J Korean Ophthalmol Soc.
2011 Nov;52(11):1351-1356.
A Case of Paranasal Diffuse Large B-Cell Lymphoma with the Orbital Invasion Masquerading as Chronic Sinusitis
- Affiliations
-
- 1Department of Opthalmology, The institute of Vision Research, Yonsei University College of Medicine, Seoul, Korea.
- 2Department of Radiology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Opthalmology, Bundang CHA Medical Center, CHA University, Seongnam, Korea. eye@cha.ac.kr
Abstract
- PURPOSE
To report a case of paranasal diffuse large B-cell lymphoma with orbital invasion extending to the intracranial lesion.
CASE SUMMARY
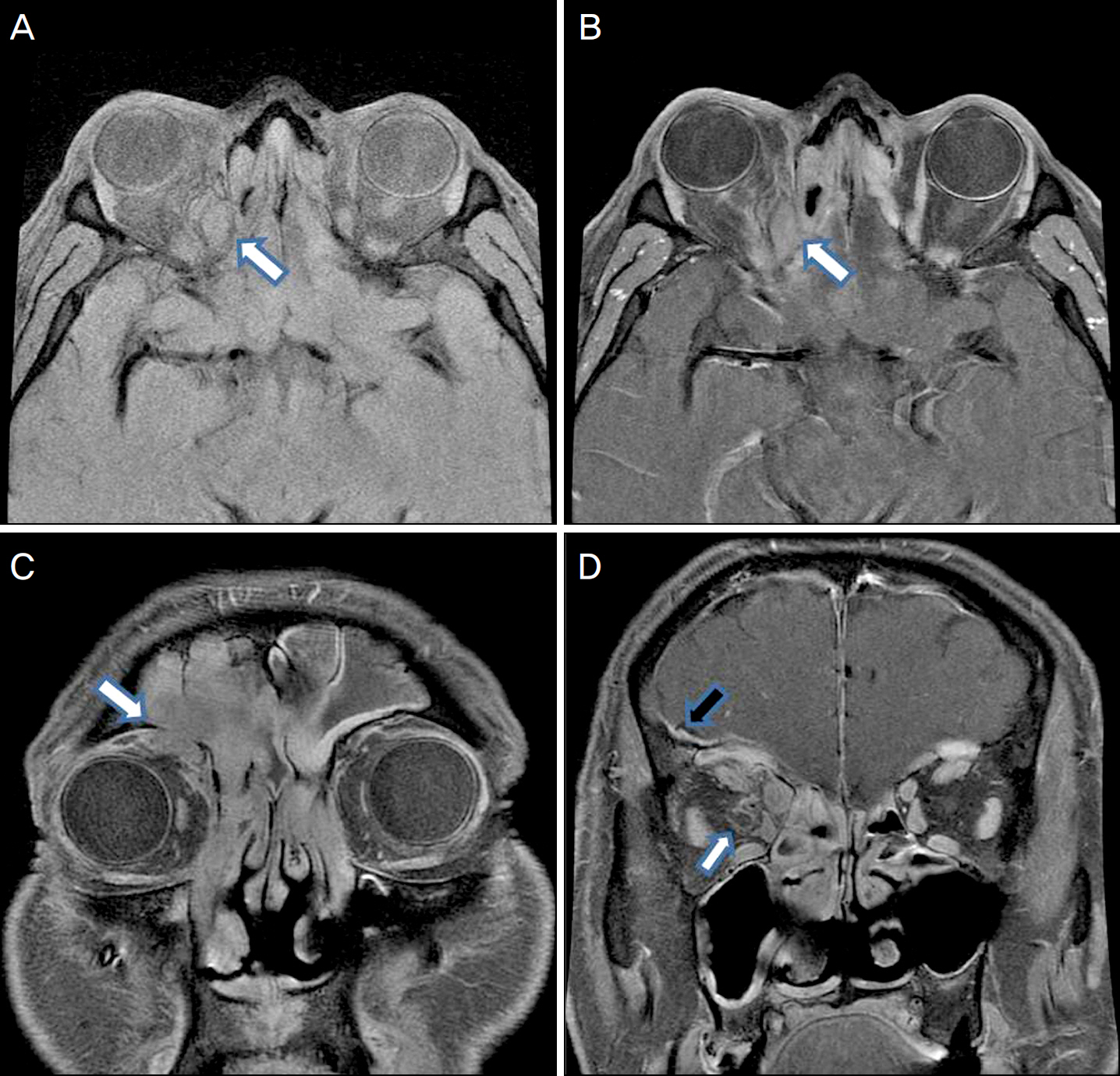
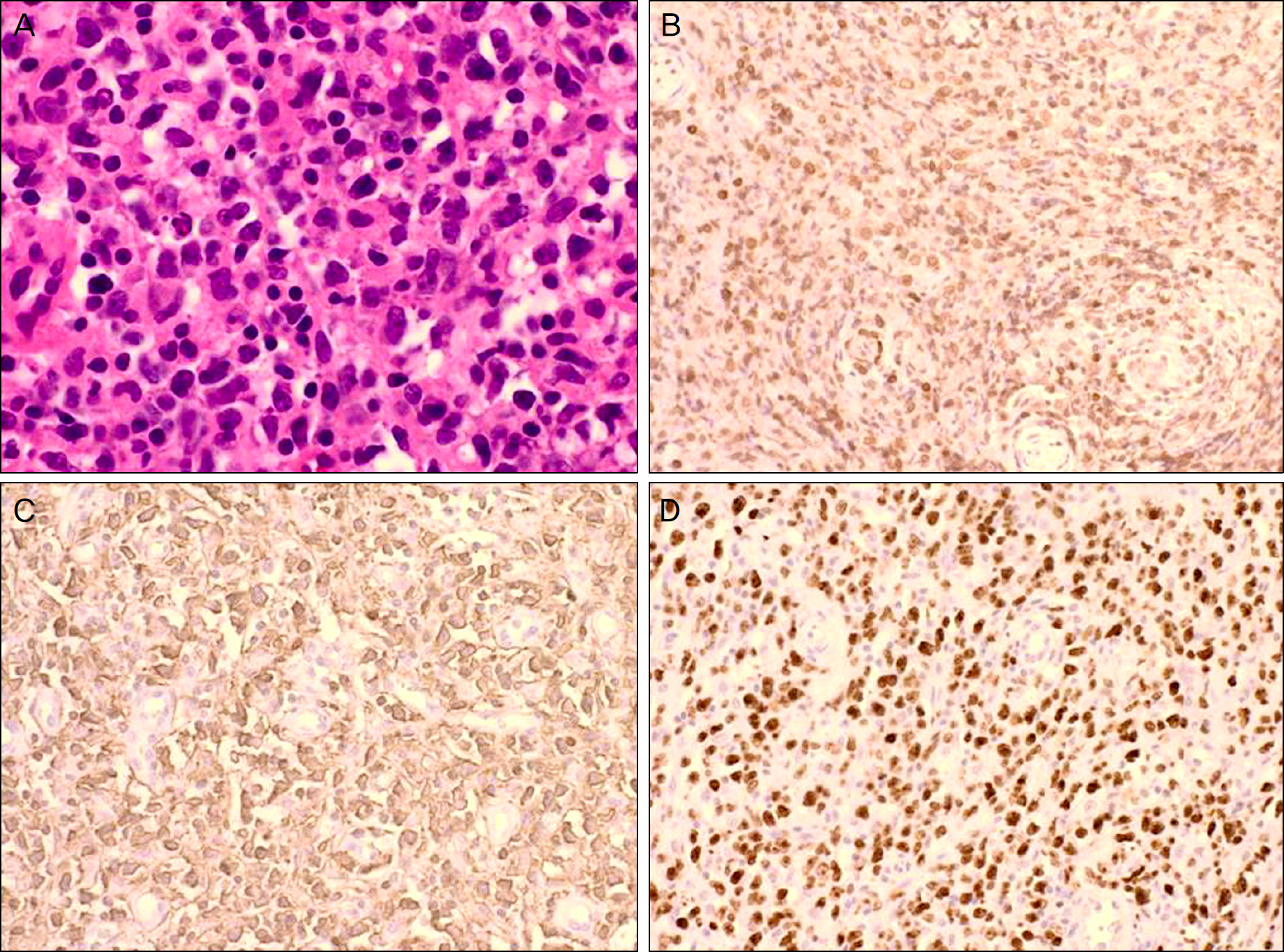
A 48-year-old male with chronic sinusitis visited our clinic for recent proptosis of his right eye, intermittent pain around the eyeball and headache. On a magnetic resonance image (MRI), a mass-like lesion was observed in the right frontal sinus, and its infiltration into the superior inner portion of the right orbital extraconal space and right intracranial dural space was suggestive of generalized inflammatory mucosal thickening in the paranasal sinuses. An incisional biopsy of the sinonasal tract was immediately performed. The pathology confirmed diffuse large B-cell lymphoma.
CONCLUSIONS
A mass involving the paranasal sinus and orbit can masquerade as chronic sinusitis. Because diffuse large B-cell lymphoma is rare and is a high-grade aggressive malignant lymphoma, the possibility for diagnosis must be considered.
MeSH Terms
Figure
Reference
-
References
1. Boring CC, Squires TS, Tong T. Cancer statistics. CA Cancer J Clin. 1993; 43:7–26.2. Aozasa K, Tsujimoto M, Sakurai M, et al. Non-Hodgkin's lymphomas in Osaka, Japan. Eur J Cancer Clin Oncol. 1985; 21:487–92.
Article3. Quraishi MS, Bessell EM, Clark D, et al. Non-Hodgkin's lymphoma of the sinonasal tract. Laryngoscope. 2000; 110:1489–92.
