Immune Netw.
2016 Aug;16(4):256-260. 10.4110/in.2016.16.4.256.
Stevens–Johnson Syndrome and Toxic Epidermal Necrolysis Associated with Acetaminophen Use during Viral Infections
- Affiliations
-
- 1Department of Allergy & Clinical Immunology, Ajou University School of Medicine, Suwon 16499, Korea. ye9007@ajou.ac.kr
- 2Ajou Regional Pharmacovigilance Center, Ajou University Hospital, Suwon 16499, Korea.
- KMID: 2349887
- DOI: http://doi.org/10.4110/in.2016.16.4.256
Abstract
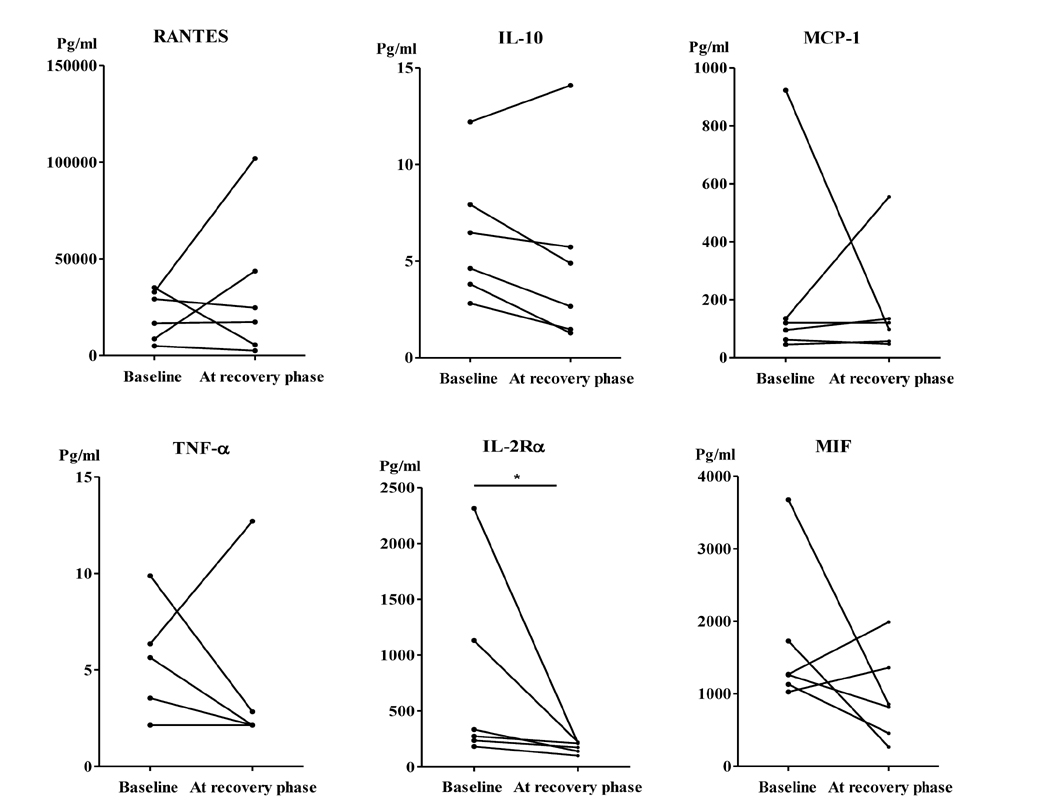
- An association between drug treatment for viral infections and severe cutaneous adverse reactions has been noted. We investigated six patients diagnosed with Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) after being prescribed acetaminophen for suspected viral illnesses. Multiplex analysis was performed to measure cytokine levels in sera before and after treatment. IL-2Rα levels significantly decreased during the convalescence phase. Although acetaminophen is relatively safe, the drug can trigger SJS/TEN in patients with suspected viral infections. T-cells and monocytes may be key components of the link between viral infection and acetaminophen-induced SJS/TEN.
MeSH Terms
Figure
Reference
-
1. Letko E, Papaliodis DN, Papaliodis GN, Daoud YJ, Ahmed AR, Foster CS. Stevens-Johnson syndrome and toxic epidermal necrolysis: a review of the literature. Ann Allergy Asthma Immunol. 2005; 94:419–436.
Article2. Pereira FA, Mudgil AV, Rosmarin DM. Toxic epidermal necrolysis. J Am Acad Dermatol. 2007; 56:181–200.
