J Korean Foot Ankle Soc.
2014 Sep;18(3):108-114. 10.14193/jkfas.2014.18.3.108.
Functional Evaluation after Modified Brostrom Procedure with Suture Bridge Technique for Chronic Ankle Instability in Athletes
- Affiliations
-
- 1Department of Orthopaedic Surgery, Chungbuk National University College of Medicine, Cheongju, Korea. cbk@chungbuk.ac.kr
- KMID: 2333474
- DOI: http://doi.org/10.14193/jkfas.2014.18.3.108
Abstract
- PURPOSE
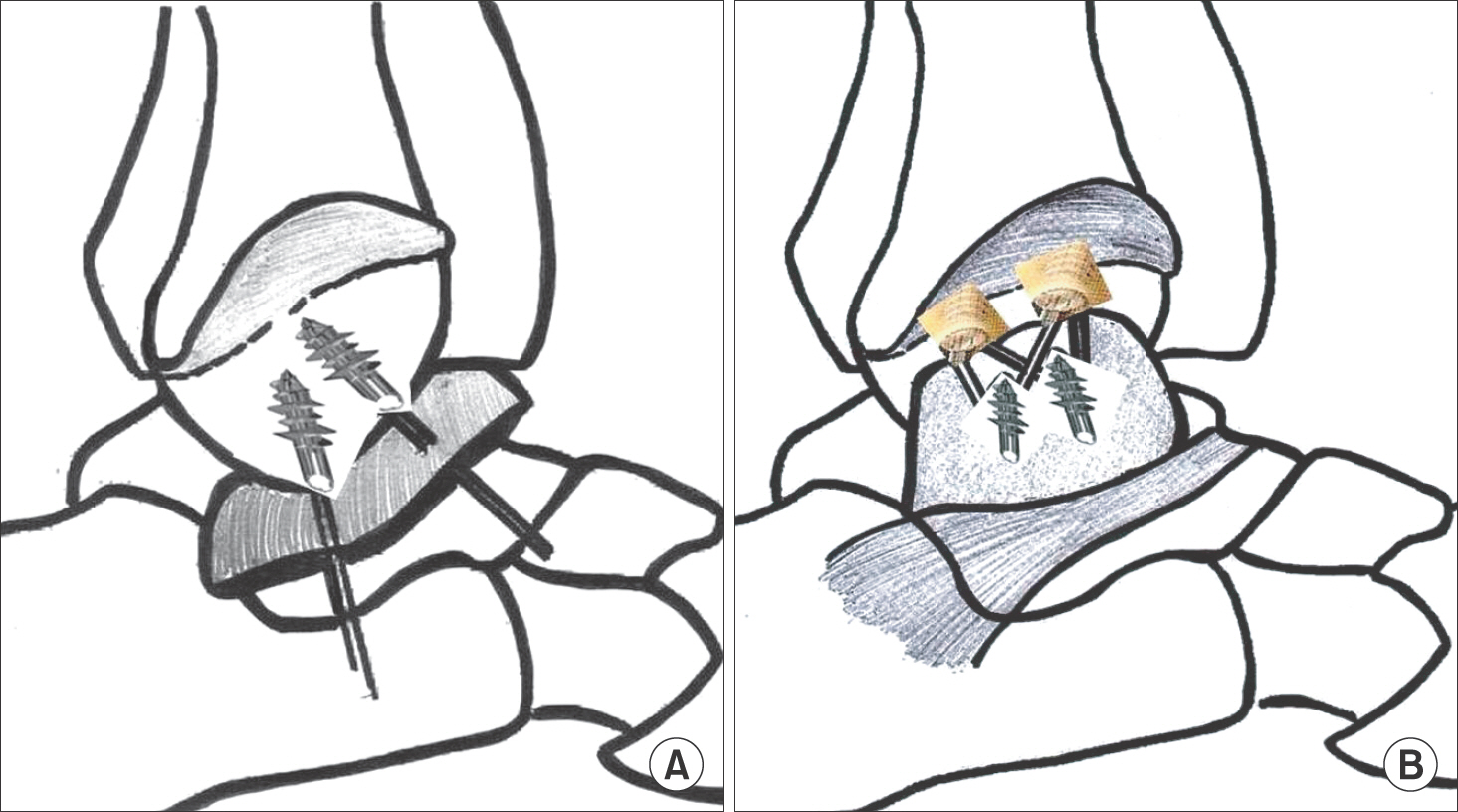
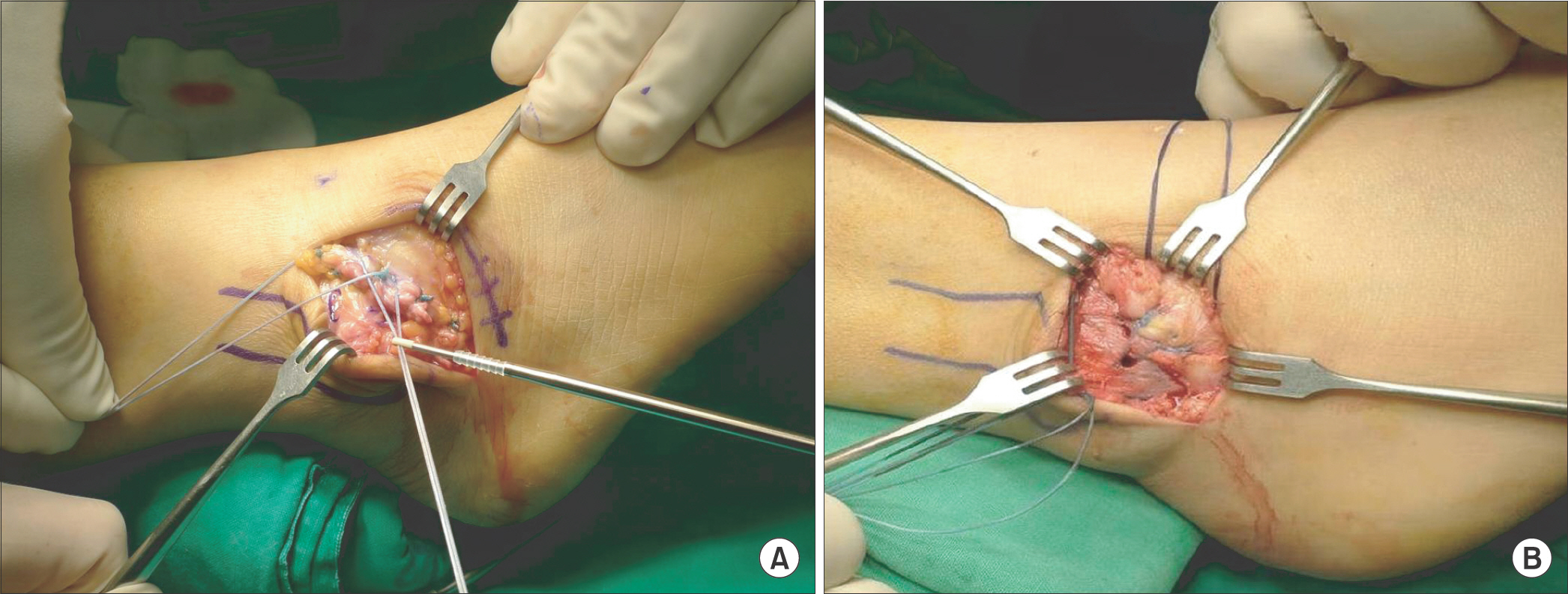
Ligament reattachment technique using a suture anchor appears to show satisfactory functional outcomes and mechanical stability compared with conventional bone tunnel technique. This study was prospectively conducted in order to evaluate functional outcomes of modified Brostrom procedures using the suture bridge technique for chronic ankle instability in athletes.
MATERIALS AND METHODS
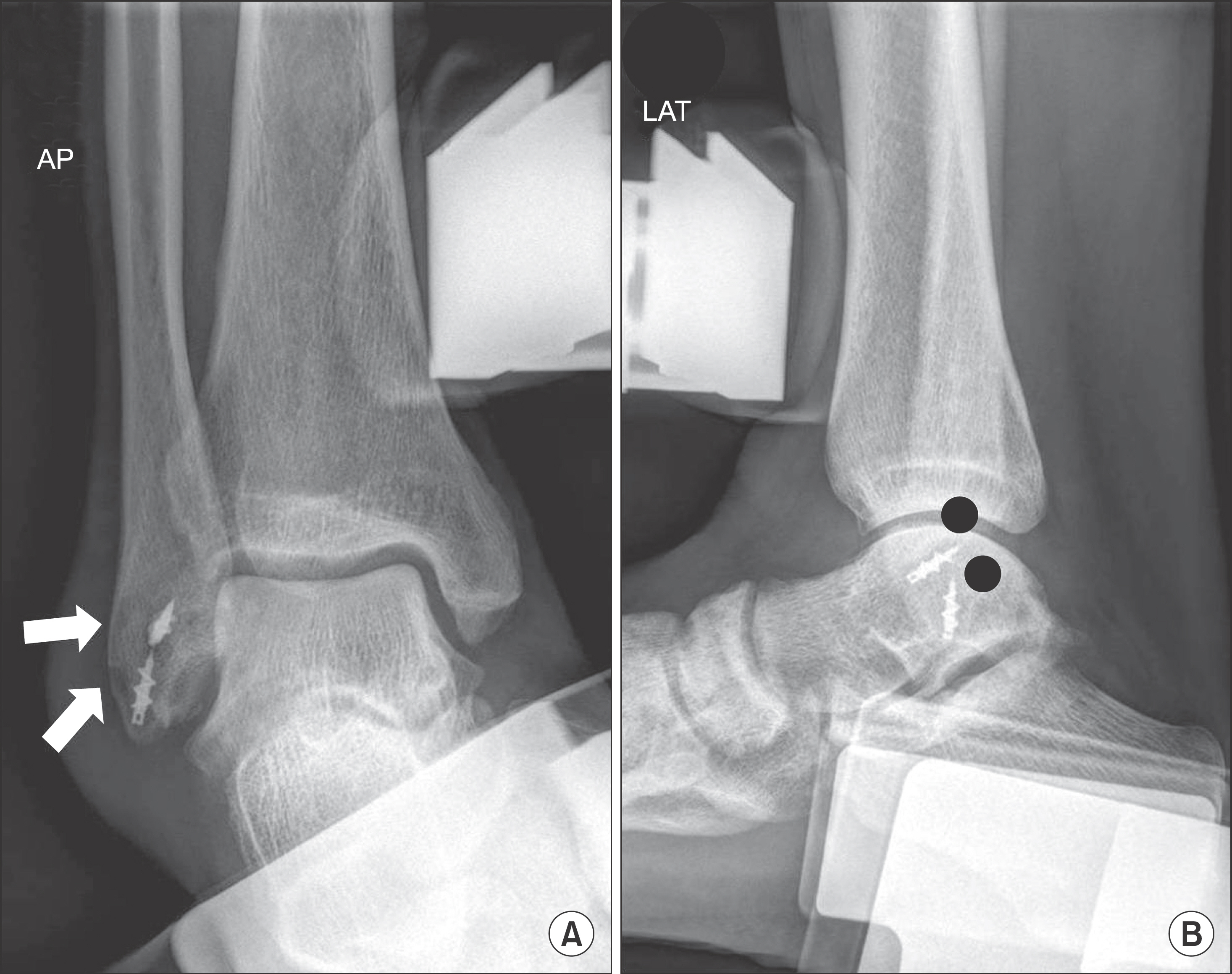
