J Korean Ophthalmol Soc.
2010 Mar;51(3):440-446.
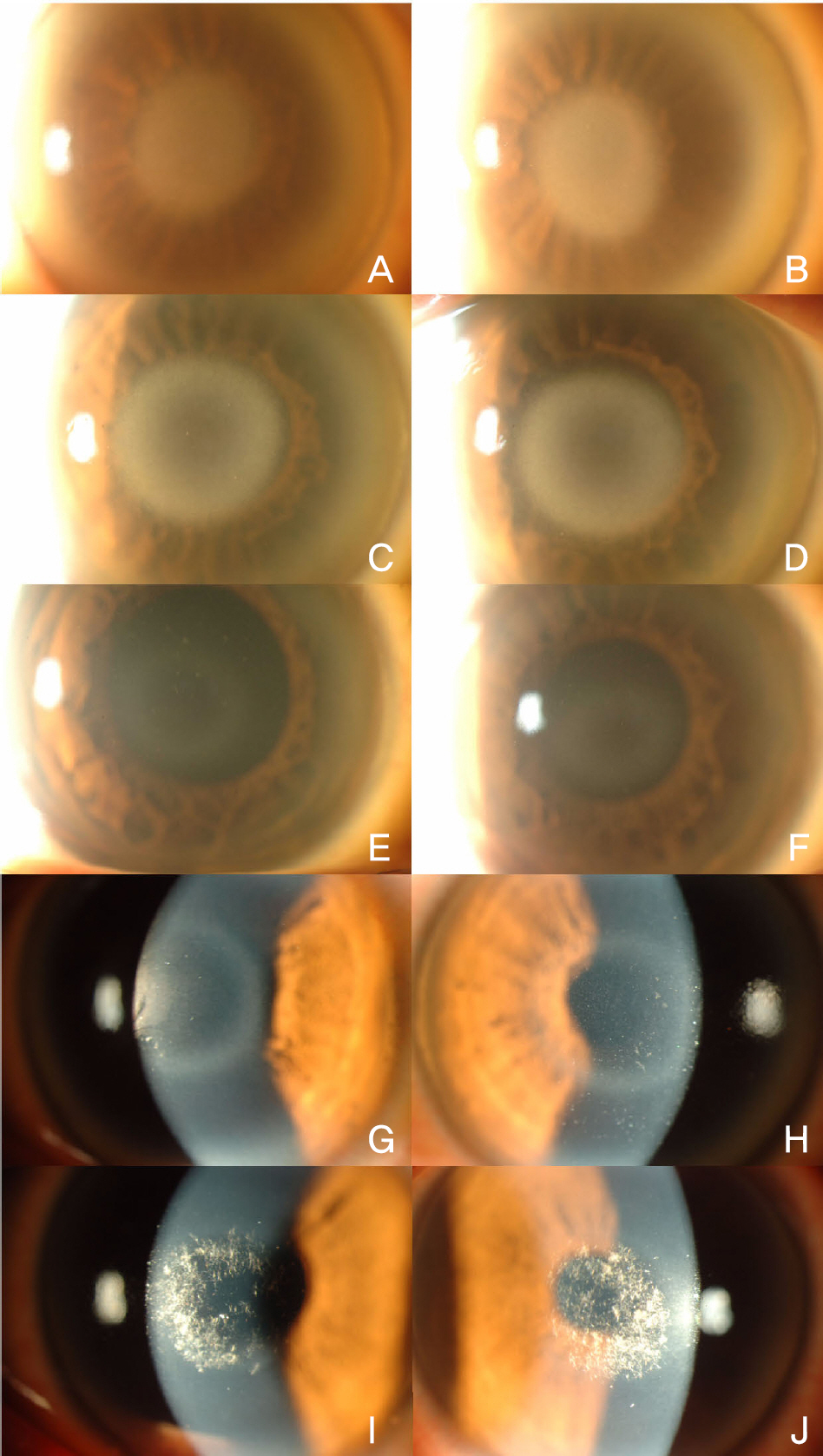
N102S Mutation of UBIAD1 Gene in a Family with Schnyder Crystalline Corneal Dystrophy
- Affiliations
-
- 1Corneal Dystrophy Research Institute, Department of Ophthalmology, Yonsei University College of Medicine, Seoul, Korea. eungkkim@yuhs.ac
Abstract
- PURPOSE
Schnyder crystalline corneal dystrophy (SCCD) is an autosomal dominant disease characterized by progressive central corneal opacification and premature development of peripheral arcus in the cornea. This disease results from a point mutation of UBIAD1 in chromosome 1p34-36. Until now, 15 different mutations of UBIAD1 gene on chromosome 1p34-36 have been reported for Schnyder crystalline corneal dystrophy. More point mutations are expected to be added to the list in the future. Schnyder crystalline corneal dystrophy is a rare disease, with only three reported cases in Korea, although there has been no report of a genetically confirmed case of the disease.
CASE SUMMARY
We encountered six patients with an N102S mutation of UBIAD1, who are from a family of two generation with 12 family members. Genetic confirmation for Schnyder crystalline corneal dystrophy was performed on these patients. This was the first report of a genetic confirmation of Schnyder crystalline corneal dystrophy in Korea. We will discuss our cases along with a review of the related literature.
