonary dysplasia. Semin Perinatol. 2006; 30:171–178.24. The Executive Committee of Korean Neonatal Network. 2013 Korean Neonatal Network Annual Report. Cheongwon: Korea Centers for Disease Control and Prevention;2014.25. Shah PS, Lee SK, Lui K, Sjörs G, Mori R, Reichman B, Håkansson S, Feliciano LS, Modi N, Adams M, et al. The International Network for Evaluating Outcomes of very low birth weight, very preterm neonates (iNeo): a protocol for collaborative comparisons of international health services for quality improvement in neonatal care. BMC Pediatr. 2014; 14:110.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevention and Treatment of Bronchopulmonary Dysplasia
- Epidemiology, Clinical Characteristics, and Pathophysiology of Bronchopulmonary Dysplasia
- Recent progress in the understanding of clinical characteristics, epidemiology, and pathogenesis of new bronchopulmonary dysplasia
- Risk Factors of Bronchopulmonary Dysplasia and Prediction in Korea
- Rehospitalization of Low-birth-weight Infants Who Were Discharged from NICU