J Korean Assoc Pediatr Surg.
2014 Jun;20(1):12-16.
Clinical Analysis of Foreign Bodies in Gastrointestinal Tract in Children
- Affiliations
-
- 1Department of Surgery, Chonnam National University School of Medicine, Gwangju, Korea. choisjn@chonnam.ac.kr
Abstract
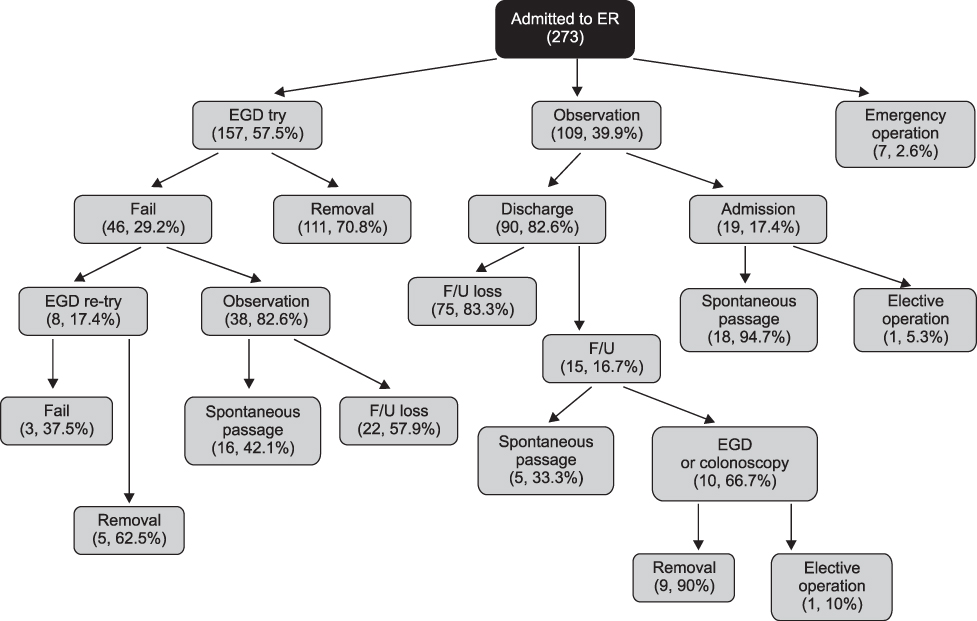
- Foreign body ingestion is a common problem among paediatric populations. Most of the ingested foreign bodies spontaneously pass through the gastrointestinal tract, but approximately less then 10% of them remain without being discharged, and trigger complications. Therefore, proper evaluation and treatment according to the situation is required. In this study, clinical progress and complications were analyzed according to the clinical features and treatment in children who ingested foreign bodies. Among pediatric patients under 18 who were admitted to Chonnam National University Hospital after ingesting foreign bodies between January 2008 to June 2012, only the patients who had their foreign body in the gastrointestinal tract were included in this study. Based on medical records, age, type of foreign body, time spent till admission, and whether the endoscopy was done or not, complication were researched retrospectively. According to symptoms and plain abdomen X-ray findings, treatment was chosen and conducted among endoscopy, observation and emergency operation. Among 273 patients, 9 (3.3%) of them had surgical removal. Seven (2.6%) of them had an emergency operation on the day of admission, and the rest 2 (0.7%) had operation during observation. Removal through initial endoscopic approach was tried in 157 (57.5%) patients. Eleven (70.8%) of them had their foreign body removed at the initial trial, and 5 (4.9%) of them at the second trial. Among 109, who were on observation status, 9 (8.3%) of them needed endoscopic removal, and 2 (1.8%) of them suffered from surgical removal. It is thought to be better to approach slowly considering the type, size and symptoms in foreign body ingestion of pediatric patients, rather than immediate and invasive removal.
Keyword
MeSH Terms
Figure
Reference
-
1. McNeill MB, Sperry SL, Crockett SD, Miller CB, Shaheen NJ, Dellon ES. Epidemiology and management of oesophageal coin impaction in children. Dig Liver Dis. 2012; 44:482–486.
