J Korean Ophthalmol Soc.
2012 Feb;53(2):348-352.
A Case of Juvenile Xanthogranuloma in the Lacrimal Sac
- Affiliations
-
- 1Department of Ophthalmology, Wonkwang University College of Medicine, Iksan, Korea. sangduck@wonkwang.ac.kr
Abstract
- PURPOSE
To report a rare case of juvenile xanthogranuloma in the lacrimal sac.
CASE SUMMARY
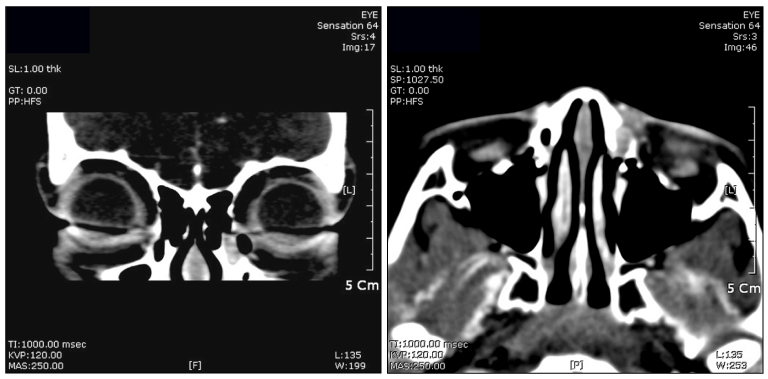
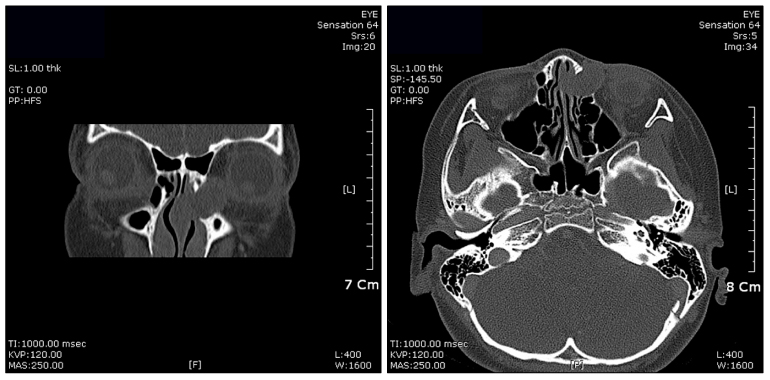
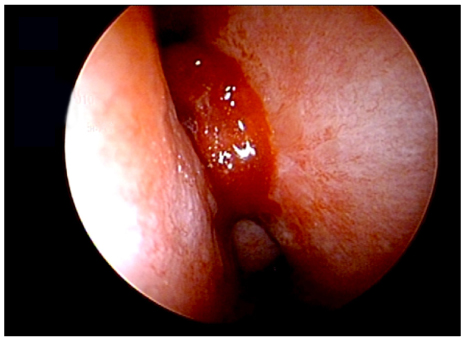
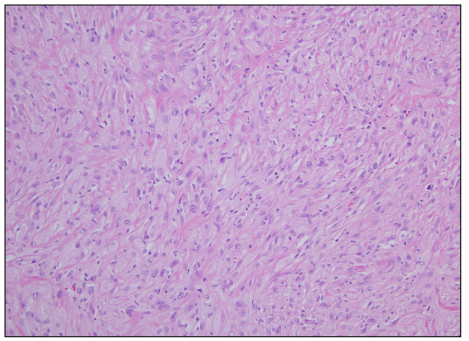
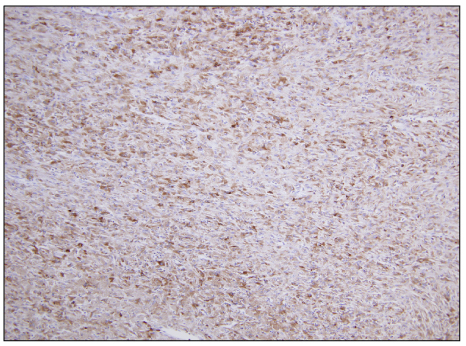
An 8-year-old female presented to our hospital with epiphora and palpable mass on the left medial canthal area. As a symptom, a sticky and bloody discharge through the punctum had begun on occasion 3 months previously. When pressure was applied on the left medial canthal area, a mucoid discharge through the punctum occurred, and a solid mass was palpable. The mass localized in the lacrimal sac and upper nasolacrimal duct was observed on orbit CT. No invasion into the surrounding tissue was present. The authors of the present study decided to perform endonasal dacryocystorhinostomy, and subsequently a skin-colored mass was found in the lacrimal sac. The histopathological and immunohistochemical diagnosis was histiocytic proliferation, compatible with juvenile xanthogranuloma. Six months later, the patient complained of epiphora recurrence with palpable mass on medial canthal area. The tumor recurrence was confirmed with enhanced orbit CT finding 14 months after the first surgery. A second surgery using endonasal dacryocystorhinostomy was performed to remove the mass.
