J Korean Med Assoc.
2006 Mar;49(3):253-271.
Epilepsy Surgery I
- Affiliations
-
- 1Department of Neurology, Sungkyunkwan University School of Medicine, Samsung Medical Center, Korea. sbhong@smc.samsung.co.kr, jey1220@freechal.com
Abstract
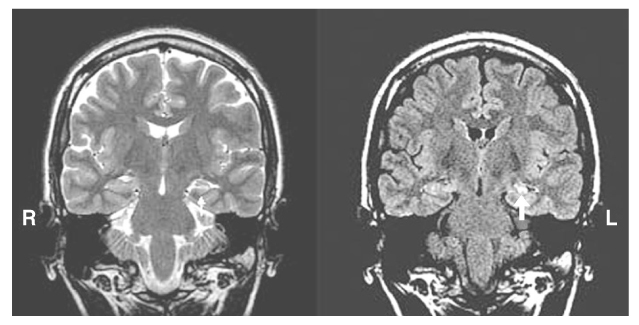
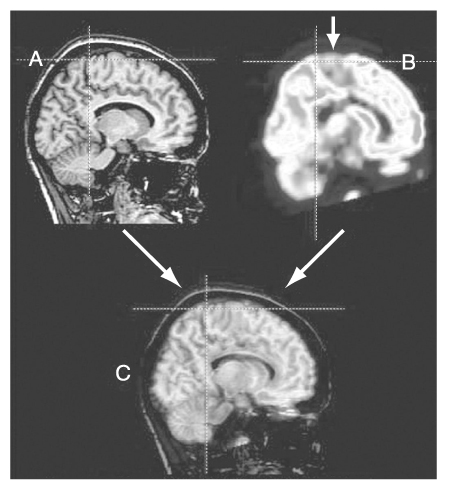
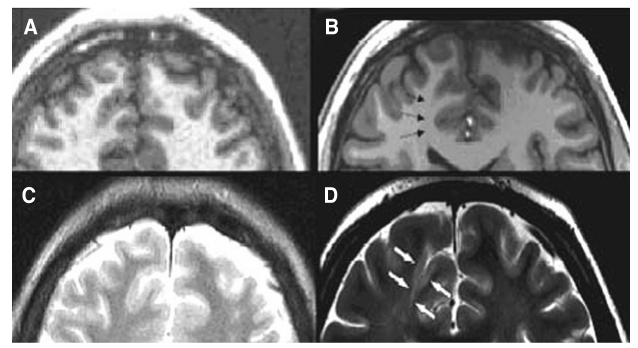
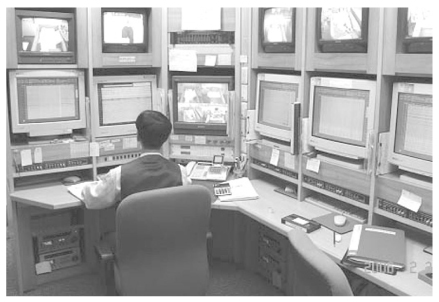
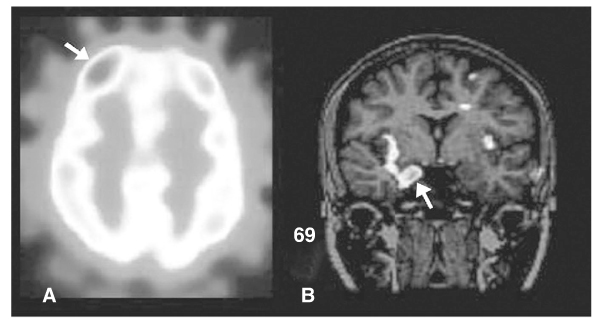
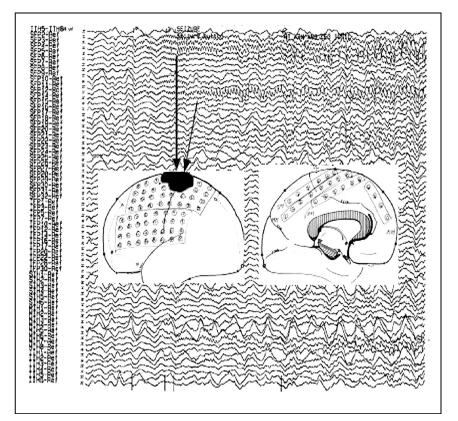
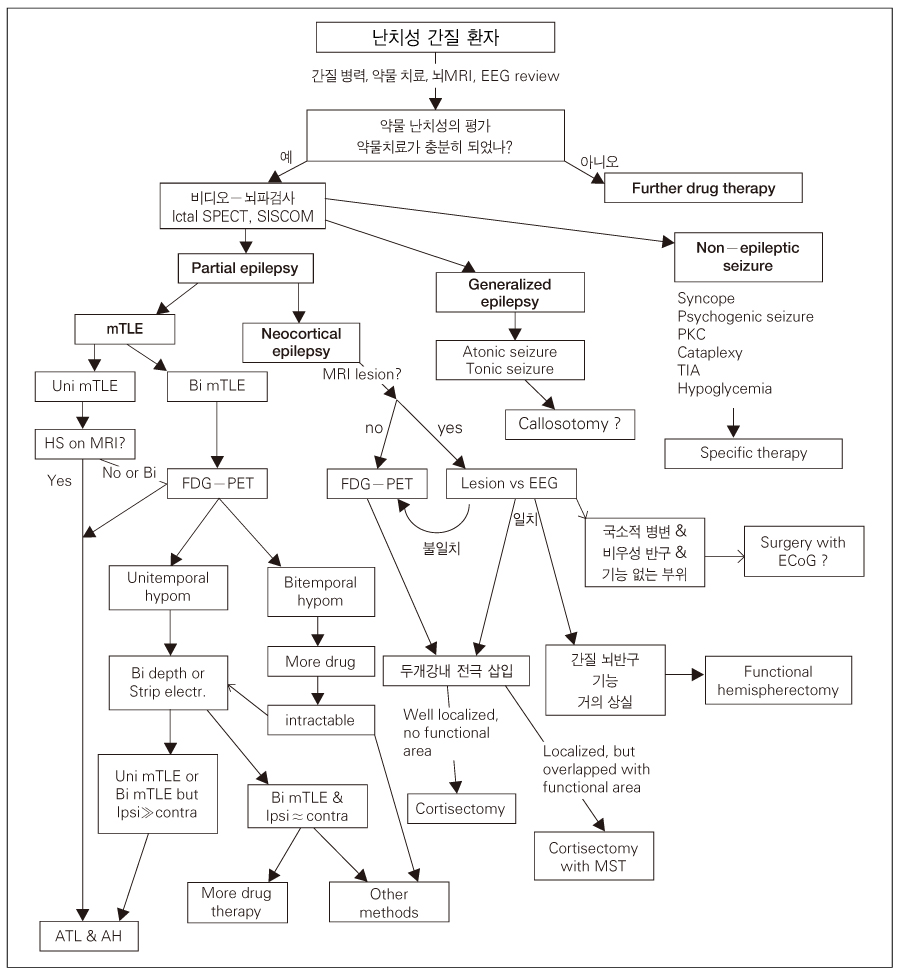
- Epilepsy is a chronic neurological disorder manifesting recurrent unprovoked epileptic seizures. About 20~30% of epilepsy patients are resistant to antiepileptic medications. These patients suffer from high risk of physical injury, unemployment, marital problem, and psychological stress. Epilepsy surgery is the firstly recommended treatment modality for the patients with medically intractable epilepsy. Presurgical evaluation is the most important process for performing epilepsy surgery. The ultimate goal of the presurgical evaluation in patients with medically refractory partial seizures is the localization of the epileptogenic zone and the resection of which is also both necessary and sufficient to render the patient seizure-free. The localization of the epileptogenic zone derives from a hierarchical synthesis of localizing data independently obtained from clinical, electrographic, neuroimaging, and neuropsychological examination. In addition, closely related to the goal of localizing the epileptogenic zone is the significant need for anticipating the risks of functional deficits that