Korean J Ophthalmol.
2014 Oct;28(5):386-392. 10.3341/kjo.2014.28.5.386.
Predictive Findings of Visual Outcome in Spectral Domain Optical Coherence Tomography after Ranibizumab Treatment in Age-related Macular Degeneration
- Affiliations
-
- 1Department of Ophthalmology, Dong-A University College of Medicine, Busan, Korea.
- 2Retina Center, Nune Eye Hospital, Seoul, Korea. owkwon0301@yuhs.ac
- KMID: 2344262
- DOI: http://doi.org/10.3341/kjo.2014.28.5.386
Abstract
- PURPOSE
To investigate which spectral domain optical coherence tomography (SD-OCT) findings predict visual outcome after anti-vascular endothelial growth factor (VEGF) treatment in neovascular age-related macular degeneration (NV-AMD).
METHODS
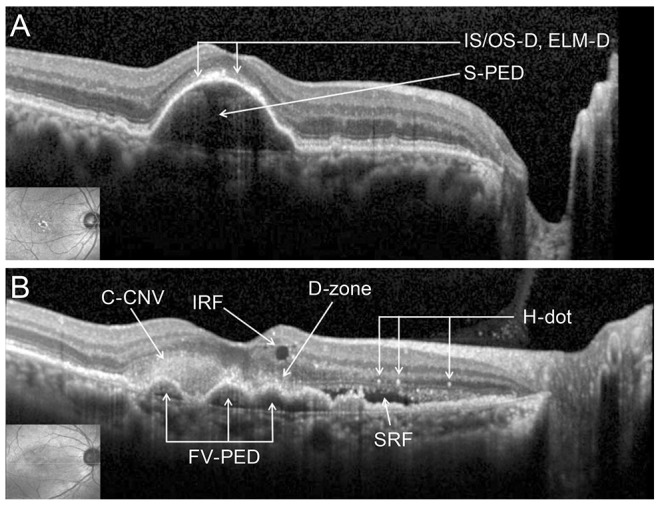
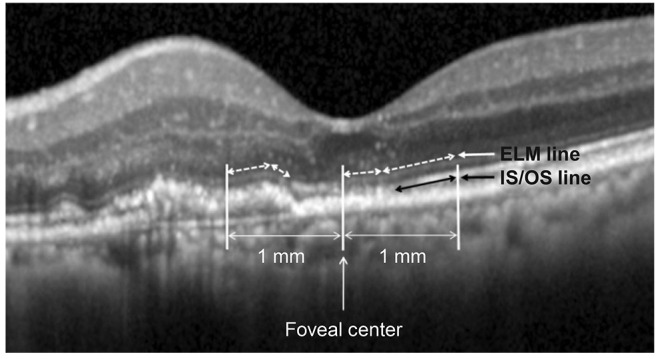
We reviewed the medical records of patients with treatment-naive NV-AMD who underwent three or more consecutive anti-VEGF injections. The patients were divided into three groups according to their changes of visual acuity (VA); improved (group I), static (group S), or worsened (group W). We assessed the incidences and values of all available SD-OCT findings of these groups, compared these findings between the three groups and compared the initial values with the post-treatment values.
RESULTS
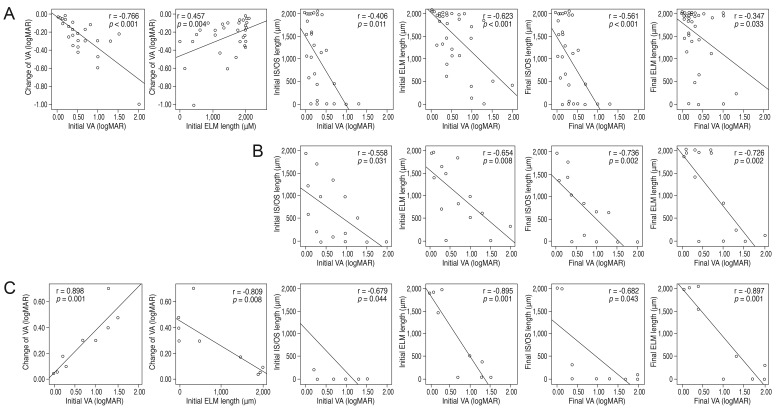
Better initial VA and longer external limiting membrane (ELM) length were associated with less change in VA after anti-VEGF treatment. The initial VA was mildly correlated with initial photoreceptor inner and outer segment junction (IS/OS) length and initial ELM length. The final VA was also mildly correlated with the final IS/OS length and the final ELM length. VA was significantly changed after anti-VEGF treatment in groups W and I. With regard to incidence, disruption of the IS/OS (IS/OS-D), disruption of the ELM (ELM-D) and ELM length differed significantly between the three groups, particularly ELM-D. The incidences of IS/OS-D and ELM-D in group I were significantly lower than those in groups S and W, and those in group S were also lower than those in group W. The ELM length in group I was significantly longer than it was in groups S and W, and the ELM length in group S was longer than that for group W. However, these three findings did not change after the anti-VEGF treatment.