MeSH Terms
Figure
Reference
-
1. Weiss SW, Goldblum JR. Enzinger and Weiss's Soft Tissue Tumors. 2008. 5th ed. Philadelphia, PA: Mosby Elsevier;331–358.2. Flaitz C, Allen C, Neville B, et al. Juvenile xanthogranuloma of oral cavity in children: a clinicopathologic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002. 94:345–352.3. Helwig EB, Hackney V. Juvenile xanthogranuloma (nevoxanthoendothelioma). Am J Pathol. 1954. 30:625–626.4. Janssen D, Harms D. Juvenile xanthogranuloma in childhood and adolescence: a clinicopathologic study of 129 patients from the kiel pediatric tumor registry. Am J Surg Pathol. 2005. 29:21.5. Redbord KP, Sheth AP. Multiple juvenile xanthogranulomas in a 13-year-old. Pediatr Dermatol. 2007. 24:238–240.6. Senear FE, Caro MR. Nevoxanthoendothelioma or juvenile xathoma. Arch Dermatol. 1936. 34:195–206.7. Mruthyunjaya P, Meyer DR. Juvenile xanthogranuloma of the lacrimal sac fossa. Am J Ophthalmol. 1997. 123:400–402.8. Adamson HG. Society intelligence: the dermatological society of London. Br J Dermatol. 1905. 17:222.9. Gartman H, Tritsch H. Hein-und grossknotiges Naevoxanthoendotheliem. Arch Klin Exp Dermatol. 1963. 215:409–421.10. Cohen BA, Hood A. Xanthogranuloma: report on clinical and histological finding in 64 patients. Pediatr Dermatol. 1989. 6:262–266.11. Tahan SR, Pastel-Levy C, Bhan AK, Mihm MC Jr. Juvenile xanthogranuloma. Clinical and pathologic characterization. Arch Pathol Lab Med. 1989. 113:1057–1061.12. Sangueza OP, Salmon JK, White CR Jr, Beckstead JH. Juvenile xanthogranuloma: a clinical, histopathologic and immunocytochemical study. J Cutan Pathol. 1995. 22:327–335.13. Chu AC, D'Angio G, Favara D. Histiocytosis syndrome in children. Lancet. 1978. 1:208–209.14. Vasconcelos FO, Oliveira LA, Naves MD, et al. Juvenile xanthogranuloma: case report with inmmunohistochemical indentification of early and late cytomegalovirus antigens. J Oral Sci. 2001. 43:21–25.15. Scappaticci S, Danesino C, Rossi E, et al. AIEOP-lstiocitosi Group. Cytogetic abnormality in PHA-stimulated lymphoxytes from patients with Langerhans cell histocytosis. Br J Haematol. 2000. 111:258–262.16. Zelger B, Cerio R, Orchard G, Wilson-Jones E. Juvenile and adult xanthogranuloma A histological and immunohistological comparison. Am J Surg Pathol. 1994. 18:126–135.17. Nascimento AG. A clinicopathologic and immunohistochemical comparative study of cutaneous and intramuscular forms of juvenile xanthogranuloma. Am J Surg Pathol. 1997. 21:645–652.18. Dehner LP. Juvenile xanthogranuloma in the first two decades of life: a clinicopathologic study of 174 cases with cutaneous and extracutaneous manifestations. Am J Surg Pathol. 2003. 27:579–593.19. Hernandez-Martin A, Baselga E, Drolet BA, Esterly NB. Juvenile xanthogranuloma. J Am Acad Dermatol. 1997. 36:355–367.20. Tanz WS, Schwartz RA, Janniger CK. Juvenile xanthogranuloma. Cutis. 1994. 54:241–245.