could derive from the surgical resection. Mesial temporal lobe epilepsy (TLE) is the best candidate for epilepsy surgery. Anterior temporal lobectomy with amygdalohippocampectomy is a surgical treatment method for mesial TLE and its seizure-free rate (SFR) is 60~90%, whereas one-year SFR of antiepileptic drug treatment for mesial TLE is 10~20%. Cortisectomy is a surgical method for extratemporal epilepsy and its SFR is about 40~70%. Corpus callosotomy is a partial or complete division of corpus callosum for preventing seizure propagations between right and left hemispheres and is effective for controlling atonic seizures. The variation of postsurgical seizure outcomes is related to the qualities of epilepsy surgery program, presurgical evaluation and surgical techniques. For the good surgical outcome, the epilepsy surgery program should include neurologist, neurosurgeon, neuropsychologist, neuro-radiologist and neuro-nuclear medicine specialist for a comprehensive team approach.
Keyword
MeSH Terms
Figure
Reference
-
1. Penfield W, Flanigin H. Surgical therapy of temporal lobe seizures. Arch Neurol Psychiatry. 1950. 64:491–500.
Article2. Bailey P, Gobbs FA. The surgical treatment of psychomotor epilepsy. J Am Med Assoc. 1951. 145:365–370.
Article3. Engel J Jr, Wiebe S, French J, Sperling M, Williamson P, Enos B, et al. Practice parameter: temporal lobe and localized neocortical resections for epilepsy. Epilepsia. 2003. 44:741–751.
Article4. Semah F, Picot MC, Adam C, Broglin D, Arzimanoglou A, Baulac M, et al. Is the underlying cause of epilepsy a major prognostic factor for recurrence? Neurology. 1998. 51:1256–1262.
