J Korean Med Sci.
2015 Oct;30(Suppl 1):S35-S44. 10.3346/jkms.2015.30.S1.S35.
Risk Factors for Cause-specific Mortality of Very-Low-Birth-Weight Infants in the Korean Neonatal Network
- Affiliations
-
- 1Department of Pediatrics, College of Medicine, Konyang University, Daejon, Korea.
- 2Department of Pediatrics, Kyung Hee University School of Medicine, Seoul, Korea.
- 3Office of Biostatistics, School of Medicine, Ajou University, Suwon, Korea.
- 4Department of Pediatrics, College of Medicine, Hanyang University, Seoul, Korea. crkim@hanyang.ac.kr
- KMID: 2351134
- DOI: http://doi.org/10.3346/jkms.2015.30.S1.S35
Abstract
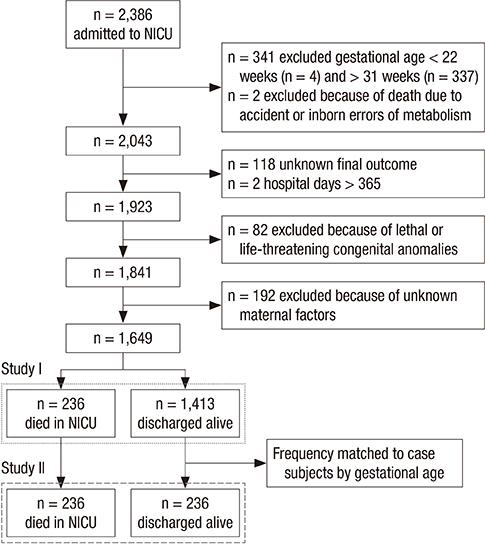
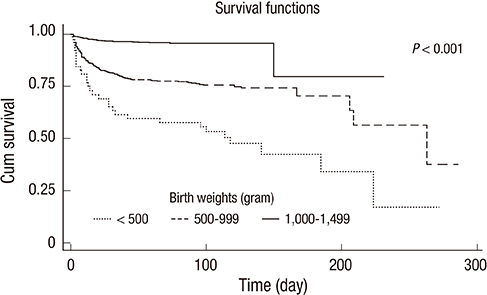
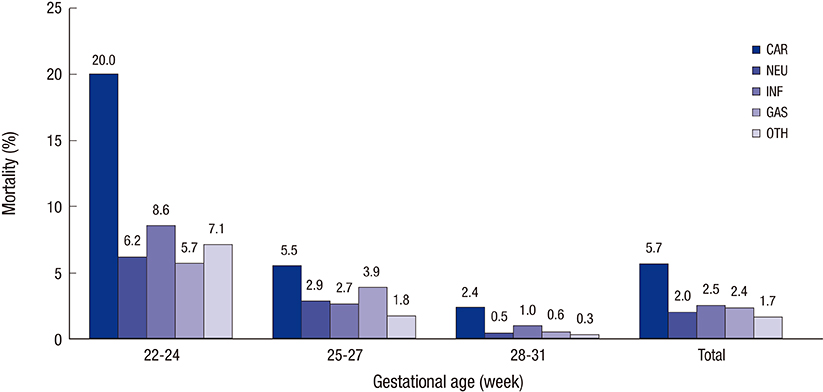
- This study attempted to assess the risk factors for mortality of very-low-birth-weight (VLBW) infants in the neonatal intensive care unit (NICU, n=2,386). Using data from the Korean Neonatal Network, we investigated infants with birth weights <1,500 g and gestational ages (GAs) of 22-31 weeks born between January 2013 and June 2014. Cases were defined as death at NICU discharge. Controls were randomly selected from live VLBW infants and frequency matched to case subjects by GA. Relevant variables were compared between the cases (n=236) and controls (n=236) by Cox proportional hazards regression to determine their associations with cause-specific mortality (cardiorespiratory, neurologic, infection, gastrointestinal, and others). In a Cox regression analysis, cardiorespiratory death were associated with a foreign mother (hazard ratio, HR, 4.33; 95% confidence interval, CI, 2.08-9.02), multiple gestation (HR, 1.65; 95% CI, 1.07-2.54), small for gestational age (HR, 2.06; 95% CI, 1.25-3.41), male gender (HR, 1.69; 95% CI, 1.10-2.60), Apgar score < or =3 at 5 min (HR, 1.97; 95% CI, 1.18-3.31), and delivery room resuscitation (HR, 2.60; 95% CI, 1.53-4.40). An Apgar score < or =3 at 5 min was also associated with neurological death (HR, 2.95; 95% CI, 1.29-6.73). Death due to neonatal infection was associated with outborn delivery (HR, 5.09; 95% CI, 1.46-17.74). Antenatal steroid and preterm premature rupture of membranes reduced risk of cardiorespiratory death (HR, 0.43; 95% CI, 0.27-0.67) and gastrointestinal death (HR, 0.30; 95% CI, 0.13-0.70), respectively. In conclusion, foreign mother, multiple gestation, small gestation age, male gender, Apgar score < or =3 at 5 min, and resuscitation in the delivery room are associated with cardiorespiratory mortality of VLBW infants in NICU. An Apgar score < or =3 at 5 min and outborn status are associated with neurological and infection mortality, respectively.
MeSH Terms
-
Apgar Score
Cohort Studies
Databases, Factual
Female
Gestational Age
Humans
Infant
*Infant Death
*Infant Mortality/trends
Infant, Newborn
Infant, Premature
Infant, Very Low Birth Weight
Intensive Care Units, Neonatal
