J Korean Rheum Assoc.
2010 Sep;17(3):278-282.
A Case of Atypical Giant Cell Arteritis Presenting as Raynaud's Phenomenon and Diagnosed by Random Temporal Artery Biopsy
- Affiliations
-
- 1Department of Internal Medicine, Gyeongsang National University School of Medicine, Jinju, Korea. goldgu@gnu.ac.kr
- 2Institute of Health Sciences, Gyeongsang National University School of Medicine, Jinju, Korea.
- 3Department of Internal Medicine, Yeungnam University Hospital, College of Medicine, Yeungnam University, Daegu, Korea.
Abstract
- Giant cell arteritis (GCA) is a chronic vasculitis that mainly involves the cranial branches of arteries, and typically it presents with a cephalic sign such as a new headache, jaw claudication and/or visual symptoms. Although the tender, swollen or beaded arteries are adequate sites for biopsy, random temporal artery biopsy should be performed in all the patients suspected of suffering with GCA and even if cephalic signs are not present. Several cases of typical GCA have been reported in Korea, but so far there have been no reports of an atypical case presenting with Raynaud's phenomenon, and the patient was diagnosed by random temporal artery biopsy. Here we describe a case that showed the typical pathological findings of GCA in an asymptomatic temporal artery. The patient complained of only Raynaud's phnomenon and the patient was without any cephalic symptoms.
MeSH Terms
Figure
Reference
-
1). Nordborg E., Nordborg C. Giant cell arteritis: strategied in diagnosis and treatment. Curr Opin Rheumatol. 2004. 16:25–30.2). Hamidou MA., Batard E., Trewick D., Masseau A., Moreau A., Agard C, et al. Silent versus cranial giant cell arteritis. Initial presentation and outcome of 50 biopsy-proven cases. Eur J Intern Med. 2005. 16:183–6.
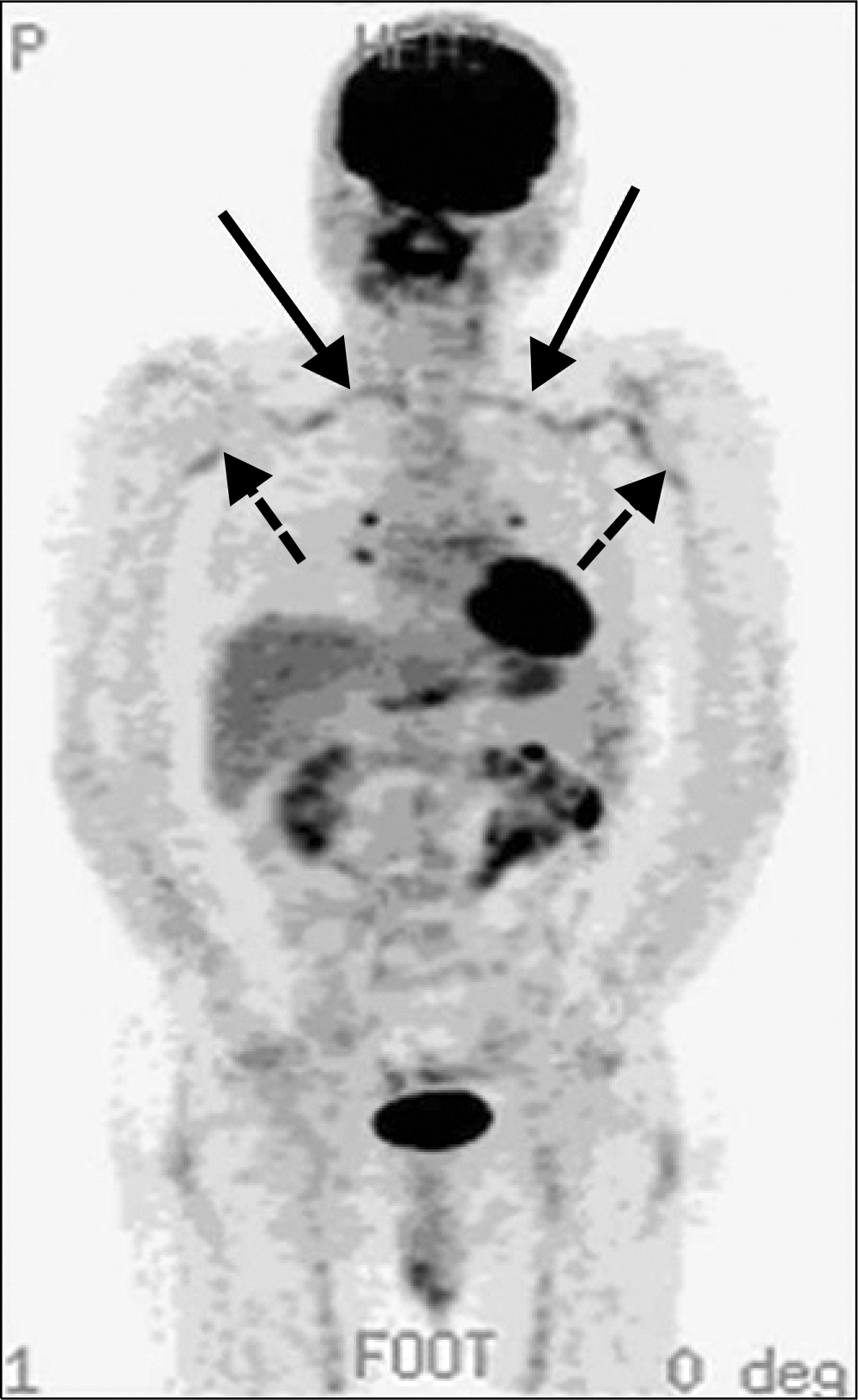
