J Korean Ophthalmol Soc.
2012 Oct;53(10):1425-1431.
Long Term Clinical Results of Penetrating Keratoplasty for Macular Corneal Dystrophy
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea. mskim@catholic.ac.kr
Abstract
- PURPOSE
To report the long term clinical results of penetrating keratoplasty as a treatment for corneal macular dystrophy.
METHODS
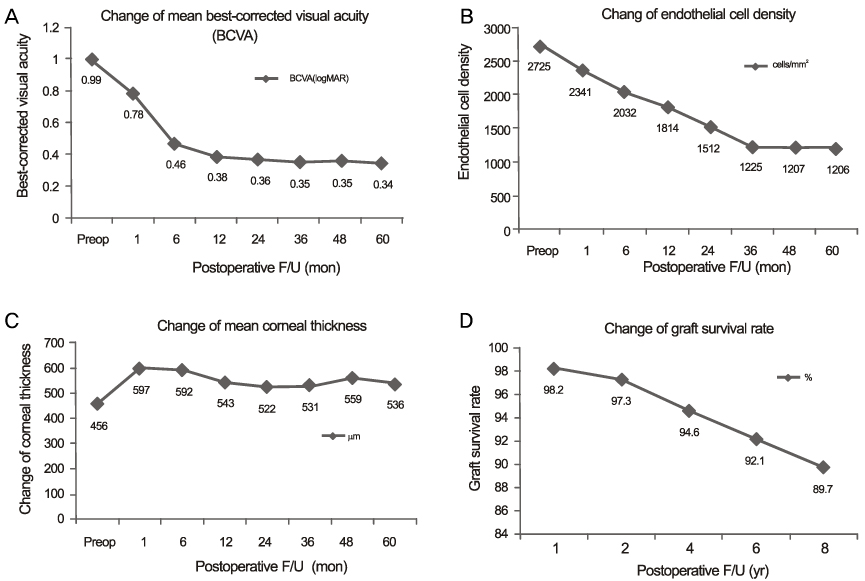
Retrospective review of the medical record of 46 eyes (31 indivisuals) who underwent primary PK for corneal macular dystrophy at the Seoul St. Mary's Hospital between November, 1986 and December, 2011. Data extracted preoperative and postoperative best-corrected visual acuity (BCVA), postoperative complications (including graft rejection episodes, and recurrent dystrophy), change of endothelial cell density at 1, 6, 12, 24, 36 months and yearly thereafter.
RESULTS
After a mean follow-up period of 91.59 +/- 3.2 months, the mean BCVA was significantly improved after penetrating keratoplasty. Endothelial cell loss rate was marked during the 1st year after penetrating keratoplasty. Graft survival was 40 graft (89.7%) at 8yrs. There was a statistically significant increased likelihood of graft failure if the patient was older than 40 years at the time of surgery (p = 0.03). Glaucoma as postoperative complication was 17.4%. Clinically significant recurrence was 2%.
CONCLUSIONS
Penetrating keratoplasty is associated with a good visual outcome and prognosis for graft survival of long-term efficacy with a low complication rate in eyes with macular corneal dystrophy.
MeSH Terms
Figure
Reference
-
1. Cogan DG, Donaldson DD, Kuwabara T, Marshall D. Microcystic Dystrophy of the Corneal Epithelium. Trans Am Ophthalmol Soc. 1964. 62:213–225.2. Waring GO 3rd, Rodrigues MM, Laibson PR. Corneal dystrophies. I. Dystrophies of the epithelium, Bowman's layer and stroma. Surv Ophthalmol. 1978. 23:71–122.3. Vemuganti GK, Rathi VM, Murthy SI. Histological landmarks in corneal dystrophy: pathology of corneal dystrophies. Dev Ophthalmol. 2011. 48:24–50.4. Weiss JS, Møller HU, Lisch W, et al. The IC3D classification of the corneal dystrophies. Cornea. 2008. 27:Suppl 2. S1–83.5. Møller HU, Weiss JS. IC3D classification of corneal dystrophies. Dev Ophthalmol. 2011. 48:1–8.6. Ghosh M, McCulloch C. Macular corneal dystrophy. Can J Ophthalmol. 1973. 8:515–526.7. Mrukwa-Kominek E, Rokita-Wala I, Gierek-Ciaciura S. [Macular corneal dystrophy--clinical state, histopathologic, immunohistochemical examinations and genetical dependence]. Klin Oczna. 2004. 106:802–805.8. Cursiefen C, Hofmann-Rummelt C, Schlötzer-Schrehardt U, et al. Immunohistochemical classification of primary and recurrent macular corneal dystrophy in Germany: subclassification of immunophenotype I A using a novel keratan sulfate antibody. Exp Eye Res. 2001. 73:593–600.9. Plaas AH, West LA, Thonar EJ, et al. Altered fine structures of corneal and skeletal keratan sulfate and chondroitin/dermatan sulfate in macular corneal dystrophy. J Biol Chem. 2001. 276:39788–39796.10. Klintworth GK, Meyer R, Dennis R, et al. Macular corneal dystrophy. Lack of keratan sulfate in serum and cornea. Ophthalmic Paediatr Genet. 1986. 7:139–143.11. Jonasson F, Johannsson JH, Garner A, Rice NS. Macular corneal dystrophy in Iceland. Eye (Lond). 