Article5. Wiebe S, Blume WT, Girvin JP, Eliasziw M. A randomized, controlled trial of surgery for temporal-lobe epilepsy. N Engl J Med. 2001. 345:311–318.
Article6. Kuzniecky R, Jackson G. Neuroimaging in epilepsy: magnetic resonance in epilepsy. 1995. New York: Raven Press;27–48.7. Jack CR Jr, Sharbrough FW, Twomey CK, et al. Temporal lobe seizures: lateralization with MR volume measurements of the hippocampal formations. Radiology. 1990. 175:423–429.
Article8. Jack C, Rydberg C, Kreacker K, et al. Mesial temporal sclerosis: diagnosis with FLAIR versus spin-echo MR imaging. Radiology. 1996. 199:367–373.
Article9. Jackson GD, Berkovic SF, Duncan JS, et al. Optimizing the diagnosis of hippocampal sclerosis using magnetic resonance imaging. AJNR Am J Neuroradiol. 1993. 14:753–762.10. Kuzniecky R, Cascino GD, Palmini A, et al. Engel J, editor. Structural imaging. Surgical treatment of the epilepsies. 1993. 2nd ed. New York: Raven Press;197–200.11. Gadian DG. Nuclear magnetic resonance and its applications to living systems. 1982. New York: Oxford University Press.12. Cascino GD, Jack CR Jr, Hirschorn KA, Sharbrough FW. Identification of the epileptic focus: magnetic resonance imaging. Epilepsy Res Suppl. 1992. 5:95–100.13. Knake S, Triantafyllou C, Wald LL, Wiggins G, Kirk GP, Grant PE, et al. 3T phased array MRI improves the presurgical evaluation in focal epilepsies: a prospective study. Neurology. 2005. 65:1026–1031.
Article14. Lagerlund TD, Cascino GD, Cicora KM, Sharbrough FW. Long-term electroencephalographic monitoring for diagnosis and management of seizures. Mayo Clin Proc. 1996. 71:1000–1006.
