Korean Circ J.
2016 Mar;46(2):239-245. 10.4070/kcj.2016.46.2.239.
Assessment of Aortic Elasticity in Patients with Celiac Disease
- Affiliations
-
- 1Cardiology Department, Antalya Education and Research Hospital, Antalya, Turkey. dr.nermin@mynet.com
- 2Gastroenterology Department, Antalya Education and Research Hospital, Antalya, Turkey.
- 3Cardiology Department, Yüksek İhtisas Education and Research Hospital, Ankara, Turkey.
- 4Internal Medicine Department, Antalya Education and Research Hospital, Antalya, Turkey.
- KMID: 2344476
- DOI: http://doi.org/10.4070/kcj.2016.46.2.239
Abstract
- BACKGROUND AND OBJECTIVES
Celiac disease (CD) is a chronic autoimmune disorder induced by dietary gluten intake by individuals who are genetically sensitive. Many studies report an increased risk of cardiovascular diseases in such patients. The aim of this study is to assess aortic elasticity properties in patients with CD that may be associated with an increased risk of cardiovascular disease.
SUBJECTS AND METHODS
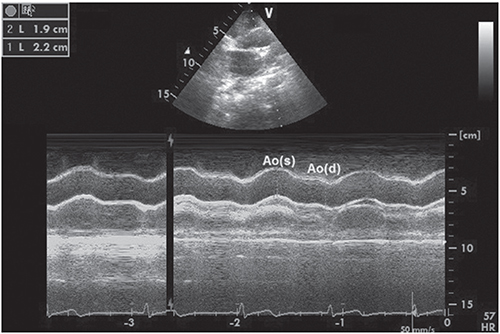
Eighty-one patients diagnosed with CD by antibody test and biopsy and 63 healthy volunteers were included in this prospective study. Electrocardiographic and echocardiographic examinations were performed.
RESULTS
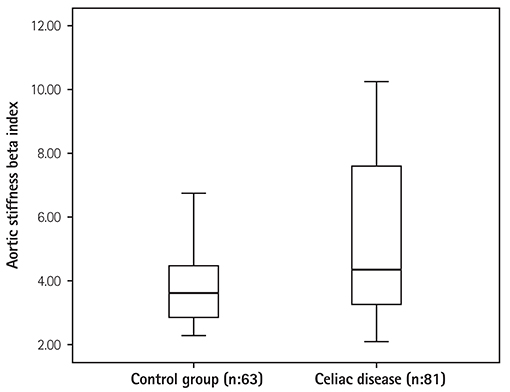
The CD group did not have any differences in the conventional echocardiographic parameters compared to the healthy individuals. However, patients in the CD group had an increased aortic stiffness beta index (4.3±2.3 vs. 3.6±1.6, p=0.010), increased pressure strain elastic modulus (33.6±17.0 kPa vs. 28.5±16.7 kPa, p=0.037), decreased aortic distensibility (7.0±3.0×10(-6) cm2/dyn vs. 8.2±3.6×10(-6) cm2/dyn, p=0.037), and similar aortic strain (17.9±7.7 vs. 16.0±5.5, p=0.070) compared to the control group. Patients with CD were found to have an elevated neutrophil/lymphocyte ratio compared to the control group (2.54±0.63 vs. 2.24±0.63, p=0.012). However, gluten-free diet and neutrophil/lymphocyte ratio were not found to be associated with aortic elasticity.
CONCLUSION
Patients with CD had increased aortic stiffness and decreased aortic distensibility. Gluten-free diet enabled the patients with CD to have a reduction in the inflammatory parameters whereas the absence of a significant difference in the elastic properties of the aorta may suggest that the risk of cardiovascular disease persists in this patient group despite a gluten-free diet.