Kaplan-Meier Estimate
Male
Pregnancy
Pregnancy, Multiple
Proportional Hazards Models
Republic of Korea
Resuscitation
Risk Factors
Sex Factors
Figure
Cited by 2 articles
-
Changes in neonatal outcomes in Korea
So Young Kim
J Korean Med Assoc. 2016;59(7):498-505. doi: 10.5124/jkma.2016.59.7.498.The Incidence and Survival Rate of Very Low Birth Weight Infants in Korea (2013–2016): A Comparison of the Statistics Korea and the Korean Neonatal Network and Improvements
Jisu Kim, Hye-Eun Kim, Kyung-Suk Lee, Sung-Hoon Chung, Yong-Sung Choi, Chong-Woo Bae, Korean Neonatal Network
Perinatology. 2019;30(1):1-7. doi: 10.14734/PN.2019.30.1.1.
Reference
-
1. Blencowe H, Cousens S, Chou D, Oestergaard M, Say L, Moller AB, Kinney M, Lawn J. Born Too Soon Preterm Birth Action Group. Born too soon: the global epidemiology of 15 million preterm births. Reprod Health. 2013; 10:S2.2. Lau C, Ambalavanan N, Chakraborty H, Wingate MS, Carlo WA. Extremely low birth weight and infant mortality rates in the United States. Pediatrics. 2013; 131:855–860.3. Hamilton BE, Hoyert DL, Martin JA, Strobino DM, Guyer B. Annual summary of vital statistics: 2010-2011. Pediatrics. 2013; 131:548–558.4. Velaphi SC, Mokhachane M, Mphahlele RM, Beckh-Arnold E, Kuwanda ML, Cooper PA. Survival of very-low-birth-weight infants according to birth weight and gestational age in a public hospital. S Afr Med J. 2005; 95:504–509.5. Evans N, Hutchinson J, Simpson JM, Donoghue D, Darlow B, Henderson-Smart D. Prenatal predictors of mortality in very preterm infants cared for in the Australian and New Zealand Neonatal Network. Arch Dis Child Fetal Neonatal Ed. 2007; 92:F34–F40.6. Kugelman A, Bader D, Lerner-Geva L, Boyko V, Levitzki O, Riskin A, Reichman B. Poor outcomes at discharge among extremely premature infants: a national population-based study. Arch Pediatr Adolesc Med. 2012; 166:543–550.7. Shankaran S, Fanaroff AA, Wright LL, Stevenson DK, Donovan EF, Ehrenkranz RA, Langer JC, Korones SB, Stoll BJ, Tyson JE, et al. Risk factors for early death among extremely low-birth-weight infants. Am J Obstet Gynecol. 2002; 186:796–802.8. Lee HC, Green C, Hintz SR, Tyson JE, Parikh NA, Langer J, Gould JB. Prediction of death for extremely premature infants in a population-based cohort. Pediatrics. 2010; 126:e644–e650.9. De Jesus LC, Pappas A, Shankaran S, Kendrick D, Das A, Higgins RD, Bell EF, Stoll BJ, Laptook AR, Walsh MC, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Risk factors for post-neonatal intensive care unit discharge mortality among extremely low birth weight infants. J Pediatr. 2012; 161:70–74.e1-2.10. Corchia C, Spagnolo A, de Vonderweid U, Zorzi C, Chiandotto V, Chiappe S, Colarizi P, Didato MA, Paludetto R. Clinical approach to the analysis of causes of death in the first two years of life of very-low-birth-weight infants in a multicentre setting. Paediatr Perinat Epidemiol. 