J Korean Soc Radiol.
2016 Aug;75(2):92-103. 10.3348/jksr.2016.75.2.92.
Vascular Plug-Assisted Retrograde Transvenous Obliteration for the Management of Gastric Varices: Comparative Effectiveness between Gelatin Sponge Embolization and Permanent Sclerosant
- Affiliations
-
- 1Department of Radiology, Dong-A University Hospital, Dong-A University College of Medicine, Busan, Korea. bhpark@dau.ac.kr
- 2Department of Radiology, Gospel Hospital, Kosin University College of Medicine, Busan, Korea.
- KMID: 2344798
- DOI: http://doi.org/10.3348/jksr.2016.75.2.92
Abstract
- PURPOSE
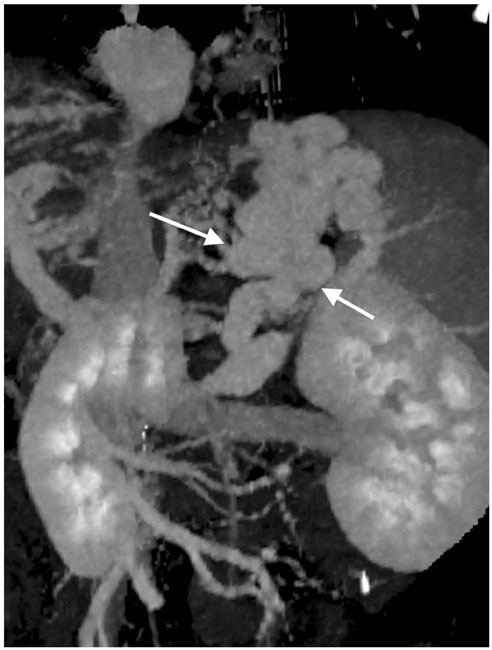
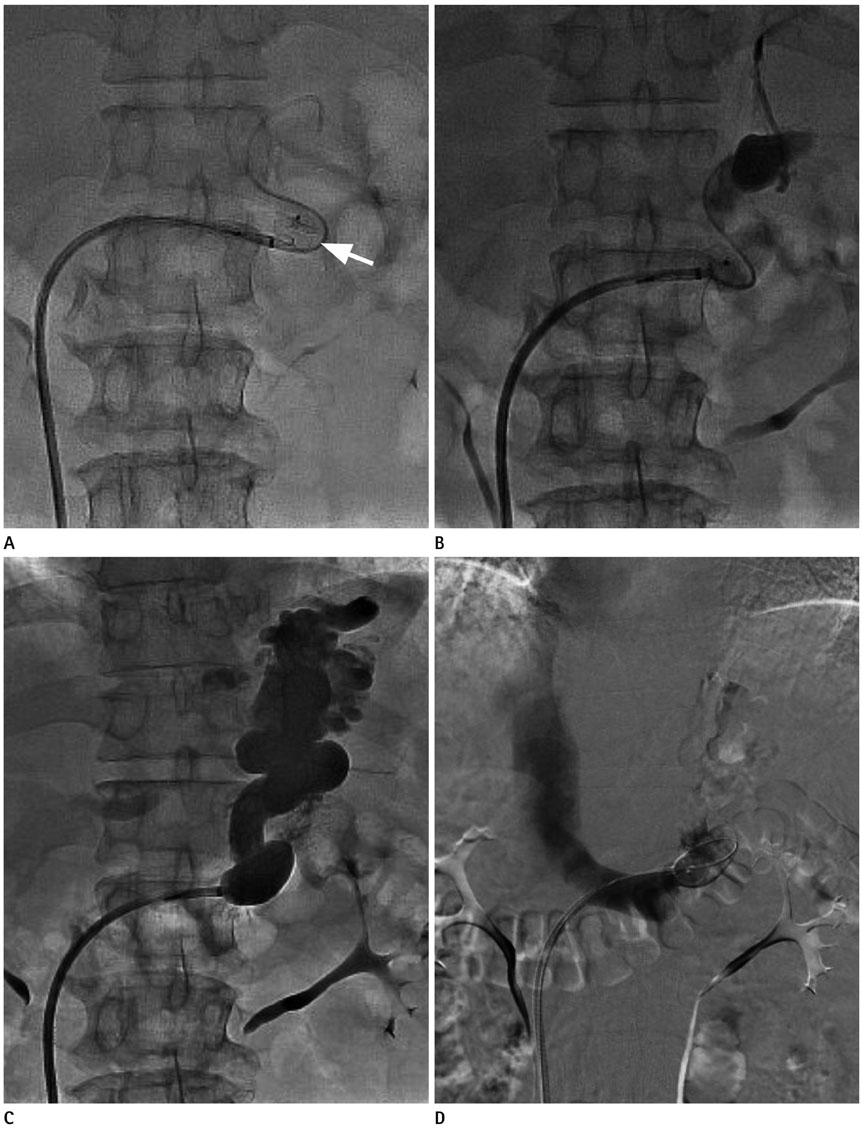
To evaluate the short-term outcome of plug-assisted retrograde transvenous obliteration (PARTO) using vascular plugs and gelatin sponges in comparison with balloon-occluded retrograde transvenous obliteration (BRTO) for the management of gastric varices.
