J Korean Med Sci.
2015 Oct;30(10):1446-1452. 10.3346/jkms.2015.30.10.1446.
Role of Atypical Pathogens and the Antibiotic Prescription Pattern in Acute Bronchitis: A Multicenter Study in Korea
- Affiliations
-
- 1Division of Pulmonary, Allergy and Critical Care Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea. pulmoks@hallym.ac.kr
- 2Myeongmun Clinic of Internal Medicine, Yongin, Korea.
- 3Joeun Clinic of Internal Medicine, Dangjin, Korea.
- 4Neulpurun Clinic of Otolaryngology, Anyang, Korea.
- 5Division of Pulmonary, Allergy and Critical Care Medicine, Konkuk University Hospital, Seoul, Korea.
- 6Division of Pulmonary, Allergy and Critical Care Medicine, Kangnam Sacred Heart Hospital, Seoul, Korea.
- 7Pyeongchon-Family Clinic of Internal Medicine, Anyang, Korea.
- 8Division of Pulmonary, Allergy and Critical Care Medicine, Chuncheon Sacred Heart Hospital, Chuncheon, Korea.
- 9Haengbok-Dream Clinic of Internal Medicine, Daegu, Korea.
- 10Hanyang Clinic of Internal Medicine, Seoul, Korea.
- 11Division of Pulmonary, Allergy and Critical Care Medicine, Kyung Hee University, Seoul, Korea.
- 12Hongjunggon Clinic of Internal Medicine, Anyang, Korea.
- 13Rapha Clinic of Otolaryngology, Anyang, Korea.
- 14Chahyunggun Clinic of Otolaryngology, Anyang, Korea.
- 15Leejaemyung Clinic of Internal Medicine, Anyang, Korea.
- 16Seojungsan Clinic of Internal Medicine, Seoul, Korea.
- KMID: 2344177
- DOI: http://doi.org/10.3346/jkms.2015.30.10.1446
Abstract
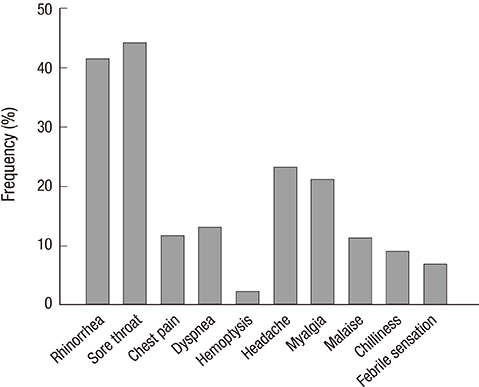
- The role of atypical bacteria and the effect of antibiotic treatments in acute bronchitis are still not clear. This study was conducted at 22 hospitals (17 primary care clinics and 5 university hospitals) in Korea. Outpatients (aged > or = 18 yr) who had an acute illness with a new cough and sputum (< or = 30 days) were enrolled in 2013. Multiplex real-time polymerase chain reaction (RT-PCR) was used to detect five atypical bacteria. A total of 435 patients were diagnosed as having acute bronchitis (vs. probable pneumonia, n = 75), and 1.8% (n = 8) were positive for atypical pathogens (Bordetella pertussis, n = 3; B. parapertussis, n = 0; Mycoplasma pneumoniae, n = 1; Chlamydophila pneumoniae, n = 3; Legionella pneumophila, n = 1). Among clinical symptoms and signs, only post-tussive vomiting was more frequent in patients with atypical pathogens than those without (P = 0.024). In all, 72.2% of the enrolled patients received antibiotic treatment at their first visits, and beta-lactams (29.4%) and quinolones (20.5%) were the most commonly prescribed agents. In conclusion, our study demonstrates that the incidence of atypical pathogens is low in patients with acute bronchitis, and the rate of antibiotic prescriptions is high.