Article16. Spencer SS, Theodore WH, Berkovic SF. Clnical applications: MRI, SPECT, and PET. Magn Reson Imaging. 1995. 13:1119–1124.17. Lee HW, Hong SB, Tae WS. Opposite ictal perfusion patterns of subtracted SPECT. Hyperperfusion and hypoperfusion. Brain. 2000. 123:2150–2150.
Article18. O'Brien TJ, So EL, Mullan BP, et al. Subtraction peri-ictal SPECT is predictive of extratemporal epilepsy surgery outcome. Neurology. 2000. 55:1668.19. Choi JY, Kim SJ, Hong SB, et al. Extratemporal hypometabolism on FDG PET in temporal lobe epilepsy as a predictor of seizure outcome after temporal lobectomy. Eur J Nucl Med Mol Imaging. 2003. 30:581–587.
Article20. Hong SB, Kim KW, Seo DW, Kim SE, Na DG, Byun HS. Contralateral EEG slowing and amobarbital distribution in Wada test: an intracarotid SPECT study. Epilepsia. 2000. 41:207–212.
Article21. Hong SB, Han HJ, Roh SY, Seo DW, Kim SE, Kim MH. Hypometabolism and interictal spikes during positron emission tomography scanning in temporal lobe epilepsy. Eur Neurol. 2002. 48:65–70.
Article22. Behrens E, Zentner J, van Roost D, Hufnagel A, Elger CE, Schramm J. Subdural and depth electrodes in the presurgical evaluation of epilepsy. Acta Neurochir (Wien). 1994. 128:84–87.
Article23. Wass CT, Grady RE, Fessler AJ, et al. The effects of remifentanil on epileptiform discharges during intraoperative electrocorticography in patients undergoing epilepsy surgery. Epilepsia. 2001. 42:1340–1344.
Article24. Fiol ME, Gates JR, Torres F, Maxwell RE. The prognostic value of residual spikes in the postexcision electrocorticogram after temporal lobectomy. Neurology. 1991. 41:512–516.
Article25. Engel J Jr, Wiebe S, French J, Sperling M, Williamson P, Gumnit R, et al. Practice parameter: temporal lobe and localized neocortical resections for epilepsy: report of the Quality Standards Subcommittee of the American Academy of Neurology, in association with the American Epilepsy Society and the American Association of Neurological Surgeons. Neurology. 2003. 60:538–547.
Article26. Daniel RT, Joseph TP, Gnanamuthu C, Chandy MJ. Hemispherotomy for paediatric hemispheric epilepsy. Stereotact Funct Neurosurg. 2001. 77:219–222.
Article27. Pulsifer MB, Brandt J, Salorio CF, Vining EP, Carson BS, Freeman JM. The cognitive outcome of hemispherectomy in 71 children. Epilepsia. 2004. 45:243–254.
Article28. Spencer SS, Schramm J, Wyler A, O'Connor M, Orbach D, Krauss G, et al. Multiple subpial transection for intractable partial epilepsy: an international meta-analysis. Epilepsia. 2002. 43:141–145.
Article29. Orbach D, Romanelli P, Devinsky O, Doyle W. Late seizure recurrence after multiple subpial transections. Epilepsia. 2001. 42:1130–1133.
Article30. Tellez-Zenteno JF, Dhar R, Wiebe S. Long-term seizure outcomes following epilepsy surgery: a systematic review and meta-analysis. Brain. 2005. 128:1188–1198.
Article31. Sass KJ, Spencer DD, Spencer SS, Novelly RA, Williamson PD, Mattson RH. Corpus callosotomy for epilepsy. II. Neurologic and neuropsychological outcome. Neurology. 1988. 38:24–28.
Article32. Spencer SS, Spencer DD, Williamson PD, Sass K, Novelly RA, Mattson RH. Corpus callosotomy for epilepsy. I. Seizure effects. Neurology. 1988. 38:19–24.
Article