MeSH Terms
Figure
Reference
-
References
1. Weiss JS. Visual morbidity in thirty-four families with Schnyder crystalline corneal dystrophy (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2007; 105:616–48.2. Shearman AM, Hudson TJ, Andresen JM, et al. The gene for schnyder's crystalline corneal dystrophy maps to human abdominal 1p34.1-p36. Hum Mol Genet. 1996; 5:1667–72.3. Aldave AJ, Rayner SA, Principe AH, et al. Analysis of fifteen abdominal candidate genes for Schnyder crystalline corneal dystrophy. Mol Vis. 2005; 11:713–6.4. Riebeling P, Polz S, Tost F, et al. Schnyder's crystalline corneal dystrophy. Further narrowing of the linkage interval at abdominal 1p34.1-p36? Ophthalmologe. 2003; 100:979–83.5. Theendakara V, Tromp G, Kuivaniemi H, et al. Fine mapping of the Schnyder's crystalline corneal dystrophy locus. Hum Genet. 2004; 114:594–600.
Article6. Weiss JS, Kruth HS, Kuivaniemi H, et al. Mutations in the UBIAD1 gene on chromosome short arm 1, region 36, cause Schnyder crystalline corneal dystrophy. Invest Ophthalmol Vis Sci. 2007; 48:5007–12.7. Kim HB, Kong YT, Hong YJ. Two Cases of Hereditary Crystaline Corneal Dystrophy of Schnyder. J Korean Ophthalmol Soc. 1973; 14:387–91.8. Kim JH, Myong YW. Histopathological Findings of Schnyder's Crystalline Corneal Dystrophy. J Korean Ophthalmol Soc. 1995; 36:1363–9.9. Jung SC, Myong YW. A Case of Spontaneous Regression of Schnyder's Crystalline Corneal Dystrophy. J Korean Ophthalmol Soc. 2000; 41:1441–4.10. Orr A, Dube MP, Marcadier J, et al. Mutations in the UBIAD1 gene, encoding a potential prenyltransferase, are causal for Schnyder crystalline corneal dystrophy. PLoS One. 2007; 2:e685.
Article11. Kobayashi A, Fujiki K, Murakami A, Sugiyama K. In vivo laser confocal microscopy findings and mutational analysis for Schnyder's crystalline corneal dystrophy. Ophthalmology. 2009; 116:1029–37.
Article12. Weiss JS, Kruth HS, Kuivaniemi H, et al. Genetic analysis of 14 families with Schnyder crystalline corneal dystrophy reveals clues to UBIAD1 protein function. Am J Med Genet A. 2008; 146:271–83.
Article13. Jing Y, Liu C, Xu J, Wang L. A novel UBIAD1 mutation abdominal in a Chinese family with Schnyder crystalline corneal dystrophy. Mol Vis. 2009; 15:1463–9.14. Weiss JS. Schnyder crystalline dystrophy sine crystals. Recommendation for a revision of nomenclature. Ophthalmology. 1996; 103:465–73.15. van Went JM WF. En zeldzame erfelijke hoornvliessandoening. Niederl Tijdschr Geneesks. 1924; 68:2996–7.16. WF S. Mitteilung über einen neuen Typus von familiärer Hornhauterkrankung. Schweiz Med Wochenschr. 1929; 10:559–71.17. Vesaluoma MH, Linna TU, Sankila EM, et al. In vivo confocal abdominal of a family with Schnyder crystalline corneal dystrophy. Ophthalmology. 1999; 106:944–51.18. Weller RO, Rodger FC. Crystalline stromal dystrophy: histochemistry and ultrastructure of the cornea. Br J Ophthalmol. 1980; 64:46–52.
Article19. Delleman JW, Winkelman JE. Degeneratio corneae cristallinea hereditaria. A clinical, genetical and histological study. Ophthalmologica. 1968; 155:409–26.20. Herring JH, Phillips D, McCaa CS. Phototherapeutic abdominal for Schnyder's central crystalline dystrophy. J Refract Surg. 1999; 15:4891989; 8:135–40.21. Bron AJ. Corneal changes in the dislipoproteinaemias. Cornea. 1989; 8:135–40.
Article22. Brownstein S, Jackson WB, Onerheim RM. Schnyder's abdominal corneal dystrophy in association with hyperlipoproteinemia: histopathological and ultrastructural findings. Can J Ophthalmol. 1991; 26:273–9.23. Lisch W, Weidle EG, Lisch C, et al. Schnyder's dystrophy. Progression and metabolism. Ophthalmic Paediatr Genet. 1986; 7:45–56.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Spontaneous Regression of Schnyder's Crystalline Corneal Dystrophy
- Histopathological Findings of Schnyder's Crystalline Corneal Dystrophy
- Two Cases of Hereditary Crystalline Corneal Dystrophy of Schnyder
- A case of Excimer Laser PRK in Schnyder's Dystrophy
- Cases of Macular Corneal Dystrophy with a Family History