Article3). Chang HK., Hur SH., Chung HR. A case of giant cell arteritis developed in polymyalgia rheumatica. J Korean Rheum Assoc. 2000. 7:72–6.4). Ryu YB., Han KR., Kim C. A case report of giant ccell arteritis combined with oculomotor nurve palsy. Korean J Pain. 2007. 20:255–7.5). Liozon E., Boutros-Toni F., Ly K., Loustaud-Ratti V., Soria P., Vidal E. Silnet, or masked, giant cell arteritis is associated with as strong inflammatory response and a benign short term course. J Rheumatol. 2003. 30:1272–6.6). Kwon CM., Hong YH., Chun KA., Cho IH., Kim MJ., Shin DG, et al. A case of silent giant cell arteritis involving the entire aorta, carotid artery and brachial artery screened by integrated PET/CT. Clin Rheumatol. 2007. 26:1959–62.
Article7). Wang X., Hu ZP., Lu W., Tang XQ., Yang HP., Zeng LW, et al. Giant cell arteritis. Rheumatol Int. 2008. 29:1–7.
Article8). Kelly J., Rudd AG. Giant cell arteritis presenting with arm claudication. Age and Ageing. 2001. 30:167–9.
Article9). Kermani TA., Matteson EL., Hunder GG., Warrington KJ. Symptomatic lower extremity vasculitis in giant cell arteritis: a case series. J Rheumatol. 2009. 36:2277–83.
Article10). Pipitone N., Versari C., Salvarani C. Role of imging studies in the diagnosis and follow-up of large-vessel vasculitis: an update. Rheumatology. 2008. 47:403–8.11). Belloli L., Rodari M., Massarotti M., Conciato L., Chiti A., Marasini B. A case of atypical giant cell arteritis diagnosed by positron emission tomography PET. Clin Rheumatol. 2008. 27:799–801.
Article12). Tato F., Hoffman U. Giant cell arteritis: a systemic vascular disease. Vasc Med. 2008. 13:127–40.
Article13). Walter MA. [18F] Fluorodeoxyglucose PET in large vessel vasculitis. Radiol Clin N Am. 2007. 45:735–44.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Giant Cell Arteritis developed in Polymyalgia Rheumatica
- Giant cell arteritis of the breast: a case report
- A Case of Atypical Giant Cell Arteritis Presenting as a Fever of Unknown Origin
- Case of Brain Biopsy Proven Giant Cell Arteritis
- A Case of Subtype Giant Cell Arteritis Without Symptoms of Arteritic Anterior Ischemic Optic Neuropathy