MeSH Terms
Figure
Reference
-
1. Green PH, Cellier C. Celiac disesase. N Engl J Med. 2007; 357:1731–1743.2. Hallert C, Grant C, Grehn S, et al. Evidence of poor vitamin status in coeliac patients on a gluten-free diet for 10 years. Aliment Pharmacol Ther. 2002; 16:1333–1339.3. Cekin AH, Cekin Y, Sezer C. Celiac disease prevalence in patients with iron deficiency anemia. Turk J Gastroenterol. 2012; 23:490–495.4. Ludvigsson JF, de Faire U, Ekbom A, Montgomery SM. Vascular diasease in a population-based cohort of individuals hospitalised with coeliac disease. Heart. 2007; 93:1111–1115.5. Wei L, Spiers E, Reynolds N, Walsh S, Fahey T, MacDonald TM. The association between coeliac disease and cardiovascular disease. Aliment Pharmacol Ther. 2008; 27:514–519.6. Peters U, Askling J, Gridley G, Ekbom A, Linet M. Causes of death in patients with celiac disease in a population-based Swedish cohort. Arch Intern Med. 2003; 163:1566–1572.7. Emilsson L, Smith JG, West J, Melander O, Ludvigsson JF. Increased risk of atrial fibrillation in patients with coeliac disease: a nationwide cohort study. Eur Heart J. 2011; 32:2430–2437.8. De Marchi S, Chiarioni G, Prior M, Arosio E. Young adults with coeliac disease may be at increased risk of early atherosclerosis. Aliment Pharmacol Ther. 2013; 38:162–169.9. Ludvigsson JF, James S, Askling J, Stenestrand U, Ingelsson E. Nationwide cohort study of risk of ischemic heart disease in patients with celiac disease. Circulation. 2011; 123:483–490.10. Emilsson L, Carlsson R, Holmqvist M, James S, Ludvigsson JF. The characterisation and risk factors of ischaemic heart disease in patients with coeliac disease. Aliment Pharmacol Ther. 2013; 37:905–914.11. Lang RM, Bierig M, Devereux RB, et al. Chamber Quantification Writing Group. American Society of Echocardiography's Guidelines and Standards Committee. European Association of Echocardiography. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005; 18:1440–1463.12. Sahn DJ, DeMaria A, Kisslo J, Weyman A. Recommendations regarding quantification in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation. 1978; 58:1072–1083.13. Lacombe F, Dart A, Dewar E, Jennings G, Cameron J, Laufer E. Arterial elastic properties in man: a comparison of echo-Doppler indices of aortic stiffness. Eur Heart J. 1992; 13:1040–1045.14. Ludvigsson JF, Lefner DA, Bai JC, et al. The Oslo definitions for celiac disease and related terms. Gut. 2013; 62:43–52.15. Green PH, Celliere C. Celiac disease. N Engl J Med. 2007; 357:1731–1743.16. Green PH, Jabri B. Coeliac disease. Lancet. 2003; 362:383–391.17. Norsa L, Shamir R, Zevit N. Gluten-free diet in celiac disease: protective or providing additive risk factors fort he development of cardiovascular disease? Nutr Ther Metab. 2012; 30:1–9.18. Ehsani-Ardakani MJ, Rostami Nejad M, Villanacci V, et al. Gastrointestinal and non-gastrointestinal presentation in patients with celiac disease. Arch Iran Med. 2013; 16:78–82.19. Park SW, Park SJ, Shin JI. Another possible underlying mechanism for the positive association between celiac disease and systemic lupus erythematosus: the role of interleukin 21. J Rheumatol. 2013; 40:1619.20. van den Driessche A, Eenkhoorn V, Van Gaal L, De Block C. Type I diabetes and autoimmune polyglandular syndrome: a clinical review. Neth J Med. 2009; 67:376–387.21. Fasano A. Systemic autoimmune disorders in celiac disease. Curr Opin Gastroenterol. 2006; 22:674–679.22. Yingchoncharoen T, Limpijankit T, Jongjirasiri S, Laothamatas J, Yamwong S, Sritara P. Arterial stiffness contributes to coronary artery disease risk prediction beyond the traditional risk score (RAMA-EGAT score). Heart Asia. 2012; 4:77–82.23. Tsuchikura S, Shoji T, Kimoto E, et al. Central versus peripheral arterial stiffness in association with coronary, cerebral and peripheral arterial disease. Atherosclerosis. 2010; 211:480–485.24. El Gamal YM, Elmasry OA, El Hadidi IS, Soliman OK. Proximal aortic stiffness is increased in systemic lupus erythematosus activity in children and adolescents. ISRN Pediatr. 2013; 765253.25. Barbulescu AL, Vreju F, Cojocaru-Gofita IR, Musetescu AE, Ciurea PL. Impaired arterial stiffness in systemic lupus ertythematosus-correlations with inflammation markers. Curr Health Sci J. 2012; 38:61–65.26. Gefel D, Doncheva M, Ben-Valid E, el Wahab-Daraushe A, Lugassy G, Sela BA. Recurrent stroke in a young patient with celiac disease and hyperhomocysteinemia. Isr Med Assoc J. 2002; 4:222–223.27. Wang X, Cui L, Joseph J, et al. Homocysteine induces cardiomyocyte dysfunction and apoptosis through p38MAPK-mediated increase in oxidant stress. J Mol Cell Cardiol. 2012; 52:753–760.28. Liao P, Wang SQ, Wang S, et al. p38 Mitogen-activated protein kinase mediated a negative inotropic effect in cardiac myocytes. Circ Res. 2002; 90:190–196.29. Nestel PJ, Chronopoulos A, Cehun M. Arterial stiffness is rapidly induces by raising the plasma homocysteine concentration with methionine. Atherosclerosis. 2003; 171:83–86.30. Lim PO, Tzemos N, Farquharson CA, et al. Reversible hypertension following coeliac disease treatment: the role moderate hyperhomocysteinaemia and vascular endothelial dysfunction. J Hum Hypertens. 2002; 16:411–415.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Aortic Elasticity was not Related with Duration, Bath Ankylosing Spondylitis Disease Activity Index
- Merits of and Technical Tips for Supra-Mesenteric Aortic Cross Clamping
- Aortopathy in Congenital Heart Disease in Adults: Aortic Dilatation with Decreased Aortic Elasticity that Impacts Negatively on Left Ventricular Function
- Biaxial Strain Analysis of Various Fixation Models in Porcine Aortic and Pulmonary Valves
- Association between Celiac Disease and Intussusceptions in Children: Two Case Reports and Literature Review