1997; 11:44–56.11. Berrington JE, Hearn RI, Bythell M, Wright C, Embleton ND. Deaths in preterm infants: changing pathology over 2 decades. J Pediatr. 2012; 160:49–53.e1.12. Corchia C, Ferrante P, Da Frè M, Di Lallo D, Gagliardi L, Carnielli V, Miniaci S, Piga S, Macagno F, Cuttini M. Cause-specific mortality of very preterm infants and antenatal events. J Pediatr. 2013; 162:1125–1132. 1132.e1–1132.e4.13. Lim JS, Lim SW, Ahn JH, Song BS, Shim KS, Hwang IT. New Korean reference for birth weight by gestational age and sex: data from the Korean Statistical Information Service (2008-2012). Ann Pediatr Endocrinol Metab. 2014; 19:146–153.14. Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M. A United States national reference for fetal growth. Obstet Gynecol. 1996; 87:163–168.15. Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM. Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics. 1988; 82:527–532.16. Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001; 163:1723–1729.17. Bacak SJ, Baptiste-Roberts K, Amon E, Ireland B, Leet T. Risk factors for neonatal mortality among extremely-low-birth-weight infants. Am J Obstet Gynecol. 2005; 192:862–867.18. Fanaroff AA, Wright LL, Stevenson DK, Shankaran S, Donovan EF, Ehrenkranz RA, Younes N, Korones SB, Stoll BJ, Tyson JE, et al. Very-low-birth-weight outcomes of the National Institute of Child Health and Human Development Neonatal Research Network, May 1991 through December 1992. Am J Obstet Gynecol. 1995; 173:1423–1431.19. Statistics Korea, Korean Statistical Information Service. Population dynamics (marriage and divorce) database. accessed on 6 April 2015. Available at http://www.kosis.kr/.20. Haddad GG, Green TP. Diagnostic approach to respiratory disease. In : Kliegman RM, Behrman RE, Jenson HB, Stanton BF, editors. Nelson textbook of pediatrics. 19th ed. Philadelphia, Pa: Saunders Elsevier;2011. p. 1421.21. Meadow W, Frain L, Ren Y, Lee G, Soneji S, Lantos J. Serial assessment of mortality in the neonatal intensive care unit by algorithm and intuition: certainty, uncertainty, and informed consent. Pediatrics. 2002; 109:878–886.22. Ondoa-Onama C, Tumwine JK. Immediate outcome of babies with low Apgar score in Mulago Hospital, Uganda. East Afr Med J. 2003; 80:22–29.23. Moster D, Lie RT, Irgens LM, Bjerkedal T, Markestad T. The association of Apgar score with subsequent death and cerebral palsy: a population-based study in term infants. J Pediatr. 2001; 138:798–803.24. Barber CA, Wyckoff MH. Use and efficacy of endotracheal versus intravenous epinephrine during neonatal cardiopulmonary resuscitation in the delivery room. Pediatrics. 2006; 118:1028–1034.25. Ziino AJ, Davies MW, Davis PG. Epinephrine for the resuscitation of apparently stillborn or extremely bradycardic newborn infants. Cochrane Database Syst Rev. 2003; CD003849.26. Luke B, Brown MB. The changing risk of infant mortality by gestation, plurality, and race: 1989-1991 versus 1999-2001. Pediatrics. 