J Korean Orthop Assoc.
2016 Aug;51(4):294-300. 10.4055/jkoa.2016.51.4.294.
Surgical and Oncological Outcome of Pelvis Bone Tumor Patients with Type III Internal Hemipelvectomy
- Affiliations
-
- 1Department of Orthopedic Surgery, Korea Cancer Center Hospital, Seoul, Korea. dgjeon@kirams.re.kr
- KMID: 2348635
- DOI: http://doi.org/10.4055/jkoa.2016.51.4.294
Abstract
- PURPOSE
It is generally accepted that bony reconstruction after type III (pubic) internal pelvectomy is not necessary. However, technical problems in type III resection, functional outcome according to the extent of resection, and the usefulness of synthetic material to decrease the risk of hernia has not been well addressed.
MATERIALS AND METHODS
Fifteen patients who underwent type III internal pelvectomy were extracted and the pathologic diagnosis, Enneking's stage, location of tumor and size, operation time, amount of transfusion, surgical margin, local recurrence, distant metastasis, and functional outcomes were analyzed according to the extent of resection.
RESULTS
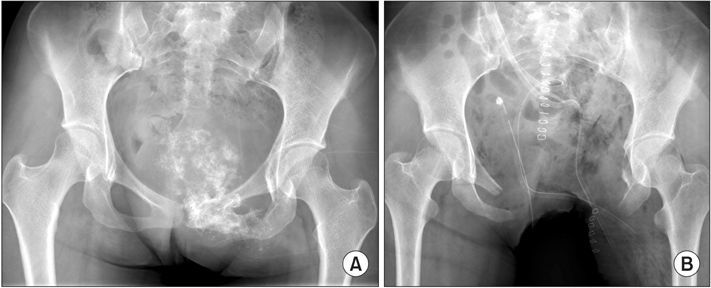
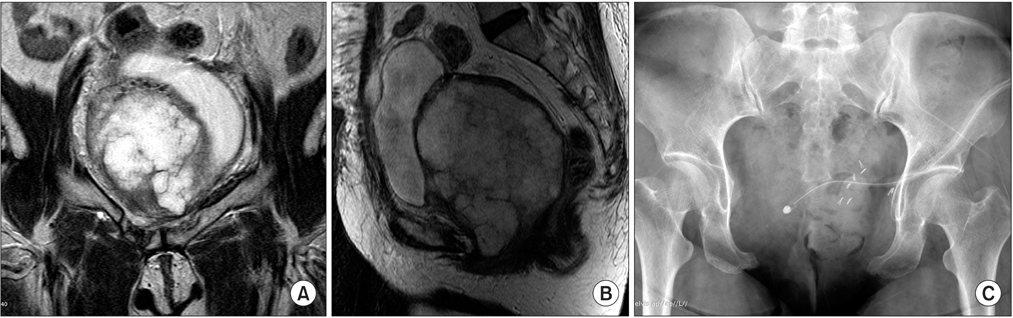
Pathologic diagnosis was chondrosarcoma in 9, Ewing's sarcoma in 3, metastatic carcinoma in 2, and osteosarcoma in 1 patient. There were 4 patients with local recurrence and one with concomitant lung metastasis. Average Musculoskeletal Tumor Society functional score was 26.7. According to the extent of resection, functional score of 7 cases with unilateral both rami (6) or ischium (1) resection was 26, 4 cases with unilateral both rami and partial contralateral pubic ramus resection was 25, and 4 cases with unilateral both rami including ischium was 24. Two patients had tumor related complication. One patient with a huge intrapelvic tumor aroused at the symphysis pubis showed urethral invasion at presentation, therefore, urethral resection and permanent suprapubic cystostomy was inevitable. The other patient with bilateral pubic ramus involvement by tumor showed caudal displacement of the uterus after pregnancy (4 years after primary resection). She underwent Caesearian section for delivery.
CONCLUSION
Regardless of the extent of pubic bone resection, functional outcome was similar. The risk of abdominal or pelvic organ hernia was minimal even without the use of artificial material for soft tissue reconstruction; however, when the extent of resection crosses the symphysis pubis, selective application of an additional procedure to reinforce the pelvic floor may be considered.
Keyword
MeSH Terms
Figure
Reference
-
1. Enneking WF, Dunham WK. Resection and reconstruction for primary neoplasms involving the innominate bone. J Bone Joint Surg Am. 1978; 60:731–746.
Article2. Wirbel RJ, Schulte M, Maier B, Koschnik M, Mutschler WE. Chondrosarcoma of the pelvis: oncologic and functional outcome. Sarcoma. 2000; 4:161–168.
Article3. Delloye C, Banse X, Brichard B, Docquier PL, Cornu O. Pelvic reconstruction with a structural pelvic allograft after resection of a malignant bone tumor. J Bone Joint Surg Am. 2007; 89:579–587.
Article4. Hillmann A, Hoffmann C, Gosheger G, Rödl R, Winkelmann W, Ozaki T. Tumors of the pelvis: complications after reconstruction. Arch Orthop Trauma Surg. 2003; 123:340–344.
Article5. O'Connor MI, Sim FH. Salvage of the limb in the treatment of malignant pelvic tumors. J Bone Joint Surg Am. 1989; 71:481–494.6. Johnson JT. Reconstruction of the pelvic ring following tumor resection. J Bone Joint Surg Am. 1978; 60:747–751.
Article7. Gradinger R, Rechl H, Hipp E. Pelvic osteosarcoma. Resection, reconstruction, local control, and survival statistics. Clin Orthop Relat Res. 1991; 270:149–158.8. Abudu A, Grimer RJ, Cannon SR, Carter SR, Sneath RS. Reconstruction of the hemipelvis after the excision of malignant tumours. Complications and functional outcome of prostheses. J Bone Joint Surg Br. 1997; 79:773–779.9. Reddy SS, Bloom ND. En bloc resection of extra-peritoneal soft tissue neoplasms incorporating a type III internal hemipelvectomy: a novel approach. World J Surg Oncol. 2012; 10:222.
Article10. Kawai A, Healey JH, Boland PJ, Lin PP, Huvos AG, Meyers PA. Prognostic factors for patients with sarcomas of the pelvic bones. Cancer. 1998; 82:851–859.
Article11. Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993; 286:241–246.
Article12. Coleman RE. Metastatic bone disease: clinical features, pathophysiology and treatment strategies. Cancer Treat Rev. 2001; 27:165–176.
Article13. Hugate R Jr, Sim FH. Pelvic reconstruction techniques. Orthop Clin North Am. 2006; 37:85–97.
Article14. Han IK, Lee YM, Cho HS, Oh JH, Lee SH, Kim HS. Outcome after surgical treatment of pelvic sarcomas. Clin Orthop Surg. 2010; 2:160–166.
Article15. Fuchs B, Hoekzema N, Larson DR, Inwards CY, Sim FH. Osteosarcoma of the pelvis: outcome analysis of surgical treatment. Clin Orthop Relat Res. 2009; 467:510–518.
Article16. Capanna R, Campanacci DA. The treatment of metastases in the appendicular skeleton. J Bone Joint Surg Br. 2001; 83:471–481.
Article17. Amid PK. Classification of biomaterials and their related complications in abdominal wall hernia surgery. Hernia. 1997; 1:15–21.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recent Advances in Malignant Bone Tumor Treatment
- Traumatic hemipelvectomy before body image has developed
- Outcome after Surgical Treatment of Pelvic Sarcomas
- Using Denosumab as a Nonsurgical Management of Aneurysmal Bone Cysts in the Pelvis
- Long-term Outcome of Chondrosarcoma: A Single Institutional Experience