Keyword
MeSH Terms
-
Anti-Bacterial Agents/therapeutic use
Bordetella parapertussis/genetics/*isolation & purification
Bordetella pertussis/genetics/*isolation & purification
Bronchitis/drug therapy/*microbiology
Chlamydophila pneumoniae/genetics/*isolation & purification
Community-Acquired Infections/microbiology
Female
Humans
Hypertension/complications
Legionella pneumophila/genetics/*isolation & purification
Male
Middle Aged
Mycoplasma pneumoniae/genetics/*isolation & purification
Real-Time Polymerase Chain Reaction
Republic of Korea
Sputum/microbiology
Anti-Bacterial Agents
Figure
Cited by 1 articles
-
Evaluation of EuDx TM-PN MLC Detection Kit for Detection of
Mycoplasma pneumoniae, Chlamydophila pneumoniae , andLegionella pneumophila in Respiratory Specimens
Mi-Kyung Lee, Heungsup Sung, Ah Ra Cho, Hyun Young Chi
Ann Clin Microbiol. 2017;20(4):97-102. doi: 10.5145/ACM.2017.20.4.97.
Reference
-
1. Macfarlane J, Holmes W, Gard P, Macfarlane R, Rose D, Weston V, Leinonen M, Saikku P, Myint S. Prospective study of the incidence, aetiology and outcome of adult lower respiratory tract illness in the community. Thorax. 2001; 56:109–114.2. Gonzales R, Sande MA. Uncomplicated acute bronchitis. Ann Intern Med. 2000; 133:981–991.3. Creer DD, Dilworth JP, Gillespie SH, Johnston AR, Johnston SL, Ling C, Patel S, Sanderson G, Wallace PG, McHugh TD. Aetiological role of viral and bacterial infections in acute adult lower respiratory tract infection (LRTI) in primary care. Thorax. 2006; 61:75–79.4. Park S, Lee MG, Lee KH, Park YB, Yoo KH, Park JW, Kim C, Lee YC, Park JS, Kwon YS, et al. A multicenter study of pertussis infection in adults with coughing in korea: PCR-based study. Tuberc Respir Dis. 2012; 73:266–272.5. Ward JI, Cherry JD, Chang SJ, Partridge S, Lee H, Treanor J, Greenberg DP, Keitel W, Barenkamp S, Bernstein DI, et al. APERT Study Group. Efficacy of an acellular pertussis vaccine among adolescents and adults. N Engl J Med. 2005; 353:1555–1563.6. Denny FW, Clyde WA Jr, Glezen WP. Mycoplasma pneumoniae disease: clinical spectrum, pathophysiology, epidemiology, and control. J Infect Dis. 1971; 123:74–92.7. Grayston JT, Kuo CC, Wang SP, Altman J. A new Chlamydia psittaci strain, TWAR, isolated in acute respiratory tract infections. N Engl J Med. 1986; 315:161–168.8. Fahey T, Stocks N, Thomas T. Quantitative systematic review of randomised controlled trials comparing antibiotic with placebo for acute cough in adults. BMJ. 1998; 316:906–910.9. Gonzales R, Steiner JF, Lum A, Barrett PH Jr. Decreasing antibiotic use in ambulatory practice: impact of a multidimensional intervention on the treatment of uncomplicated acute bronchitis in adults. JAMA. 1999; 281:1512–1519.10. Cho CH, Chulten B, Lee CK, Nam MH, Yoon SY, Lim CS, Cho Y, Kim YK. Evaluation of a novel real-time RT-PCR using TOCE technology compared with culture and Seeplex RV15 for simultaneous detection of respiratory viruses. J Clin Virol. 2013; 57:338–342.11. Kim HK, Oh SH, Yun KA, Sung H, Kim MN. Comparison of Anyplex II RV16 with the xTAG respiratory viral panel and Seeplex RV15 for detection of respiratory viruses. J Clin Microbiol. 