2006; 118:2488–2497.27. Norwitz ER, Edusa V, Park JS. Maternal physiology and complications of multiple pregnancy. Semin Perinatol. 2005; 29:338–348.28. Qiu X, Lee SK, Tan K, Piedboeuf B, Canning R. Canadian Neonatal Network. Comparison of singleton and multiple-birth outcomes of infants born at or before 32 weeks of gestation. Obstet Gynecol. 2008; 111:365–371.29. Nielsen HC, Harvey-Wilkes K, MacKinnon B, Hung S. Neonatal outcome of very premature infants from multiple and singleton gestations. Am J Obstet Gynecol. 1997; 177:653–659.30. Peacock JL, Lo JW, D'Costa W, Calvert S, Marlow N, Greenough A. Respiratory morbidity at follow-up of small-for-gestational-age infants born very prematurely. Pediatr Res. 2013; 73:457–463.31. Guellec I, Lapillonne A, Renolleau S, Charlaluk ML, Roze JC, Marret S, Vieux R, Monique K, Ancel PY. EPIPAGE Study Group. Neurologic outcomes at school age in very preterm infants born with severe or mild growth restriction. Pediatrics. 2011; 127:e883–e891.32. Khoury MJ, Marks JS, McCarthy BJ, Zaro SM. Factors affecting the sex differential in neonatal mortality: the role of respiratory distress syndrome. Am J Obstet Gynecol. 1985; 151:777–782.33. Lemons JA, Bauer CR, Oh W, Korones SB, Papile LA, Stoll BJ, Verter J, Temprosa M, Wright LL, Ehrenkranz RA, et al. Very low birth weight outcomes of the National Institute of Child health and human development neonatal research network, January 1995 through December 1996. NICHD Neonatal Research Network. Pediatrics. 2001; 107:E1.34. Cornette L. Fetal and neonatal inflammatory response and adverse outcome. Semin Fetal Neonatal Med. 2004; 9:459–470.35. Tanir HM, Sener T, Tekin N, Aksit A, Ardic N. Preterm premature rupture of membranes and neonatal outcome prior to 34 weeks of gestation. Int J Gynaecol Obstet. 2003; 82:167–172.36. Mercer BM, Miodovnik M, Thurnau GR, Goldenberg RL, Das AF, Ramsey RD, Rabello YA, Meis PJ, Moawad AH, Iams JD, et al. Antibiotic therapy for reduction of infant morbidity after preterm premature rupture of the membranes. A randomized controlled trial. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. JAMA. 1997; 278:989–995.37. Liggins GC, Howie RN. A controlled trial of antepartum glucocorticoid treatment for prevention of the respiratory distress syndrome in premature infants. Pediatrics. 1972; 50:515–525.38. Redman ME, Gonik B. Cesarean delivery rates at the threshold of viability. Am J Obstet Gynecol. 2002; 187:873–876.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Study of Prematurity and Low Birth Weight Infants
- Neonatal Research Network of Japan and Neonatal Database
- Rehospitalization of Low-birth-weight Infants Who Were Discharged from NICU
- Changes in Neonatal Epidemiology during the Last 3 Decades in Korea
- The risk factors and prognosis associated with neonatal pulmonary hemorrhage