J Korean Ophthalmol Soc.
2014 Aug;55(8):1248-1252.
A Case of Bilateral Central Serous Chorioretinopathy after Blunt Trauma
- Affiliations
-
- 1Department of Ophthalmology, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea. hyuny@medimail.co.kr
Abstract
- PURPOSE
To report a case of bilateral central serous chorioretinopathy (CSC) after blunt trauma with rapid remission.
CASE SUMMARY
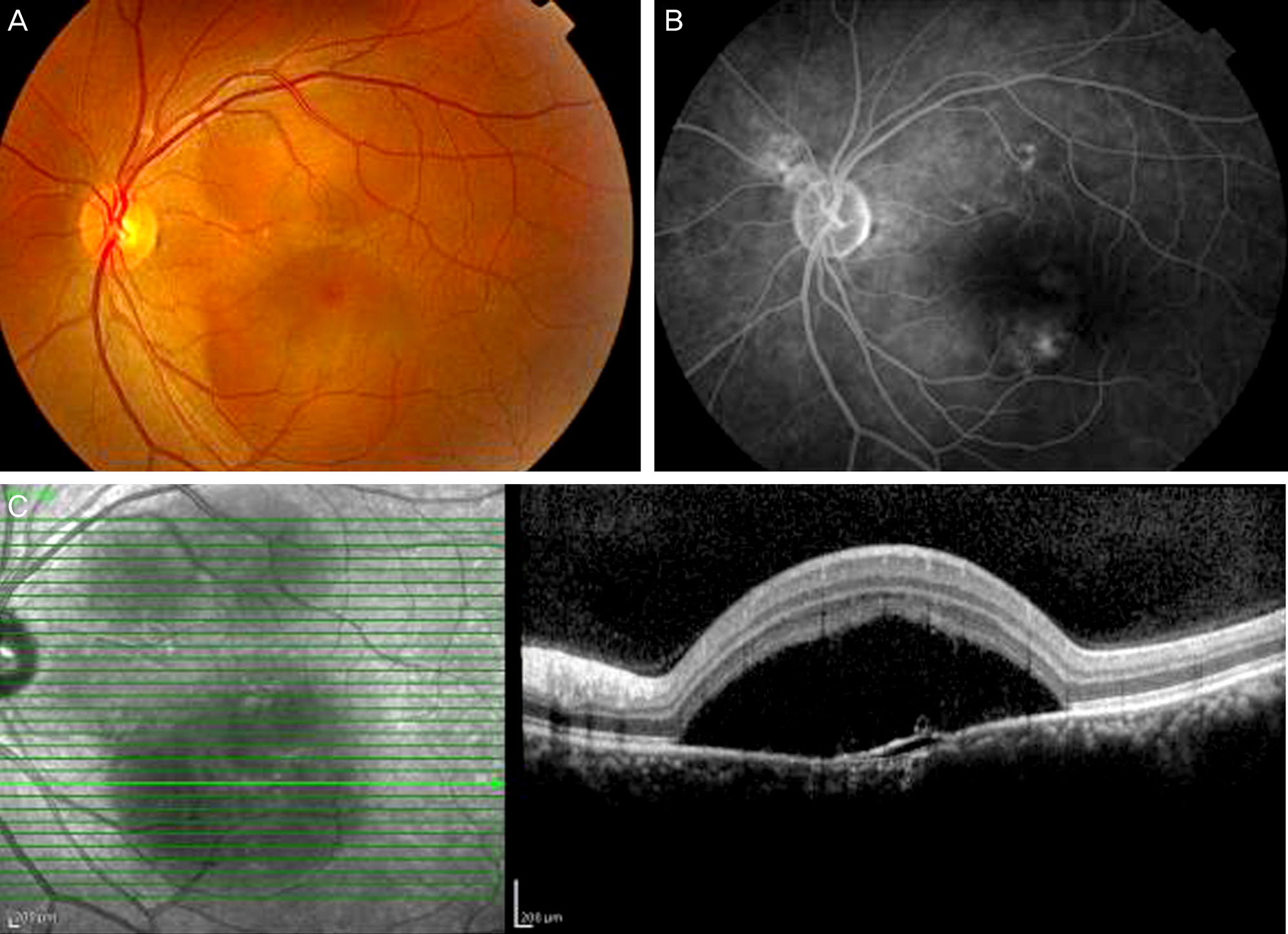
A 44-year-old man visited our clinic after blunt trauma around the right eye. At the first examination, no ocular problem was detected except a periorbital contusion. After one week, the patient complained of visual disturbance in his right eye. Fundus examination showed subretinal fluid in his right eye, and fluorescein angiography (FAG) showed typical smoke-stack pattern leakage, which lead to a diagnosis of CSC. Three days later, the patient complained of visual disturbance in his left eye, which was then also diagnosed as CSC. After 2 more weeks, the subretinal fluid in the right and left eyes had decreased. After 3 weeks, the subretinal fluid was almost completely absorbed in both eyes.
