J Korean Ophthalmol Soc.
2012 Jun;53(6):743-748.
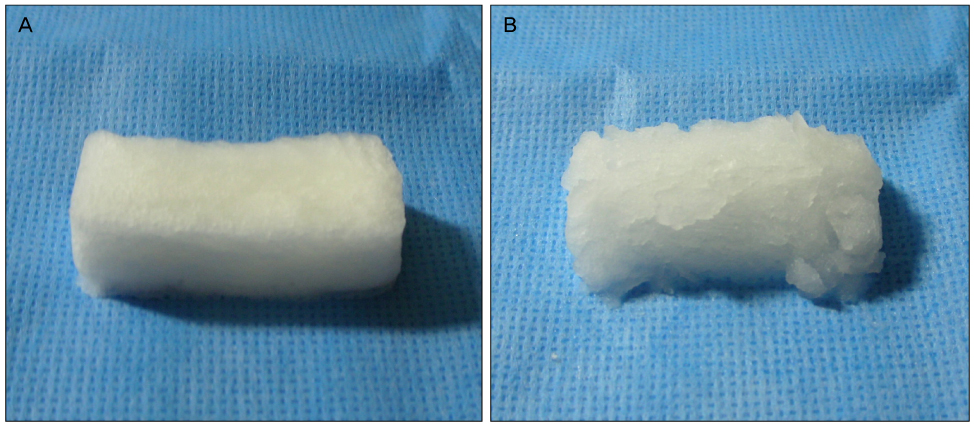
Clinical Application of Polyether Ester Urethane in Endonasal Dacryocystorhinostomy
- Affiliations
-
- 1Department of Ophthalmology, Maryknoll Medical Center, Busan, Korea. eyerheu@hanafos.com
Abstract
- PURPOSE
To evaluate the clinical effect of intraoperative application of polyether ester urethane (Nasopore(R)) in endonasal dacryocystorhinostomy.
METHODS
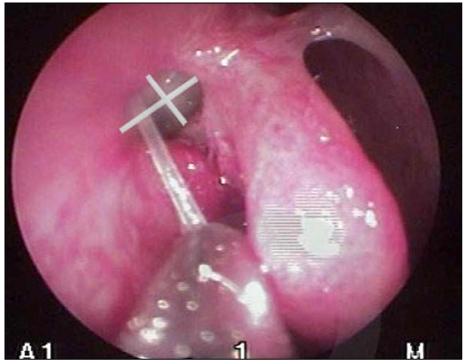
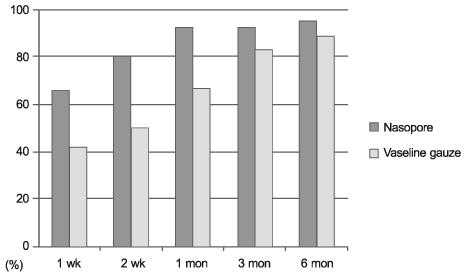
Endonasal dacryocystorhinostomy was performed on 77 eyes diagnosed with nasolacrimal duct obstruction between January 2010 and February 2011. Nasopore(R) was applied to the newly-formed internal lacrimal opening in the experimental group (41 eyes), and vaseline gauze was applied in the control group (36 eyes). For the evaluation of clinical effects regarding postoperative adhesion and stenosis of the internal lacrimal opening, subjective symptom improvement, lacrimal irrigation tests, and endoscopic examinations were performed at 1 week, 2 weeks, 1 month, 3 months, and 6 months, postoperatively.
RESULTS
In subjective symptom improvement and lacrimal irrigation tests, differences between the 2 groups were not statistically significant. In endoscopic findings, the Nasopore(R) group showed significantly lower severity of adhesion and stenosis of the internal lacrimal opening at 1 week, 2 weeks, and 1 month after operation (p < 0.05).
CONCLUSIONS
Application of the Nasopore(R) may effectively reduce initial postoperative adhesion or stenosis of the internal lacrimal opening after endonasal dacryocystorhinostomy and has usefulness as an auxiliary method.
MeSH Terms
Figure
Reference
-
1. McDonogh M, Meiring JH. Endoscopic transnasal dacryocystorhinostomy. J Laryngol Otol. 1989. 103:585–587.2. Park JW, Park HY, Yoon KC. Clinical effect of the mixed solution of sodium hyaluronate and sodium carboxymethylcellulose after endonasal dacryocystorhinostomy. J Korean Ophthalmol Soc. 2010. 51:795–801.3. Boush GA, Lemke BN, Dortzbach RK. Results of endonasal laser-assisted dacryocystorhinosotmy. Ophthalmology. 1994. 101:955–959.4. Woog JJ, Metson R, Puliafito CA. Holmium: YAG endonasal laser dacryocystorhionostomy. Am J Ophthalmol. 1993. 116:1–10.5. Choi YJ, Hwang SJ, Lee TS. Short-term clinical results of amniotic membrane application to endonasal dacryocystorhinostomy. J Korean Ophthalmol Soc. 2008. 49:384–389.6. Kim JH, Shin JC. Clinical evaluation of endoscopic transnasal dacryocyocystorhinostomy. J Korean Ophthalmol Soc. 1997. 38:1706–1711.7. Metson R. Endoscopic surgery for lacrimal obstruction. Otolaryngol Head Neck Surg. 1991. 104:473–479.8. Goldberg RA. Endonasal dacryocystorhinostomy: is it really less successful? Arch Ophthalmol. 2004. 122:108–110.9. Mannor GE, Millman AL. The prognostic value of preoperative dacryocystography in endoscopic intranasal dacryocystorhinostomy. Am J Ophthalmol. 1992. 113:134–137.10. Leong M, Phillips LG. Townsend CM, editor. Wound healing. Sabiston Textbook of Surgery. 2004. 17th ed. Philadelphia: WB Saunders;chap. 18.11. Roozitalab MH, Amirahmadi M, Namazi MR. Results of the application of intraoperative mitomycin C in dacryocystorhinostomy. Eur J Ophthalmol. 2004. 14:461–463.12. Oh TH, Paik JS, Yang SW. Results of the mixed solution of hyaluronate and sodium carboxymethylcellulose in endonasal dacryocystorhinostomy. J Korean Ophthalmol Soc. 2010. 51:159–163.13. Lee TS, Kim SW, Park BW. The relationship between rate of wound healing and success rate after endonasal laser-drill assisted dacryocystorhinostomy. J Korean Ophthalmol Soc. 1999. 40:2969–2974.14. Field FK, Kerstein MD. Overview of wound healing in a moist environment. Am J Surg. 1994. 167:2S–6S.15. Dogru S, Haholu A, Gungor A, et al. Histologic analysis of the effects of three different support materials within rat middle ear. Otolaryngol Head Neck Surg. 2009. 140:177–182.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Mitomycin C in Endonasal Dacryocystorhinostomy
- Clinical Outcomes of Endonasal Dacryocystorhinostomy with Canalicular Trephination in Canalicular Obstruction
- Clinical Effecd of Endonasal Lacrimal Surgery
- Clinical Effect of the Mixed Solution of Sodium Hyaluronate and Sodium Carboxymethylcellulose After Endonasal Dacryocystorhinostomy
- Success Rate of Endonasal Dacryocystorhinostomy Based on the Location of the Lacrimal Sac