Article2. Tander B, Yazici M, Rizalar R, Ariturk E, Ayyildiz SH, Bernay F. Coin ingestion in children: which size is more risky? J Laparoendosc Adv Surg Tech A. 2009; 19:241–243.
Article3. Chen X, Milkovich S, Stool D, van As AB, Reilly J, Rider G. Pediatric coin ingestion and aspiration. Int J Pediatr Otorhinolaryngol. 2006; 70:325–329.
Article4. Schunk JE, Corneli H, Bolte R. Pediatric coin ingestions. A prospective study of coin location and symptoms. Am J Dis Child. 1989; 143:546–548.5. Panieri E, Bass DH. The management of ingested foreign bodies in children--a review of 663 cases. Eur J Emerg Med. 1995; 2:83–87.6. Conners GP, Chamberlain JM, Weiner PR. Pediatric coin ingestion: a home-based survey. Am J Emerg Med. 1995; 13:638–640.
Article7. Allotey J, Duncan H, Williams H. Mediastinitis and retropharyngeal abscess following delayed diagnosis of glass ingestion. Emerg Med J. 2006; 23:e12.
Article8. Wright CC, Closson FT. Updates in pediatric gastrointestinal foreign bodies. Pediatr Clin North Am. 2013; 60:1221–1239.
Article9. Volle E, Beyer P, Kaufmann HJ. Therapeutic approach to ingested button-type batteries. Magnetic removal of ingested button-type batteries. Pediatr Radiol. 1989; 19:114–118.10. Litovitz T, Whitaker N, Clark L. Preventing battery ingestions: an analysis of 8648 cases. Pediatrics. 2010; 125:1178–1183.
Article11. Namasivayam S. Button battery ingestion: a solution to a management dilemma. Pediatr Surg Int. 1999; 15:383–384.
Article12. Honzumi M, Shigemori C, Ito H, Mohri Y, Urata H, Yamamoto T. An intestinal fistula in a 3-year-old child caused by the ingestion of magnets: report of a case. Surg Today. 1995; 25:552–553.
Article13. Martin A. Safety worry leads to end of a popular toy magnet [Internet]. New York (NY): The New York Times; 2012 Dec 17; [cited 2014 Feb 20]. Available from: http://www.nytimes.com/2012/12/18/business/maker-of-buckyballs-says-it-will-stop-selling-them.html?_r=0.14. Lelli JL. Foreign bodies. In: Ashcraft KW, Hoder TM, editors. Pediatric Surgery, chap 11. ed 5. Philadelphia, PA: WB Sounders; 2010. pp. Pp141.15. Hussain SZ, Bousvaros A, Gilger M, Mamula P, Gupta S, Kramer R, Noel RA. Management of ingested magnets in children. J Pediatr Gastroenterol Nutr. 2012; 55:239–242.
Article16. Da Silva EJ, Golakai VK. Foreign body causing chronic subacute small bowel obstruction: an unusual case from Harare Hospital. Cent Afr J Med. 1998; 44:16–18.17. Lelli JL. Foreign bodies. In: Ashcraft KW, Hoder TM, editors. Pediatric Surgery, chap 11. ed 5. Philadelphia, PA: WB Sounders; 2010. pp. Pp141.18. Messner AH. Pitfalls in the diagnosis of aerodigestive tract foreign bodies. Clin Pediatr (Phila). 1998; 37:359–365.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Foreign Bodies in the upper Gastrointestinal Tract Diagnosed by Endoscopy
- Upper Gastrointestinal Tract Foreign Bodies
- Gastrointestinal Foreign Bodies in Children: Experiences of 60 Cases in Kangwon, Korea
- Review of 78 Cases Foreign Body in the Upper Gastrointestinal Tract
- What is the Principle of Endoscopic Removal Technique of Foreign Bodies in the Upper Gastrointestinal Tract?