CONCLUSIONS
Central serous chorioretinopathy can develop after blunt trauma, especially with a rapid clinical course. Thus, periodic ophthalmologic examination is needed after the first examination for blunt trauma of the eye.
Keyword
MeSH Terms
Figure
Reference
-
References
1. von Graefe A. Ueber centrale recidivirende retinitis. Graefes Arch Clin Exp Ophthalmol. 1866; 12:211–5.2. Gass JD. Pathogenesis of disciform detachment of the neuroepithelium II. Idiopathic central serous chorioretinopathy. Am J Ophthalmol. 1967; 63:587–615.3. Gelber GS, Schatz H. Loss of vision due to central serous chorioretinopathy following psychological stress. Am J Psychiatry. 1987; 144:46–50.4. Yannuzzi LA. Type-A behavior and central serous chorioretinopathy. Retina. 1987; 7:111–31.
Article5. Spitznas M. Pathogenesis of central serous retinopathy: a new working hypothesis. Graefes Arch Clin Exp Ophthalmol. 1986; 224:321–4.
Article6. Marmor MF. New hypothesis on the pathogenesis and treatment of serous retinal detachment. Graefes Arch Clin Exp Ophthalmol. 1988; 226:548–52.7. Wakakura M, Ichikawa S. Central serous chorioretinopathy complicating systemic corticosteroid treatment. Br J Ophthalmol. 1984; 68:329–31.
Article8. Kang SW, Park JS. A Study on stress and personality characteristics of the central serous chorioretinopathy patients. J Korean Ophthalmol Soc. 1999; 40:1012–9.9. Gackle HC, Lang GE, Freissler KA, Lang GK. Central serous chorioretinopathy. Clinical, fluorescein angiography and demographic aspects. Ophthalmologe. 1998; 95:529–3.10. Kitzmann AS, Pulido JS, Diehl NN, et al. The incidence of central serous chorioretinopathy in Olmsted County, Minnesota, 1980-2002. Ophthalmology. 2008; 115:169–73.
Article11. Oosterhuis JA. Familial central serous retinopathy. Graefes Arch Clin Exp Ophthalmol. 1996; 234:337–41.
Article12. Jackson TE, Sood V, Haigh PM. Central serous chorioretinopathy secondary to trauma. Oman J Ophthalmol. 2012; 5:51–2.
Article13. Ponce CM, Mohidat HM, Garcia CA. Central serous chorioretinopathy after blunt trauma. BMJ Case Rep. 2012; 2012.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of Atypical Central Serous Chorioretinopathy with Bullous Retinal Detachment
- A Case of Bilateral Central Serous Chorioretinopathy in a Chronic Tibial Osteomyelitis Patient
- A Case of Central Serous Chorioretinopathy Following Systemic Corticosteroid Therapy
- A Case of Atypical Idiopathic Central Serous Chorioretinopathy
- Electronmicroscopic Study of the Effect of Hexamethonium on Serous Choriretinopathy in Rabbits