J Korean Rheum Assoc.
2007 Dec;14(4):417-421.
A Case of Hypothenar Hammer Syndrome Presented as Digital Ulcerations
- Affiliations
-
- 1Department of Internal Medicine, Kyungpook National University School of Medicine, Daegu, Korea. ymkang@knu.ac.kr
Abstract
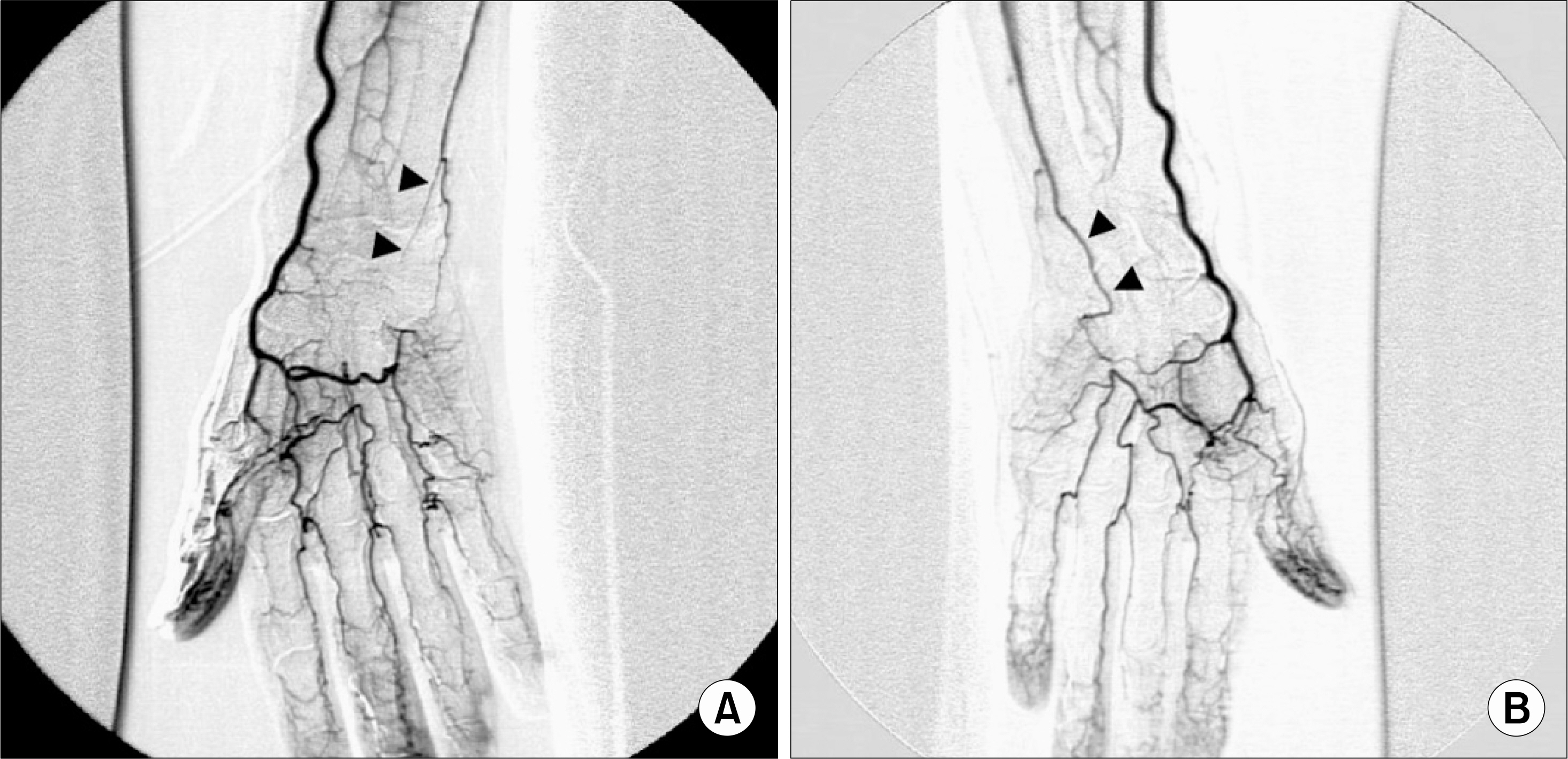
- Hypothenar hammer syndrome (HHS) is a non-atherosclerotic, non-inflammatory vascular disease that causes a digital ischemia as a result of the occlusion of distal ulnar artery adjacent to the hook of hamate. This syndrome is usually observed in men who use the hypothenar eminence of the hand to grip devices such as a hammer. As a consequence of repeated blunt trauma, the ulnar artery beneath hypothenar eminence may lead to pathologic changes, such as intima-medial hyperplasia and reactive inflammatory infiltrates, which lead to the digital ischemia. We experienced a case of HHS with digital ulcerations which occurred after intensive work with nail remover for 10 days. Selective angiography of right forearm showed complete occlusion of the ulnar artery at the level of hook of hamate with deficient superficial palmar arch. After treatment with intravenous prostaglandin E1 and heparin, the ulcerative lesions of fingers improved without surgical intervention, which implicates that medical management of HHS should be considered prior to the surgical treatment.
