J Gynecol Oncol.
2015 Oct;26(4):320-326. 10.3802/jgo.2015.26.4.320.
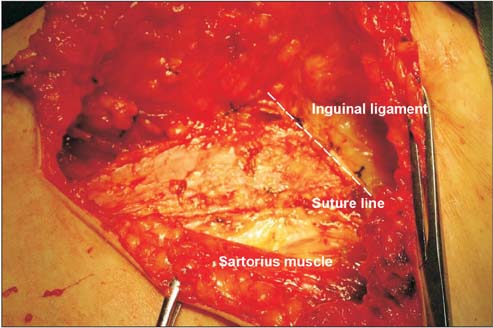
Clinical application of sartorius tendon transposition during radical vulvectomy: a case control study of 58 cases at a single institution
- Affiliations
-
- 1Department of Gynecologic Oncology, Affiliated Tumor Hospital of Zhengzhou University, Zhengzhou, China. lilei04301596@163.com
- KMID: 2345923
- DOI: http://doi.org/10.3802/jgo.2015.26.4.320
Abstract
OBJECTIVE
The aim of this study was to investigate the clinical effects of sartorius tendon transposition versus sartorius transposition during bilateral inguinal lymphadenectomy of radical vulvectomy.
METHODS
A total of 58 vulvar cancer patients who had surgery from May 2007 to October 2013, in which 30 patients received sartorius transposition and 28 patients received sartorius tendon transposition. All patients were matched by age, body mass index, stage, histology, and grade. Intraoperative variables and postoperative complications, recurrence, progression-free survival (PFS), and overall survival (OS) and postoperative life quality were compared and analyzed.
RESULTS
No significant differences were found at median surgical times and amounts of bleeding (p=0.316 and p=0.249, respectively), neither at the incidences of groin cellulitis and lymphocele (p=0.673 and p=0.473, respectively), but the recovery times of the inguinal wounds were shorter (p=0.026) and the incidences of wound break and chronic lymphedema were significantly decreased in the tendon transposition group (p=0.012 and p=0.022, respectively). Postoperative quality of life in tendon transposition group was significantly improved as indicated by the EORTC QLQ-C30 questionnaire. Recurrences were similar (p=0.346) and no significant differences were found at PFS and OS (p=0.990 and p=0.683, respectively).
CONCLUSION
Compared to sartorius transposition, sartorius tendon transposition during inguinal lymphadenectomy led to improved patient recovery, reduced postoperative complications, and improved life quality without compromising the outcomes.
Keyword
MeSH Terms
Figure
Reference
-
1. Woelber L, Kock L, Gieseking F, Petersen C, Trillsch F, Choschzick M, et al. Clinical management of primary vulvar cancer. Eur J Cancer. 2011; 47:2315–2321.2. van der Steen S, de Nieuwenhof HP, Massuger L, Bulten J, de Hullu JA. New FIGO staging system of vulvar cancer indeed provides a better reflection of prognosis. Gynecol Oncol. 2010; 119:520–525.3. Soliman AA, Heubner M, Kimmig R, Wimberger P. Morbidity of inguinofemoral lymphadenectomy in vulval cancer. ScientificWorldJournal. 2012; 2012:341253.4. Way S. Carcinoma of the vulva. Am J Obstet Gynecol. 1960; 79:692–697.5. Judson PL, Jonson AL, Paley PJ, Bliss RL, Murray KP, Downs LS Jr, et al. A prospective, randomized study analyzing sartorius transposition following inguinal-femoral lymphadenectomy. Gynecol Oncol. 2004; 95:226–230.6. Miller AJ, Bruna J, Beninson J. A universally applicable clinical classification of lymphedema. Angiology. 1999; 50:189–192.7. Taussig FJ. Cancer of the vulva: an analysis of 155 cases (1911-1940). Am J Obstet Gynecol. 1940; 40:764–779.8. Wills A, Obermair A. A review of complications associated with the surgical treatment of vulvar cancer. Gynecol Oncol. 2013; 131:467–479.9. Gaarenstroom KN, Kenter GG, Trimbos JB, Agous I, Amant F, Peters AA, et al. Postoperative complications after vulvectomy and inguinofemoral lymphadenectomy using separate groin incisions. Int J Gynecol Cancer. 2003; 13:522–527.10. Li J, Zhou H, Wang LJ, Lu XM, Rao QX, Lu HW, et al. A modified triple incision technique for women with locally advanced vulvar cancer: a description of the technique and outcomes. Eur J Obstet Gynecol Reprod Biol. 2012; 164:185–190.11. DiSaia PJ, Creasman WT, Rich WM. An alternate approach to early cancer of the vulva. Am J Obstet Gynecol. 1979; 133:825–832.12. Bell JG, Lea JS, Reid GC. Complete groin lymphadenectomy with preservation of the fascia lata in the treatment of vulvar carcinoma. Gynecol Oncol. 2000; 77:314–318.13. Zhang X, Sheng X, Niu J, Li H, Li D, Tang L, et al. Sparing of saphenous vein during inguinal lymphadenectomy for vulval malignancies. Gynecol Oncol. 2007; 105:722–726.14. Manci N, Marchetti C, Esposito F, De Falco C, Bellati F, Giorgini M, et al. Inguinofemoral lymphadenectomy: randomized trial comparing inguinal skin access above or below the inguinal ligament. Ann Surg Oncol. 2009; 16:721–728.15. Paley PJ, Johnson PR, Adcock LL, Cosin JA, Chen MD, Fowler JM, et al. The effect of sartorius transposition on wound morbidity following inguinal-femoral lymphadenectomy. Gynecol Oncol. 1997; 64:237–241.16. Walker KF, Day H, Abu J, Nunns D, Williamson K, Duncan T. Do surgical techniques used in groin lymphadenectomy for vulval cancer affect morbidity rates? Int J Gynecol Cancer. 2011; 21:1495–1499.17. Senn B, Mueller MD, Cignacco EL, Eicher M. Period prevalence and risk factors for postoperative short-term wound complications in vulvar cancer: a cross-sectional study. Int J Gynecol Cancer. 2010; 20:646–654.18. Baiocchi G, Rocha RM. Vulvar cancer surgery. Curr Opin Obstet Gynecol. 2014; 26:9–17.19. Rouzier R, Haddad B, Dubernard G, Dubois P, Paniel BJ. Inguinofemoral dissection for carcinoma of the vulva: effect of modifications of extent and technique on morbidity and survival. J Am Coll Surg. 2003; 196:442–450.20. Senn B, Eicher M, Mueller MD, Hornung R, Fink D, Baessler K, et al. A patient-reported outcome measure to identify occurrence and distress of post-surgery symptoms of WOMen with vulvAr Neoplasia (WOMAN-PRO): a cross sectional study. Gynecol Oncol. 2013; 129:234–240.21. Gunther V, Malchow B, Schubert M, Andresen L, Jochens A, Jonat W, et al. Impact of radical operative treatment on the quality of life in women with vulvar cancer: a retrospective study. Eur J Surg Oncol. 2014; 40:875–882.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Vulvar reconstruction with Gluteal Fasciocutaneous Island Sensory Flap after Radical Vulvectomy in the Patient with Vulvar Cancer
- The Result of Full Tendon Transposition in Paralyzed Strabismus
- Microneurovascular Free Muscle Transplantations in Dogs
- The Effect of V-Y Advancement Flap after Vulvectomy in Patients with Vulvar Cancer
- Effect of Vertical Displacement of Bilateral Horizontal Muscles in AV Syndrome