Twenty eight athletes under 30 years of age were followed for more than two years after undergoing the modified Brostrom procedure using the suture bridge technique. Functional evaluation consisted of the foot and ankle outcome score (FAOS), foot and ankle ability measure (FAAM) score. Range of motion and time to return to exercise were evaluated using a periodic questionnaire. Talar tilt angle and anterior talar translation were measured through stress radiographs for evaluation of mechanical stability.
RESULTS
FAOS improved significantly from preoperative mean 59.4 points to 91.4 points (p<0.001). Daily living and sport activity scores of FAAM improved significantly from preoperative mean 50.5, 32.5 points to 94.8, 87.3 points, respectively (p<0.001). Talar tilt angle and anterior talar translation improved significantly from preoperative mean 16.8degrees, 13.5 mm to 4.2degrees, 4.1 mm at final follow-up (p<0.001). Times to return to exercise were as follows: mean 10.2 weeks in jogging, 15.4 weeks in spurt running, 13.1 weeks in jumping, 11.5 weeks in walking on uneven ground, 9.1 weeks in standing on one leg, 7.2 weeks in tip-toeing gait, 8.4 weeks in squatting, and 10.6 weeks in descending stairs.
CONCLUSION
Modified Brostrom procedure using the suture bridge technique showed satisfactory functional outcomes for chronic ankle instability in athletes. Optimal indication and cost-effectiveness of the suture bridge technique will be studied in the future.
Keyword
MeSH Terms
Figure
Reference
-
1.Pederson B., Tesoro D., Wertheimer SJ., Coraci M. Mitek Anchor System: a new technique for tenodesis and ligamentous repair of the foot and ankle. J Foot Surg. 1991. 30:48–51.2.Messer TM., Cummins CA., Ahn J., Kelikian AS. Outcome of the modified Broström procedure for chronic lateral ankle instability using suture anchors. Foot Ankle Int. 2000. 21:996–1003.
Article3.Cho BK., Kim YM., Kim DS., Choi ES., Shon HC., Park KJ. Comparison between suture anchor and transosseous suture for the modified-Broström procedure. Foot Ankle Int. 2012. 33:462–8.
Article4.Cho BK., Kim YM., Kim DS., Choi ES., Shon HC., Park KJ. Outcomes of the modified Brostrom procedure using suture anchors for chronic lateral ankle instability--a prospective, randomized comparison between single and double suture anchors. J Foot Ankle Surg. 2013. 52:9–15.