MATERIALS AND METHODS
From January 2005 to October 2014, 171 patients were referred for management of gastric varices, of which, 52 patients with hemodynamically stable gastric varices (48 recent bleeding; 4 primary prophylaxes) were evaluated. Of these, 38 received BRTO (men/women 23/15; mean age 61.3; Child-Pugh classes A/B/C = 11/25/2) and 14 underwent PARTO (men/women 11/3; mean age 63.4; Child-Pugh classes A/B/C = 9/4/1). The technical success rate, complications, variceal changes, liver function, and exacerbation of ascites/pleural effusion were compared between the 2 groups within 3 months after the procedure.
RESULTS
The technical success rates were 92.1% in the BRTO and 100% in the PARTO group. Procedure-related early complications occurred in the BRTO group alone (8%, n = 3). Among patients with technical success, follow-up CT at 1 month was available for 98% (n = 48/49). Complete thrombosis of gastric varices was achieved in 97.1% in the BRTO and 100% in the PARTO group. Worsening of esophageal varices was observed in 24% of the BRTO group alone (n = 8). The albumin level increased significantly in both groups and aspartate aminotransferase/alanine aminotransferase level improved significantly in the PARTO group (p < 0.05). Exacerbation of ascites/pleural effusion was observed in both groups (35.2% vs. 21.4%, both p > 0.05).
CONCLUSION
PARTO appears to be equivalent to BRTO for short-term management of gastric varices.
MeSH Terms
Figure
Reference
-
1. Al-Osaimi AM, Caldwell SH. Medical and endoscopic management of gastric varices. Semin Intervent Radiol. 2011; 28:273–282.2. Saad WE, Darcy MD. Transjugular intrahepatic portosystemic shunt (TIPS) versus balloon-occluded retrograde transvenous obliteration (BRTO) for the management of gastric varices. Semin Intervent Radiol. 2011; 28:339–349.3. Ripamonti R, Ferral H, Alonzo M, Patel NH. Transjugular intrahepatic portosystemic shunt-related complications and practical solutions. Semin Intervent Radiol. 2006; 23:165–176.4. Kanagawa H, Mima S, Kouyama H, Gotoh K, Uchida T, Okuda K. Treatment of gastric fundal varices by balloon-occluded retrograde transvenous obliteration. J Gastroenterol Hepatol. 1996; 11:51–58.5. Fukuda T, Hirota S, Sugimura K. Long-term results of balloon-occluded retrograde transvenous obliteration for the treatment of gastric varices and hepatic encephalopathy. J Vasc Interv Radiol. 2001; 12:327–336.6. Hirota S, Matsumoto S, Tomita M, Sako M, Kono M. Retrograde transvenous obliteration of gastric varices. Radiology. 1999; 211:349–356.7. Saad WE. Balloon-occluded retrograde transvenous obliteration of gastric varices: concept, basic techniques, and outcomes. Semin Intervent Radiol. 2012; 29:118–128.8. Fukuda T, Hirota S, Matsumoto S, Sugimoto K, Fujii M, Tsurusaki M, et al. Application of balloon-occluded retrograde transvenous obliteration to gastric varices complicating refractory ascites. Cardiovasc Intervent Radiol. 2004; 27:64–67.9. An EJ, Kim YH, Kim SH. Comparison of coil embolization and sclerotherapy of collateral veins during balloon occluded retrograde transvenous obliteration: its long term effect for gastric varix treatment. J Korean Soc Radiol. 2011; 65:357–363.10. Kim JH, Kim YH, An EJ, Kim SH, Choi JS. CT findings after BRTO in patients with gastric varix bleeding: can we predict varix recurrence. J Korean Soc Radiol. 2011; 64:131–137.11. Park SJ, Chung JW, Kim HC, Jae HJ, Park JH. The prevalence, risk factors, and clinical outcome of balloon rupture in balloon-occluded retrograde transvenous obliteration of gastric varices. J Vasc Interv Radiol. 