2013; 51:1137–1141.12. Boldy DA, Skidmore SJ, Ayres JG. Acute bronchitis in the community: clinical features, infective factors, changes in pulmonary function and bronchial reactivity to histamine. Respir Med. 1990; 84:377–385.13. Albert RH. Diagnosis and treatment of acute bronchitis. Am Fam Physician. 2010; 82:1345–1350.14. Holm A, Nexoe J, Bistrup LA, Pedersen SS, Obel N, Nielsen LP, Pedersen C. Aetiology and prediction of pneumonia in lower respiratory tract infection in primary care. Br J Gen Pract. 2007; 57:547–554.15. Powell DA, Hu PC, Wilson M, Collier AM, Baseman JB. Attachment of Mycoplasma pneumoniae to respiratory epithelium. Infect Immun. 1976; 13:959–966.16. Lee SJ, Lee MG, Jeon MJ, Jung KS, Lee HK, Kishimoto T. Atypical pathogens in adult patients admitted with community-acquired pneumonia in Korea. Jpn J Infect Dis. 2002; 55:157–159.17. Block S, Hedrick J, Hammerschlag MR, Cassell GH, Craft JC. Mycoplasma pneumoniae and Chlamydia pneumoniae in pediatric community-acquired pneumonia: comparative efficacy and safety of clarithromycin vs. erythromycin ethylsuccinate. Pediatr Infect Dis J. 1995; 14:471–477.18. Cosentini R, Blasi F, Raccanelli R, Rossi S, Arosio C, Tarsia P, Randazzo A, Allegra L. Severe community-acquired pneumonia: a possible role for Chlamydia pneumoniae. Respiration. 1996; 63:61–65.19. Woodhead M. Community-acquired pneumonia in Europe: causative pathogens and resistance patterns. Eur Respir J Suppl. 2002; 36:20s–27s.20. Lieberman D, Lieberman D, Ben-Yaakov M, Lazarovich Z, Ohana B, Friedman MG, Dvoskin B, Leinonen M, Boldur I. Infectious aetiologies in elderly patients hospitalised with non-pneumonic lower respiratory tract infection. Age Ageing. 2003; 32:95–101.21. Lieberman D, Lieberman D, Korsonsky I, Ben-Yaakov M, Lazarovich Z, Friedman MG, Dvoskin B, Leinonen M, Ohana B, Boldur I. A comparative study of the etiology of adult upper and lower respiratory tract infections in the community. Diagn Microbiol Infect Dis. 2002; 42:21–28.22. Macfarlane J, Prewett J, Rose D, Gard P, Cunningham R, Saikku P, Euden S, Myint S. Prospective case-control study of role of infection in patients who reconsult after initial antibiotic treatment for lower respiratory tract infection in primary care. BMJ. 1997; 315:1206–1210.23. Macfarlane JT, Colville A, Guion A, Macfarlane RM, Rose DH. Prospective study of aetiology and outcome of adult lower-respiratory-tract infections in the community. Lancet. 1993; 341:511–514.24. Cherry JD. Epidemic pertussis in 2012-- the resurgence of a vaccine-preventable disease. N Engl J Med. 2012; 367:785–787.25. Park S, Lee SH, Seo KH, Shin KC, Park YB, Lee MG, Yoo KH, Kim HJ, Park JS, Cho JH, et al. Epidemiological aspects of pertussis among adults and adolescents in a Korean outpatient setting: a multicenter, PCR-based study. J Korean Med Sci. 2014; 29:1232–1239.26. Park WB, Park SW, Kim HB, Kim EC, Oh M, Choe KW. Pertussis in adults with persistent cough in South Korea. Eur J Clin Microbiol Infect Dis. 2005; 24:156–158.27. Cherry JD. The epidemiology of pertussis: a comparison of the epidemiology of the disease pertussis with the epidemiology of Bordetella pertussis infection. Pediatrics. 