MeSH Terms
Figure
Reference
-
1). Ferris BL., Taylor LM Jr., Oyama K., McLafferty RB., Edwards JM., Moneta GL, et al. Hypothenar hammer syndrome: proposed etiology. J Vasc Surg. 2000. 31:104–13.
Article2). Stone JR. Intimal hyperplasia in the distal ulnar artery; influence of gender and implications for the hypothenar hammer syndrome. Cardiovasc Pathol. 2004. 13:20–5.3). Guazzo EP., Hicks BL., Keary PJ. Hypothenar hammer syndrome. Med J Aust. 1986. 145:174–5.
Article4). Spencer-Green G., Morgan GJ., Brown L., FitzGerald O. Hypothenar hammer syndrome: an occupational cause of Raynaud's phenomenon. J Rheumatol. 1987. 14:1048–51.5). Lambert M., Hatron PY., Hachulla E., Devulder B. Hypothenar hammer syndrome followed by systemic sclerosis. J Rheumatol. 2000. 27:2516–7.6). Liskutin J., Dorffner R., Resinger M., Silberbauer K., Mostbeck G. Hypothenar hammer syndrome. Eur Radiol. 2000. 10:542.
Article7). Higgins JP., Orlando GS., Chang P., Serletti JM. Hypothenar hammer syndrome after radial forearm flap harvest: a case report. J Hand Surg [Am]. 2001. 26:772–5.
Article8). Wong GB., Whetzel TP. Hypothenar hammer syndrome–review and case report. Vasc Surg. 2001. 35:163–6.9). Birrer M., Baumgartner I. Images in clinical medicine. Work-related vascular injuries of the hand–hypothenar hammer syndrome. N Engl J Med. 2002. 347:339.10). Taylor LM Jr. Hypothenar hammer syndrome. J Vasc Surg. 2003. 37:697.11). Abudakka M., Pillai A., Al-Khaffaf H. Hypothenar hammer syndrome: rare or underdiagnosed? Eur J Vasc Endovasc Surg. 2006. 32:257–60.
Article12). Thompson A., House R. Hand-arm vibration syndrome with concomitant arterial thrombosis in the hands. Occup Med (Lond). 2006. 56:317–21.
Article13). Gellman H., Botte MJ., Shankwiler J., Gelberman RH. Arterial patterns of the deep and superficial palmar arches. Clin Orthop Relat Res. 2001. 41–6.
Article14). Aleksic M., Heckenkamp J., Gawenda M., Brunkwall J. Occupation-related vascular disorders of the upper extremity–two case reports. Angiology. 2006. 57:107–14.15). Wheatley MJ., Marx MV. The use of intra-arterial urokinase in the management of hand ischemia secondary to palmar and digital arterial occlusion. Ann Plast Surg. 1996. 37:356–62.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Peripheral Arterial Bypass Using Interpositional Vein Graft in the Hypothenar Hammer Syndrome
- Fistulized Pseudoaneurysm Associated with Hypothenar Hammer Syndrome to the Skin in a 12-Year-Old Patient: A Case Report
- A case of Infantile Digital Fibromatosis Locaated on Hypothenar Area Showing Spontaneous Regression
- Posttraumatic Arteriovenous Hemangioma of the Hypothenar Eminence in a Car Mechanic
- Treatment of Lesser Toe Deformities