2010; 21:503–507.12. Hiraga N, Aikata H, Takaki S, Kodama H, Shirakawa H, Imamura M, et al. The long-term outcome of patients with bleeding gastric varices after balloon-occluded retrograde transvenous obliteration. J Gastroenterol. 2007; 42:663–672.13. Chikamori F, Kuniyoshi N, Shibuya S, Takase Y. Eight years of experience with transjugular retrograde obliteration for gastric varices with gastrorenal shunts. Surgery. 2001; 129:414–420.14. Sabri SS, Swee W, Turba UC, Saad WE, Park AW, Al-Osaimi AM, et al. Bleeding gastric varices obliteration with balloonoccluded retrograde transvenous obliteration using sodium tetradecyl sulfate foam. J Vasc Interv Radiol. 2011; 22:309–316. quiz 316.15. Gwon DI, Ko GY, Yoon HK, Sung KB, Kim JH, Shin JH, et al. Gastric varices and hepatic encephalopathy: treatment with vascular plug and gelatin sponge-assisted retrograde transvenous obliteration--a primary report. Radiology. 2013; 268:281–287.16. Sabri SS, Saad WE. Balloon-occluded retrograde transvenous obliteration (BRTO): technique and intraprocedural imaging. Semin Intervent Radiol. 2011; 28:303–313.17. Hashizume M, Kitano S, Yamaga H, Koyanagi N, Sugimachi K. Endoscopic classification of gastric varices. Gastrointest Endosc. 1990; 36:276–280.18. Tajiri T, Yoshida H, Obara K, Onji M, Kage M, Kitano S, et al. General rules for recording endoscopic findings of esophagogastric varices (2nd edition). Dig Endosc. 2010; 22:1–9.19. Yu NC, Margolis D, Hsu M, Raman SS, Lu DS. Detection and grading of esophageal varices on liver CT: comparison of standard and thin-section multiplanar reconstructions in diagnostic accuracy. AJR Am J Roentgenol. 2011; 197:643–649.20. Lubarsky M, Ray CE, Funaki B. Embolization agents-which one should be used when? Part 1: large-vessel embolization. Semin Intervent Radiol. 2009; 26:352–357.21. Choi SY, Won JY, Kim KA, Lee do Y, Lee KH. Foam sclerotherapy using polidocanol for balloon-occluded retrograde transvenous obliteration (BRTO). Eur Radiol. 2011; 21:122–129.22. Miura H, Yamagami T, Tanaka O, Yoshimatsu R. Portopulmonary venous anastomosis detected at balloon-occluded retrograde transvenous obliteration for gastric varices. J Vasc Interv Radiol. 2013; 24:131–134.23. Koito K, Namieno T, Nagakawa T, Morita K. Balloon-occluded retrograde transvenous obliteration for gastric varices with gastrorenal or gastrocaval collaterals. AJR Am J Roentgenol. 1996; 167:1317–1320.24. Gwon DI, Kim YH, Ko GY, Kim JW, Ko HK, Kim JH, et al. Vascular plug-assisted retrograde transvenous obliteration for the treatment of gastric varices and hepatic encephalopathy: a prospective multicenter study. J Vasc Interv Radiol. 2015; 26:1589–1595.25. Chikamori F, Kuniyoshi N, Shibuya S, Takase Y. Short-term hemodynamic effects of transjugular retrograde obliteration of gastric varices with gastrorenal shunt. Dig Surg. 2000; 17:332–336.26. Watanabe M, Shiozawa K, Ikehara T, Nakano S, Kougame M, Otsuka T, et al. Short-term effects and early complications of balloon-occluded retrograde transvenous obliteration for gastric varices. ISRN Gastroenterol. 2012; 2012:919371.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Plug-Assisted Retrograde Transvenous Obliteration for the Treatment of Gastric Varices: The Role of Intra-Procedural Cone-Beam Computed Tomography
- Plug-Assisted Retrograde Transvenous Obliteration for the Treatment of Gastric Varix with Both Gastrorenal and Gastrocaval Shunts: A Case Report
- Successful Treatment of Duodenal Variceal Bleeding with Coil-Assisted Retrograde Transvenous Obliteration: A Case Report
- Vascular Plug Assisted Retrograde Transvenous Obliteration (PARTO) for Gastric Varix Bleeding Patients in the Emergent Clinical Setting
- Off-label plug-assisted retrograde transvenous obliteration of a giant gastrorenal shunt: A report of two cases