Article5.Giza E., Nathe R., Nathe T., Anderson M., Campanelli V. Strength of bone tunnel versus suture anchor and push-lock construct in Broström repair. Am J Sports Med. 2012. 40:1419–23.
Article6.Karlsson J., Bergsten T., Lansinger O., Peterson L. Reconstruction of the lateral ligaments of the ankle for chronic lateral instability. J Bone Joint Surg Am. 1988. 70:581–8.
Article7.Krips R., van Dijk CN., Lehtonen H., Halasi T., Moyen B., Karlsson J. Sports activity level after surgical treatment for chronic anterolateral ankle instability. A multicenter study. Am J Sports Med. 2002. 30:13–9.8.Li X., Killie H., Guerrero P., Busconi BD. Anatomical reconstruction for chronic lateral ankle instability in the high-demand athlete: functional outcomes after the modified Broström repair using suture anchors. Am J Sports Med. 2009. 37:488–94.9.Bahr R., Pena F., Shine J., Lew WD., Tyrdal S., Engebretsen L. Biomechanics of ankle ligament reconstruction. An in vitro comparison of the Broström repair, Watson-Jones reconstruction, and a new anatomic reconstruction technique. Am J Sports Med. 1997. 25:424–32.10.Riegler HF. Reconstruction for lateral instability of the ankle. J Bone Joint Surg Am. 1984. 66:336–9.
Article11.Snook GA., Chrisman OD., Wilson TC. Long-term results of the Chrisman-Snook operation for reconstruction of the lateral ligaments of the ankle. J Bone Joint Surg Am. 1985. 67:1–7.
Article12.Hennrikus WL., Mapes RC., Lyons PM., Lapoint JM. Outcomes of the Chrisman-Snook and modified-Broström procedures for chronic lateral ankle instability. A prospective, randomized comparison. Am J Sports Med. 1996. 24:400–4.13.Lee KT., Young KW., Bae SW., Lee JH. Analysis of affecting factors of modified Brostrom procedure in chronic ankle lateral insta-bility. J Korean Soc Foot Surg. 2002. 6:66–72.14.Roos EM., Brandsson S., Karlsson J. Validation of the foot and ankle outcome score for ankle ligament reconstruction. Foot Ankle Int. 2001. 22:788–94.
Article15.Martin RL., Irrgang JJ., Burdett RG., Conti SF., Van Swearingen JM. Evidence of validity for the Foot and Ankle Ability Measure (FAAM). Foot Ankle Int. 2005. 26:968–83.16.Takao M., Miyamoto W., Matsui K., Sasahara J., Matsushita T. Functional treatment after surgical repair for acute lateral ligament disruption of the ankle in athletes. Am J Sports Med. 2012. 40:447–51.
Article17.Brady PC., Arrigoni P., Burkhart SS. Evaluation of residual rotator cuff defects after in vivo single- versus double-row rotator cuff repairs. Arthroscopy. 2006. 22:1070–5.
Article18.Sugaya H., Maeda K., Matsuki K., Moriishi J. Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthroscopy. 2005. 21:1307–16.
Article19.Cho NS., Lee BG., Rhee YG. Arthroscopic rotator cuff repair using a suture bridge technique: is the repair integrity actually maintained? Am J Sports Med. 2011. 39:2108–16.20.Park MC., ElAttrache NS., Tibone JE., Ahmad CS., Jun BJ., Lee TQ. Part I: Footprint contact characteristics for a transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg. 2007. 16:461–8.
Article21.Park MC., Tibone JE., ElAttrache NS., Ahmad CS., Jun BJ., Lee TQ. Part II: Biomechanical assessment for a footprint-restoring transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg. 2007. 16:469–76.
Article22.Yi JW., Cho NS., Cho SH., Rhee YG. Arthroscopic suture bridge repair technique for full thickness rotator cuff tear5 Clin Orthop Surg. 2010. 2:105–11.23.Karlsson J., Peterson L. Evaluation of ankle joint function: the use of a scoring scale. The Foot. 1991. 1:15–9.
Article24.Sefton GK., George J., Fitton JM., McMullen H. Reconstruction of the anterior talofibular ligament for the treatment of the unstable ankle. J Bone Joint Surg Br. 1979. 61:352–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Outcomes of Arthroscopic Modified Brostrom Procedure in Chronic Lateral Ankle Instability
- Modified Brostrom Procedure with Suture Anchor & PushLock Anchor in Lateral Ankle Instability
- Anatomical Repair for Chronic Lateral Ankle Instability
- Treatment of Chronic Ankle Lateral Instability using Modified Brostrom Procedure with Anchor suture&Arthroscopy
- Treatment of Chronic Lateral Ankle Instability: A Modified Broström Technique Using All-Suture Anchor