J Korean Ophthalmol Soc.
2014 Apr;55(4):541-547.
The Intima Media Thickness (IMT) as Measured by Carotid Ultrasonography in Patients with Retinal Vascular Diseases
- Affiliations
-
- 1Department of Ophthalmology, Maryknoll Hospital, Busan, Korea. pjm1438@hanmail.net
- 2Kim's Eye Clinic, Cheongju, Korea.
- 3Department of Ophthalmology, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea.
Abstract
- PURPOSE
To evaluate the findings of carotid ultrasonography performed on patients with retinal vascular disease and to determine the risk of cardiovascular disease and association of retinal vascular disease and cardiovascular disease.
METHODS
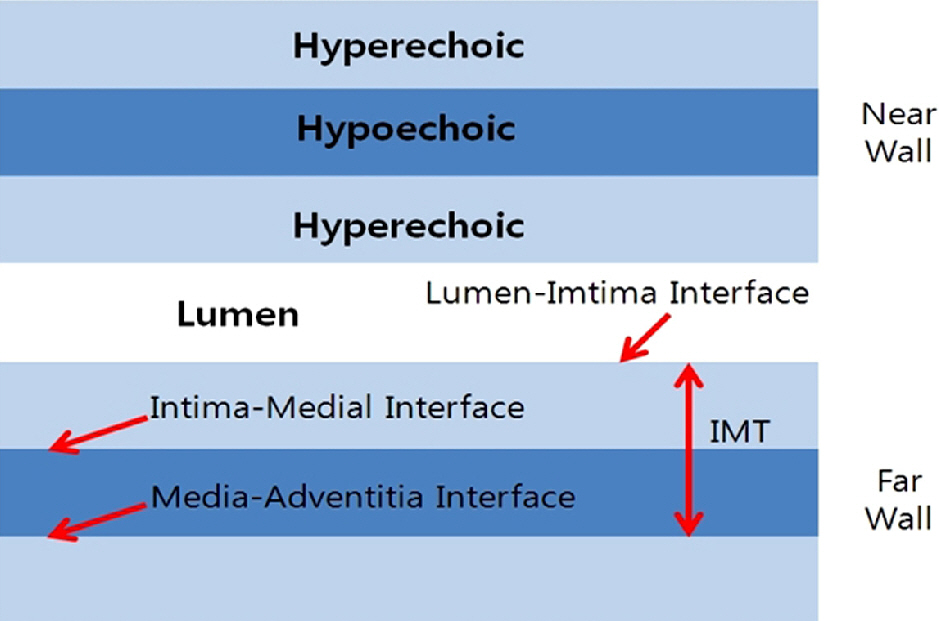
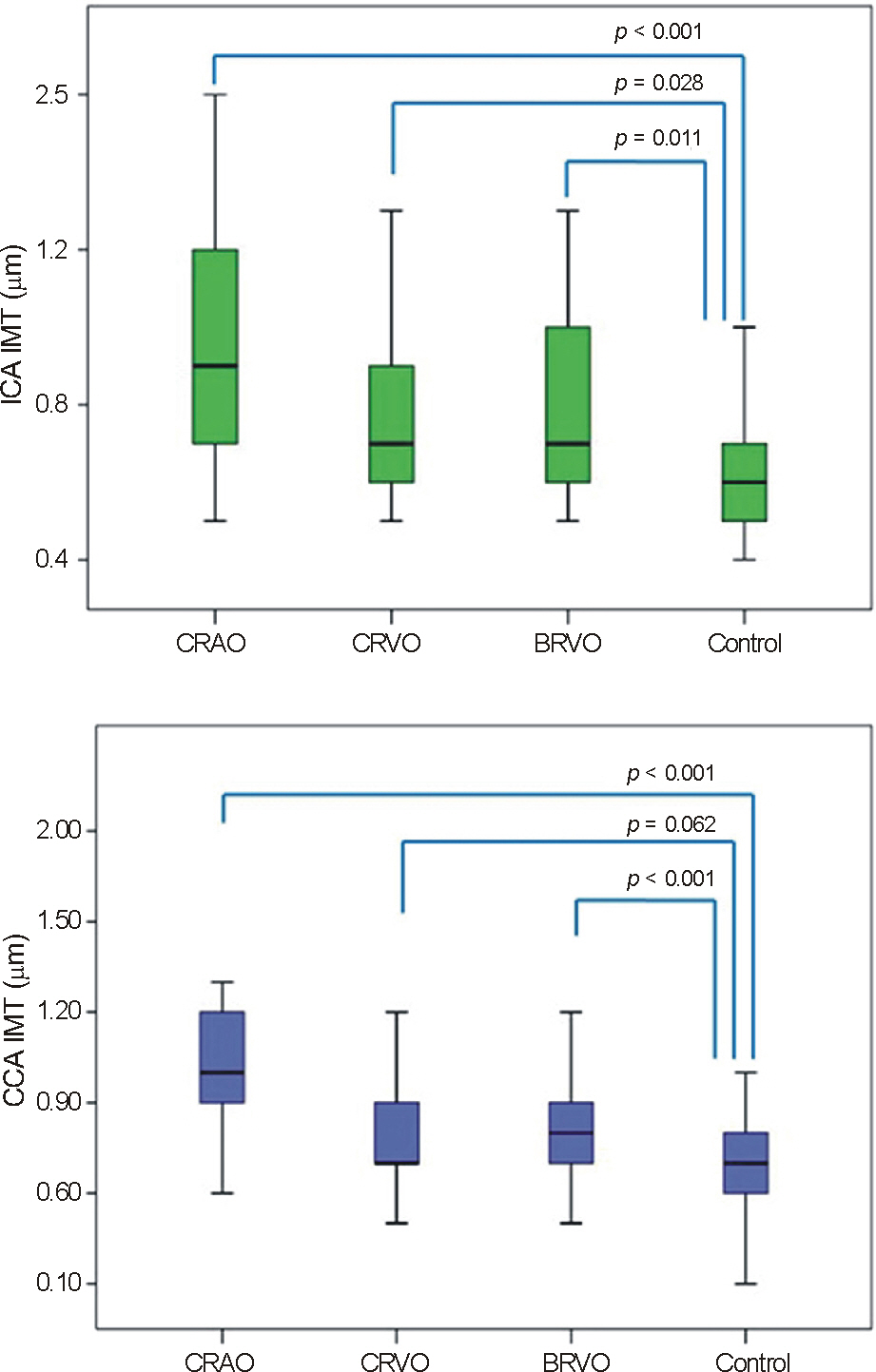
From December 2009 to May 2012, patients diagnosed with central retinal artery occlusion (CRAO, n = 18), central retinal vein occlusion (CRVO, n = 23), and branch retinal vein occlusion (BRVO, n = 68) underwent carotid ultrasonography. We evaluated the intima-media thickness (IMT) of the common carotid artery (CCA) and the internal carotid artery (ICA), stenosis and the number of plaques, and then compared these results with those of a healthy control group (n = 221).