CONCLUSIONS
Initial IS/OS-D, ELM length and particularly ELM-D can be useful predictors of the visual outcome after anti-VEGF treatment in NV-AMD patients.
MeSH Terms
-
Aged
Aged, 80 and over
Angiogenesis Inhibitors/*therapeutic use
Choroidal Neovascularization/*drug therapy/physiopathology
Female
Humans
Intravitreal Injections
Male
Middle Aged
Ranibizumab/*therapeutic use
Retinal Photoreceptor Cell Inner Segment/pathology
Retinal Photoreceptor Cell Outer Segment/pathology
Tomography, Optical Coherence
Vascular Endothelial Growth Factor A/antagonists & inhibitors
Visual Acuity/*physiology
Wet Macular Degeneration/*drug therapy/physiopathology
Angiogenesis Inhibitors
Ranibizumab
Vascular Endothelial Growth Factor A
Figure
Reference
-
1. Dadgostar H, Waheed N. The evolving role of vascular endothelial growth factor inhibitors in the treatment of neovascular age-related macular degeneration. Eye (Lond). 2008; 22:761–767. PMID: 18388961.
Article2. Joeres S, Kaplowitz K, Brubaker JW, et al. Quantitative comparison of optical coherence tomography after pegaptanib or bevacizumab in neovascular age-related macular degeneration. Ophthalmology. 2008; 115:347–354.e2. PMID: 17628685.
Article3. Kaiser PK, Blodi BA, Shapiro H, et al. Angiographic and optical coherence tomographic results of the MARINA study of ranibizumab in neovascular age-related macular degeneration. Ophthalmology. 2007; 114:1868–1875. PMID: 17628683.
Article4. Treatment of age-related macular degeneration with photodynamic therapy (TAP) Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: one-year results of 2 randomized clinical trials: TAP report. Arch Ophthalmol. 1999; 117:1329–1345. PMID: 10532441.5. Verteporfin In Photodynamic Therapy Study Group. Verteporfin therapy of subfoveal choroidal neovascularization in age-related macular degeneration: two-year results of a randomized clinical trial including lesions with occult with no classic choroidal neovascularization: verteporfin in photodynamic therapy report 2. Am J Ophthalmol. 2001; 131:541–560. PMID: 11336929.6. Bressler NM. Treatment of Age-Related Macular Degeneration with Photodynamic Therapy (TAP) Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: two-year results of 2 randomized clinical trials-tap report 2. Arch Ophthalmol. 2001; 119:198–207. PMID: 11176980.7. Hayashi H, Yamashiro K, Tsujikawa A, et al. Association between foveal photoreceptor integrity and visual outcome in neovascular age-related macular degeneration. Am J Ophthalmol. 2009; 148:83–89.e1. PMID: 19327745.
Article8. Sayanagi K, Sharma S, Kaiser PK. Photoreceptor status after antivascular endothelial growth factor therapy in exudative age-related macular degeneration. Br J Ophthalmol. 2009; 93:622–626. PMID: 19208677.
Article9. Hagan MJ, Alvarado JA, Weddell JE. Histology of the human eye: an atlas and textbook. Philadelphia: Saunders;1971. p. 393–522.10. Shin HJ, Chung H, Kim HC. Association between foveal microstructure and visual outcome in age-related macular degeneration. Retina. 2011; 31:1627–1636. PMID: 21606888.
Article11. Oishi A, Hata M, Shimozono M, et al. The significance of external limiting membrane status for visual acuity in age-related macular degeneration. Am J Ophthalmol. 2010; 150:27–32.e1. PMID: 20609705.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Correlation between Visual Outcomes and Pre-Treatment Factors Including Hyperreflective Foci in Neovascular Age-Related Macular Degeneration
- Repeatability of Spectral Domain OCT (3D-OCT 1000) in Normal Subjects and Various Macular Diseases
- Macular Thickness Changes with Age and Gender in Emmetropia Using Spectral Domain Optical Coherence Tomography
- Analysis of Factors Associated with Variability in Measures Obtained by Spectral Domain Optical Coherence Tomography
- Comparison between Aflibercept, Ranibizumab Intravitreal Injection on Neovascular Age-related Macular Degeneration Patients