2005; 115:1422–1427.28. Lieberman D, Shvartzman P, Lieberman D, Ben-Yaakov M, Lazarovich Z, Hoffman S, Mosckovitz R, Ohana B, Leinonen M, Luffy D, et al. Etiology of respiratory tract infection in adults in a general practice setting. Eur J Clin Microbiol Infect Dis. 1998; 17:685–689.29. Wadowsky RM, Castilla EA, Laus S, Kozy A, Atchison RW, Kingsley LA, Ward JI, Greenberg DP. Evaluation of Chlamydia pneumoniae and Mycoplasma pneumoniae as etiologic agents of persistent cough in adolescents and adults. J Clin Microbiol. 2002; 40:637–640.30. Bent S, Saint S, Vittinghoff E, Grady D. Antibiotics in acute bronchitis: a meta-analysis. Am J Med. 1999; 107:62–67.31. Evans AT, Husain S, Durairaj L, Sadowski LS, Charles-Damte M, Wang Y. Azithromycin for acute bronchitis: a randomised, double-blind, controlled trial. Lancet. 2002; 359:1648–1654.32. Smucny J, Fahey T, Becker L, Glazier R. Antibiotics for acute bronchitis. Cochrane Database Syst Rev. 2004; 14:CD000245.33. Wilson AA, Crane LA, Barrett PH, Gonzales R. Public beliefs and use of antibiotics for acute respiratory illness. J Gen Intern Med. 1999; 14:658–662.34. Kim SH, Song JH, Chung DR, Thamlikitkul V, Yang Y, Wang H, Lu M, So TM, Hsueh PR, Yasin RM, et al. ANSORP Study Group. Changing trends in antimicrobial resistance and serotypes of Streptococcus pneumoniae isolates in Asian countries: an Asian Network for Surveillance of Resistant Pathogens (ANSORP) study. Antimicrob Agents Chemother. 2012; 56:1418–1426.35. Mainous AG 3rd, Saxena S, Hueston WJ, Everett CJ, Majeed A. Ambulatory antibiotic prescribing for acute bronchitis and cough and hospital admissions for respiratory infections: time trends analysis. J R Soc Med. 2006; 99:358–362.36. Thom DH, Grayston JT, Campbell LA, Kuo CC, Diwan VK, Wang SP. Respiratory infection with Chlamydia pneumoniae in middle-aged and older adult outpatients. Eur J Clin Microbiol Infect Dis. 1994; 13:785–792.37. Jonsson JS, Sigurdsson JA, Kristinsson KG, Guthnadóttir M, Magnusson S. Acute bronchitis in adults. How close do we come to its aetiology in general practice? Scand J Prim Health Care. 1997; 15:156–160.38. Meijer A, Dagnelie CF, De Jong JC, De Vries A, Bestebroer TM, Van Loon AM, Bartelds AI, Ossewaarde JM. Low prevalence of Chlamydia pneumoniae and Mycoplasma pneumoniae among patients with symptoms of respiratory tract infections in Dutch general practices. Eur J Epidemiol. 2000; 16:1099–1106.39. Graffelman AW, Knuistingh Neven A, le Cessie S, Kroes AC, Springer MP, van den Broek PJ. Pathogens involved in lower respiratory tract infections in general practice. Br J Gen Pract. 2004; 54:15–19.40. Gaillat J, Flahault A, deBarbeyrac B, Orfila J, Portier H, Ducroix JP, Bébéar C, Mayaud C. Community epidemiology of Chlamydia and Mycoplasma pneumoniae in LRTI in France over 29 months. Eur J Epidemiol. 2005; 20:643–651.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prescription Pattern of Atypical Antipsychotics in a University Psychiatric Ward : 11-Year Observational Study
- Survey on Physician Attitude of Antibiotic Prescription for Upper Respiratory Tract Infections
- Antibiotic Use in Korean Children Diagnosed With Acute Bronchiolitis: Analysis of the National Health Insurance Reimbursement Data
- Appropriate Use of Antibiotics for the Treatment of Acute Upper Respiratory Tract Infections in Adults
- Factors Influencing Antibiotics Prescribing of Primary Health Physicians in Acute Upper Respiratory Infections