RESULTS
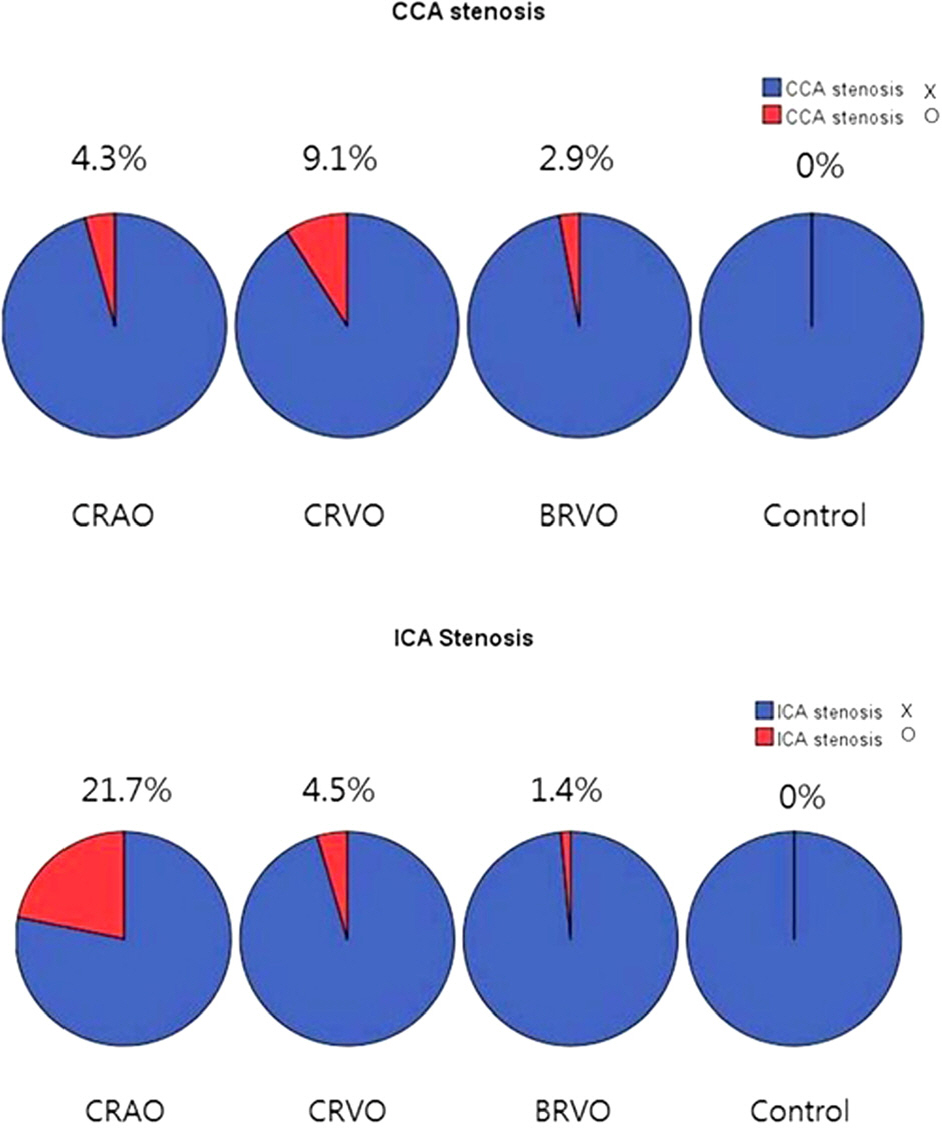
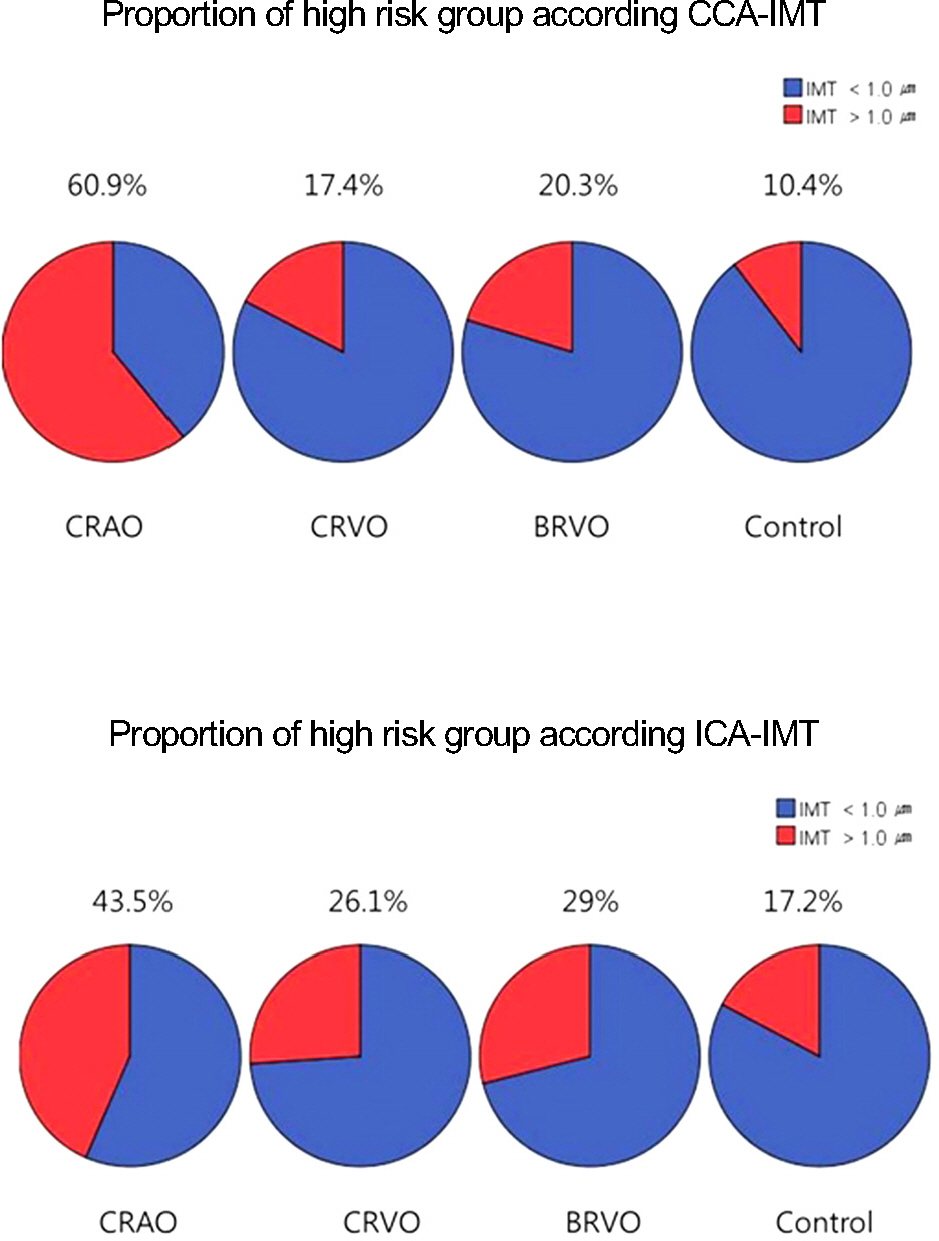
The mean CCA-IMT and ICA-IMT were significantly higher in the CRAO and BRVO groups compared with the control group. On the contralateral side, CCA-IMT was increased in the CRAO, BRVO, and CRVO groups and ICA-IMT was increased in the CRAO and BRVO groups compared with the control group. Contralateral CCA stenosis was higher in the CRVO group (9.1%) and ipsilateral ICA stenosis in CRAO group (21.7%) was significantly higher than that of the control group. Plaque was observed better in all groups compared with the control group. The proportion of patients risk for cardiovascular disease, i.e. those who had IMT thickenesses more than 1.0 mm, was higher in the CRAO and BRVO groups compared with the control group.
CONCLUSIONS
The carotid ultrasound findings of patients with retinal vascular diseases showed increased IMT and plaque. The group of patient at risk for cardiovascular disease, which was defined with carotid artery IMT, was higher in patients with retinal vascular disease. Therefore, in patients with retinal vascular disease, carotid artery ultrasonography and the overall management and treatment of cardiovascular disease are necessary.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Bullock JD, Falter RT, Downing JE, Snyder HE. Ischemic oph-thalmia secondary to an ophthalmic artery occlusion. Am J Ophthalmol. 1972; 74:486–93.2. Breslin DJ, Gifford RW Jr, Fairbairn JF 2nd, Kearns TP. Prognostic importance of ophthalmoscopic finding in essential hypertension. JAMA. 1966; 195:335–8.3. Feussner JR, Matchar DB. When and how to study the carotid arteries. Ann Intern Med. 1988; 109:805–18.