Article4. Neves MC, Lessa MM, Voegels RL, Butugan O. Primary non-Hodgkin's lymphoma of the frontal sinus: case report and review of the literature. Ear Nose Throat J. 2005; 84:47–51.
Article5. Shohat I, Berkowicz M, Dori S, et al. Primary non-Hodgkin's lymphoma of the sinonasal tract. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004; 97:328–31.
Article6. Chain JR, Kingdom TT. Non-Hodgkin's lymphoma of the frontal sinus presenting as osteomyelitis. Am J Otolaryngol. 2007; 28:42–5.7. Som PM, Shapiro MD, Biller HF, et al. Sinonasal tumors and inflammatory tissues: differentiation with MR imaging. Radiology. 1988; 167:803–8.8. Han MH, Chang KH, Kim IO, et al. Non-Hodgkin lymphoma of the central skull base: MR manifestations. J Comput Assist Tomogr. 1993; 17:567–71.9. Dare AO, Datta RV, Loree TR, et al. Sinonasal Non-Hodgkin's lymphoma with skull base involvement. Skull Base. 2001; 11:129–35.
Article10. Baik SH, Yeom DJ, Kang YK, et al. Orbital apex syndrome with nasal type Natural Killer(NK)/T-cell lymphoma of sphenoid and ethmoid sinus. J Korean Ophthalmol Soc. 2010; 51:286–91.
Article11. Choi KH, Lee SJ, Suh YL, Kim YD. Nasal-type natural kill-er/T-cell lymphoma of the orbit. J Korean Ophthalmol Soc. 2004; 45:2145–50.12. Ko YH, Kim CW, Park CS, et al. REAL classification of malignant lymphomas in the republic of korea: incidence of recently recognized entities and changes in clinicopathologic features. Hematolymphoreticular Study Group of the Korean Society of Pathologists. Revised European-American lymphoma. Cancer. 1998; 83:806–12.13. Rudders RA, Ross ME, DeLellis RA. Primary extranodal lymphoma: response to treatment and factors influencing prognosis. Cancer. 1978; 42:406–16.14. Greiner TC, Medeiros LJ, Jaffe ES. Non-Hodgkin's lymphoma. Cancer. 1995; 75:370–80.
Article15. Vidal RW, Devaney K, Ferlito A, et al. Sinonasal malignant lymphomas: a distinct clinicopathological category. Ann Otol Rhinol Laryngol. 1999; 108:411–9.
Article16. Oprea C, Cainap C, Azoulay R, et al. Primary diffuse large B-cell non-Hodgkin lymphoma of the paranasal sinuses: a report of 14 cases. Br J Haematol. 2005; 131:468–71.
Article17. Logsdon MD, Ha CS, Kavadi VS, et al. Lymphoma of the nasal cavity and paranasal sinuses: improved outcome and altered prognostic factors with combined modality therapy. Cancer. 1997; 80:477–88.18. Hausdorff J, Davis E, Long G, et al. Non-Hodgkin's lymphoma of the paranasal sinuses: clinical and pathological features, and response to combined-modality therapy. Cancer J Sci Am. 1997; 3:303–11.19. Oh DE, Kim YD. Lymphoproliferative diseases of the ocular adnexa in Korea. Arch Ophthalmol. 2007; 125:1668–73.
Article20. Kang IB, Tae K, Lee YJ. Ocular manifestations of paranasal sinus malignancies. J Korean Ophthalmol soc. 2009; 50:1455–60.
Article21. Giannoni CM, Stewart MG, Alford EL. Intracranial complications of sinusitis. Laryngoscope. 1997; 107:863–7.
Article22. Weber AL, Rahemtullah A, Ferry JA. Hodgkin and non-Hodgkin lymphoma of the head and neck: clinical, pathologic, and imaging evaluation. Neuroimaging Clin N Am. 2003; 13:371–92.23. Friedberg JW, Fisher RI. Diffuse large B-cell NHL. Cancer Treat. 2006; 131:121–40.
Article24. Smithers DW. Summary of papers delivered at the conference on staging in Hodgkin's Disease (Ann Arbor). Cancer Res. 1971; 31:1869–70.25. Shima N, Kobashi Y, Tsutsui K, et al. Exranodal non-Hodgkin's lymphoma of the head and neck. A clinicopathologic study in the Kyoto-Nara area in Japan. Cancer. 1990; 66:1190–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relapse of Ocular Lymphoma following Primary Testicular Diffuse Large B-cell Lymphoma
- A Case of Orbital Apex Syndrome Caused by Paranasal Sinusitis
- A Case of Isolated Frontal Fungal Sinusitis with Orbital Complication
- A Case of Peripheral T-Cell Lymphoma Mixed With Invasive Fungal Sinusitis of Maxillary Sinus
- A Case of Septic Cavernous Sinus Thrombosis Complicated by Sepsis