Korean Circ J.
2016 Jul;46(4):499-506. 10.4070/kcj.2016.46.4.499.
Multimodality Intravascular Imaging Assessment of Plaque Erosion versus Plaque Rupture in Patients with Acute Coronary Syndrome
- Affiliations
-
- 1Heart Research Institute, Cardiovascular-Arrhythmia Center, College of Medicine, Chung-Ang University Hospital, Seoul, Korea. wslee1227@cau.ac.kr
- 2Cardiovascular Research Foundation, New York, USA.
- 3Chonnam National University Hospital, Gwangju, Korea.
- 4Inje University Ilsan Paik Hospital, Koyang, Korea.
- 5Jeju National University Hospital, Jeju, Korea.
- 6Samsung Medical Center, Seoul, Korea.
- KMID: 2344424
- DOI: http://doi.org/10.4070/kcj.2016.46.4.499
Abstract
- BACKGROUND AND OBJECTIVES
We assessed plaque erosion of culprit lesions in patients with acute coronary syndrome in real world practice.
SUBJECTS AND METHODS
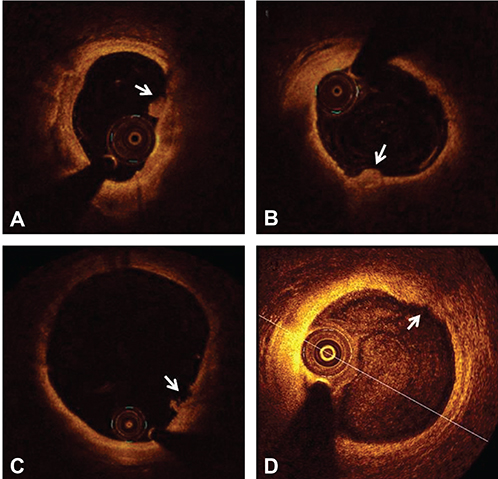
Culprit lesion plaque rupture or plaque erosion was diagnosed with optical coherence tomography (OCT). Intravascular ultrasound (IVUS) was used to determine arterial remodeling. Positive remodeling was defined as a remodeling index (lesion/reference EEM [external elastic membrane area) >1.05.
RESULTS
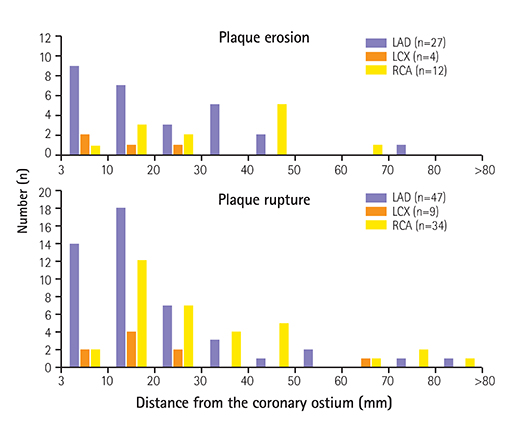
A total of 90 patients who had plaque rupture showing fibrous-cap discontinuity and ruptured cavity were enrolled. 36 patients showed definite OCT-plaque erosion, while 7 patients had probable OCT-plaque erosion. Overall, 26% (11/43) of definite/probable plaque erosion had non-ST elevation myocardial infarction (NSTEMI) while 35% (15/43) had ST elevation myocardial infarction (STEMI). Conversely, 14.5% (13/90) of plaque rupture had NSTEMI while 71% (64/90) had STEMI (p<0.0001). Among plaque erosion, white thrombus was seen in 55.8% (24/43) of patients and red thrombus in 27.9% (12/43) of patients. Compared to plaque erosion, plaque rupture more often showed positive remodeling (p=0.003) with a larger necrotic core area examined by virtual histology (VH)-IVUS, while negative remodeling was prominent in plaque erosion. Overall, 65% 28/43 of plaque erosions were located in the proximal 30 mm of a culprit vessel-similar to plaque ruptures (72%, 65/90, p=0.29).
CONCLUSION
Although most of plaque erosions show nearly normal coronary angiogram, modest plaque burden with negative remodeling and an uncommon fibroatheroma might be the nature of plaque erosion. Multimodality intravascular imaging with OCT and VH-IVUS showed fundamentally different pathoanatomic substrates underlying plaque rupture and erosion.
MeSH Terms
Figure
Cited by 1 articles
-
Rediscover a Missed Culprit Lesion with Optical Coherence Tomography in Acute Coronary Syndrome: a Simple Stationary Pullback Method
Bino John Sahayo, Sundeep Mishra, Sang-Wook Kim, Arvind Dambalkar, Quang Tan Phan, Hoyoun Won, Jun Hwan Cho, Wang Soo Lee
Korean Circ J. 2020;50(11):1043-1044. doi: 10.4070/kcj.2020.0081.