Article4. Smith SC Jr, Amsterdam E, Balady GJ, et al. Prevention Conference V: beyond secondary prevention: identifying the high-risk patient for primary prevention: tests for silent and inducible ischemia: Writing Group II. Circulation. 2000; 101:E12–6.5. Pearsn TA. New tools for coronary risk assessment: what are their advantages and limitations? Circulation. 2002; 105:886–92.6. Chambless LE, Folsom AR, Clegg LX, et al. Carotid wall thickness is predictive of incident clinical stroke: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Epidemiol. 2000; 151:478–87.
Article7. O’Leary DH, Polak JF, Kronmal RA, et al. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med. 1999; 340:14–22.
Article8. Nowak J, Nilsson T, Sylvén C. Potential of carotid ultrasonography in the diagnosis of coronary artery disease: a comparison with ex-ercise test and variance ECG. Stroke. 1998; 29:439–46.9. Suh DC, Lee SH, Kim KR, et al. Pattern of atherosclerotic carotid stenosis in Korean patients with stroke: different involvement of intracranial versus extracranial vessels. AJNR Am J Neuroradiol. 2003; 24:239–44.10. Cote R, Barnett HJ, Taylor DW. Internal carotid occlusion: a prospective study. Stroke. 1983; 14:898–902.
Article11. Peternel P, Keber D, Videcnik V. Carotid arteries in central retinal vessel occlusion as assessed by Doppler ultrasound. Br J Ophthal. 1989; 73:880–3.
Article12. Klien BA, Olwin JH. A survey of the pathogenesis of retinal venous occlusion, emphasis upon choice of therapy and an analysis of the therapeutic results in fifty-three patients. AMA Arch Ophthalmol. 1956; 56:207–47.13. Klien BA. Sidelights on retinal venous occlusion. Am J Ophthalmol. 1966; 61:25–36.
Article14. CASSADY JV. Central retinal vein thrombosis. Am J Ophthalmol. 1953; 36:331–5.
Article15. Hayreh SS. Classification of central retinal vein occlusion. Ophthalmology. 1983; 90:458–74.
Article16. Hayreh SS. Pathogenesis of occlusion of the central retinal vessels. Am J Ophthalmol. 1971; 72:998–1011.
Article17. Marin-Sanabria EA, Kondoh T, Yamanaka A, Kohmura E. Ultrasonographic screening of carotid artery in patients with vascular retinopathies. Kobe J Med Sci. 2005; 51:7–16.18. Matsushima C, Wakabayashi Y, Iwamoto T, et al. Relationship between retinal vein occlusion and carotid artery lesions. Retina. 2007; 27:1038–43.
Article19. Sayag D, Gotzamanis A, Brugniart C, et al. Retinal vein occlusion and carotid Doppler imaging. J Fr Ophthalmol. 2002; 25:826–30.20. Cheung N, Klein R, Wang JJ, et al. Traditional and novel cardiovascular risk factor for retinal vein occlusion: the multiethnic study of atherosclerosis. Invest Ophthalmol Vis Sci. 2008; 49:4297–302.21. Choi SY, Kim D, Kang JH, et al. Nonalcoholic fatty liver disease as a risk factor of cardiovascular disease: relation of non-alcoholic fatty liver disease to carotid atherosclerosis. Korean J Hepatol. 2008; 14:77–88.
Article22. Stojakovic T, Scharnagl H, März W, et al. Low density lipoprotein triglycerides and lipoprotein are risk factors for retninal vascular occlusion. Clin Chim Acta. 2007; 382:77–81.23. Su TC, Chien KL, Jeng JS, et al. Age-and gender-associated determinants of carotid intima-media thickness: a community-based study. J Atheroscler Thromb. 2012; 19:872–80.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Do we need individual measurement of carotid intima and media thickness?
- Association between Carotid Artery Intima-Media Thickness and Stroke Risk Factors in Ischemic Stroke
- Measurements of Carotid Intima, Media, and Intima-media Thickness and Their Clinical Importance
- The Relationship of Pulse-wave Velocity with Carotid Intima-media Thickness and Carotid Artery Distensibility
- Carotid Artery Intima-Media Thickness and Large-Artery Atherosclerotic Cerebral Infarction