1989. 3(Pt 4):446–454.12. Jonasson F, Oshima E, Thonar EJ, et al. Macular corneal dystrophy in Iceland. A clinical, genealogic, and immunohistochemical study of 28 patients. Ophthalmology. 1996. 103:1111–1117.13. Liu NP, Dew-Knight S, Rayner M, et al. Mutations in corneal carbohydrate sulfotransferase 6 gene (CHST6) cause macular corneal dystrophy in Iceland. Mol Vis. 2000. 6:261–264.14. Klintworth GK, Oshima E, al-Rajhi A, et al. Macular corneal dystrophy in Saudi Arabia: a study of 56 cases and recognition of a new immunophenotype. Am J Ophthalmol. 1997. 124:9–18.15. Choi SH, Lee YW, Kim HM, et al. Epidemiologic Studies of Keratoplasty in Korea. J Korean Ophthalmol Soc. 2006. 47:538–547.16. Patel AK, Nayak H, Kumar V. Comparative evaluation of big-bubble deep anterior lamellar keratoplasty and penetrating keratoplasty in a case of macular corneal dystrophy. Cornea. 2009. 28:583–585.17. Akova YA, Kirkness CM, McCartney AC, et al. Recurrent macular corneal dystrophy following penetrating keratoplasty. Eye (Lond). 1990. 4(Pt 5):698–705.18. Meyer HJ. [Prognosis of keratoplasty in hereditary stromal dystrophies]. Klin Monbl Augenheilkd. 1996. 208:446–449.19. Wagoner MD, Badr IA. Phototherapeutic keratectomy for macular corneal dystrophy. J Refract Surg. 1999. 15:481–484.20. Kawashima M, Kawakita T, Den S, et al. Comparison of deep lamellar keratoplasty and penetrating keratoplasty for lattice and macular corneal dystrophies. Am J Ophthalmol. 2006. 142:304–309.21. Klintworth GK, Reed J, Stainer GA, Binder PS. Recurrence of macular corneal dystrophy within grafts. Am J Ophthalmol. 1983. 95:60–72.22. Newsome DA, Hassell JR, Rodrigues MM, et al. Biochemical and histological analysis of "recurrent' macular corneal dystrophy. Arch Ophthalmol. 1982. 100:1125–1131.23. Al-Swailem SA, Al-Rajhi AA, Wagoner MD. Penetrating keratoplasty for macular corneal dystrophy. Ophthalmology. 2005. 112:220–224.24. Price FW Jr, Whitson WE, Johns S, Gonzales JS. Risk factors for corneal graft failure. J Refract Surg. 1996. 12:134–143. discussion 143-7.25. Kim TK, Byun YS, Kim MS. Analysis of factors affecting corneal endothelial cell loss after penetrating keratoplasty. J Korean Ophthalmol Soc. 2011. 52:807–815.26. Price FW Jr, Whitson WE, Marks RG. Graft survival in four common groups of patients undergoing penetrating keratoplasty. Ophthalmology. 1991. 98:322–328.27. Marcon AS, Cohen EJ, Rapuano CJ, Laibson PR. Recurrence of corneal stromal dystrophies after penetrating keratoplasty. Cornea. 2003. 22:19–21.28. Küchle M, Cursiefen C, Fischer DC, et al. Recurrent macular corneal dystrophy type II 49 years after penetrating keratoplasty. Arch Ophthalmol. 1999. 117:528–531.29. Lorenzetti DW, Kaufman HE. Macular and lattice dystrophies and their recurrences after keratoplasty. Trans Am Acad Ophthalmol Otolaryngol. 1967. 71:112–118.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long-Term Outcomes of Penetrating Keratoplasty in Treating Macular Corneal Dystrophy, TGFBI Dystrophy, and Fuchs' Dystrophy
- Clinical Evaluation of Full-thickness Deep Lamellar Keratoplasty
- Cataract Extraction after Penetrating Keratoplasty
- A Case of Corneal Transplantation for Type III Lattice Corneal Dystrophy with Aphakia
- A Case of Macular Dystrophy of the Cornea