Reference
-
1. Farb A, Burke AP, Tang AL, et al. Coronary plaque erosion without rupture into a lipid core: a frequent cause of coronary thrombosis in sudden coronary death. Circulation. 1996; 93:1354–1363.2. Virmani R, Burke AP, Farb A, Kolodgie FD. Pathology of the vulnerable plaque. J Am Coll Cardiol. 2006; 47:8 Suppl. C13–C18.3. Burke AP, Farb A, Malcom GT, Liang Y, Smialek J, Virmani R. Effect of risk factors on the mechanism of acute thrombosis and sudden coronary death in women. Circulation. 1998; 97:2110–2116.4. Hong YJ, Ahn Y, Jeong MH. Role of Intravascular Ultrasound in Patients with Acute Myocardial Infarction. Korean Circ J. 2015; 45:259–265.5. Sanidas EA, Maehara A, Mintz GS, et al. Angioscopic and virtual histology intravascular ultrasound characteristics of culprit lesion morphology underlying coronary artery thrombosis. Am J Cardiol. 2011; 107:1285–1290.6. Kim SW, Hong YJ, Mintz GS, et al. Relation of ruptured plaque culprit lesion phenotype and outcomes in patients with ST elevation acute myocardial infarction. Am J Cardiol. 2012; 109:794–799.7. Yabushita H, Bouma BE, Houser SL, et al. Characterization of human atherosclerosis by optical coherence tomography. Circulation. 2002; 106:1640–1645.8. Jang IK, Tearney GJ, MacNeill B, et al. In vivo characterization of coronary atheroscleroticplaque by use of optical coherence tomography. Circulation. 2005; 111:1551–1555.9. Kubo T, Imanishi T, Takarada S, et al. Assessment of culprit lesion morphology in acute myocardial infarction: ability of optical coherence tomography compared with intravascular ultrasound and coronary angioscopy. J Am Coll Cardiol. 2007; 50:933–939.10. Rathore S, Terashima M, Matsuo H, et al. Association of coronary plaque composition and arterial remodeling: an optical coherence tomography study. Atherosclerosis. 2012; 221:405–415.11. Jia H, Abtahian F, Aguirre AD, et al. In vivo diagnosis of plaque erosion and calcified nodule in patients with acute coronary syndrome by intravascular optical coherence tomography. J Am Coll Cardiol. 2013; 62:1748–1758.12. Ino Y, Kubo T, Tanaka A, et al. Difference of culprit lesion morphologies between ST-segment elevation myocardial infarction and non-ST-segment elevation acute coronary syndrome: an optical coherence tomography study. JACC Cardiovasc Interv. 2011; 4:76–82.13. Cho YK, Hur SH. Practical Application of Coronary Imaging Devices in Cardiovascular Intervention. Korean Circ J. 2015; 45:87–95.14. Tearney GJ, Regar E, Akasaka T, et al. International Working Group for Intravascular Optical Coherence Tomography (IWG-IVOCT). Consensus standards for acquisition, measurement, and reporting of intravascular optical coherence tomography studies: a report from the International Working Group for Intravascular Optical Coherence Tomography Standardization and Validation. J Am Coll Cardiol. 2012; 59:1058–1072.15. Mintz GS, Nissen SE, Anderson WD, et al. American College of Cardiology Clinical Expert Consensus Document on Standards for Acquisition, Measurement and Reporting of Intravascular Ultrasound Studies (IVUS). A report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2001; 37:1478–1492.16. García-García HM, Mintz GS, Lerman A, et al. Tissue characterisation using intravascular radiofrequency data analysis: recommendations for acquisition, analysis, interpretation and reporting. EuroIntervention. 2009; 5:177–189.17. Hayashi T, Kiyoshima T, Matsuura M, et al. Plaque erosion in the culprit lesion is prone to develop a smaller myocardial infarction size compared with plaque rupture. Am Heart J. 2005; 149:284–290.18. Hong MK, Mintz GS, Lee CW, et al. The site of plaque rupture in native coronary arteries: a three-vessel intravascular ultrasound analysis. J Am Coll Cardiol. 2005; 46:261–265.19. Fujii K, Masutani M, Okumura T, et al. Frequency and predictor of coronary thin-cap fibroatheroma in patients with acute myocardial infarction and stable angina pectoris a 3-vessel optical coherence tomography study. J Am Coll Cardiol. 2008; 52:787–788.20. Kume T, Okura H, Yamada R, et al. Frequency and spatial distribution of thin-cap fibroatheroma assessed by 3-vessel intravascular ultrasound and optical coherence tomography: an ex vivo validation and an initial in vivo feasibility study. Circ J. 2009; 73:1086–1091.21. Toutouzas K, Karanasos A, Riga M, et al. Optical coherence tomography assessment of the spatial distribution of culprit ruptured plaques and thin-cap fibroatheromas in acute coronary syndrome. EuroIntervention. 2012; 8:477–485.22. Schoenhagen P, Ziada KM, Kapadia SR, Crowe TD, Nissen SE, Tuzcu EM. Extent and direction of arterial remodeling in stable versus unstable coronary syndromes : an intravascular ultrasound study. Circulation. 2000; 101:598–603.23. Inaba S, Mintz GS, Farhat NZ, et al. Impact of positive and negative lesion site remodeling on clinical outcomes: insights from PROSPECT. JACC Cardiovasc Imaging. 2014; 7:70–78.24. Kramer MC, Rittersma SZ, de Winter RJ, et al. Relationship of thrombus healing to underlying plaque morphology in sudden coronary death. J Am Coll Cardiol. 2010; 55:122–132.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Plaque Morphology in Acute Coronary Syndrome: An Intravascular Ultrasound Study
- Advances in Intravascular Imaging: New Insights into the Vulnerable Plaque from Imaging Studies
- Lesion Characteristics in Patients with Acute Coronary Syndrome: A Comparison with Lesion in Patients with Stable Angina by Intravascular Ultrasound
- A case of acute myocardial infarction with plaque rupture in patient with hyperthyroidism
- Acute coronary syndrome and vulnerable plaque