Article3. Torres MJ, Mayorga C, Blanca M. Nonimmediate allergic reactions induced by drugs: pathogenesis and diagnostic tests. J Investig Allergol Clin Immunol. 2009; 19:80–90.4. Tohyama M, Hashimoto K. Immunological mechanisms of epidermal damage in toxic epidermal necrolysis. Curr Opin Allergy Clin Immunol. 2012; 12:376–382.
Article5. Harr T, French LE. Toxic epidermal necrolysis and Stevens-Johnson syndrome. Orphanet J Rare Dis. 2010; 5:39.
Article6. Barron SJ, Del Vecchio MT, Aronoff SC. Intravenous immunoglobulin in the treatment of Stevens-Johnson syndrome and toxic epidermal necrolysis: a meta-analysis with meta-regression of observational studies. Int J Dermatol. 2015; 54:108–115.
Article7. Shiohara T, Kano Y. A complex interaction between drug allergy and viral infection. Clin Rev Allergy Immunol. 2007; 33:124–133.
Article8. Blazquez AB, Cuesta J, Mayorga C. Role of dendritic cells in drug allergy. Curr Opin Allergy Clin Immunol. 2011; 11:279–284.
Article9. Kim KJ, Lee DP, Suh HS, Lee MW, Choi JH, Moon KC, Koh JK. Toxic epidermal necrolysis: analysis of clinical course and SCORTEN-based comparison of mortality rate and treatment modalities in Korean patients. Acta Derm Venereol. 2005; 85:497–502.10. Mockenhaupt M. The current understanding of Stevens-Johnson syndrome and toxic epidermal necrolysis. Expert Rev Clin Immunol. 2011; 7:803–813.
Article11. Beldomenico PM, Telfer S, Gebert S, Lukomski L, Bennett M, Begon M. Poor condition and infection: a vicious circle in natural populations. Proc Biol Sci. 2008; 275:1753–1759.12. Segel GB, Halterman JS. Neutropenia in pediatric practice. Pediatr Rev. 2008; 29:12–23.
Article13. Sohn KH, Oh SY, Lim KW, Kim MY, Lee SY, Kang HR. Sorafenib induces delayed-onset cutaneous hypersensitivity: a case series. Allergy Asthma Immunol Res. 2015; 7:304–307.
Article14. Kim EJ, Lim H, Park SY, Kim S, Yoon SY, Bae YJ, Kwon HS, Cho YS, Moon HB, Kim TB. Rapid onset of Stevens-Johnson syndrome and toxic epidermal necrolysis after ingestion of acetaminophen. Asia Pac Allergy. 2014; 4:68–72.
Article15. Shimizu T. Role of macrophage migration inhibitory factor (MIF) in the skin. J Dermatol Sci. 2005; 37:65–73.
Article16. Alam R. Chemokines in allergic inflammation. J Allergy Clin Immunol. 1997; 99:273–277.17. Nomura YM, Lim H, Park SY, Kim S, Yoon SY, Bae YJ, Kwon HS, Cho YS, Moon HB, Kim TB. Evaluation of serum cytokine levels in toxic epidermal necrolysis and Stevens-Johnson syndrome compared with other delayed-type adverse drug reactions. J Dermatol. 2011; 38:1076–1079.
Article18. Yawalkar NM, Shrikhande M, Hari Y, Nievergelt H, Braathen LR, Pichler WJ. Evidence for a role for IL-5 and eotaxin in activating and recruiting eosinophils in drug-induced cutaneous eruptions. J Allergy Clin Immunol. 2000; 106:1171–1176.
Article19. Halevy S, Livni E. The role of macrophage migration inhibition factor in toxic epidermal necrolysis. Int J Dermatol. 1997; 36:776–778.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- T Cell Mediated Drug Hypersensitivity: Stevens Johnson Syndrome and Toxic Epidermal Necrolysis
- A Case of Toxic Epidermal Necrolysis
- Rapid onset of Stevens-Johnson syndrome and toxic epidermal necrolysis after ingestion of acetaminophen
- A comparative clinical study of toxic epidermal necrolysis and Stevens-Johnson syndrome
- Two Cases of HLA-B59(+) Stevens-Johnson Syndrome (SJS)-Toxic Epidermal Necrolysis (TEN) Associated with Methazolamide Treatment