Hip Pelvis.
2016 Jun;28(2):82-89. 10.5371/hp.2016.28.2.82.
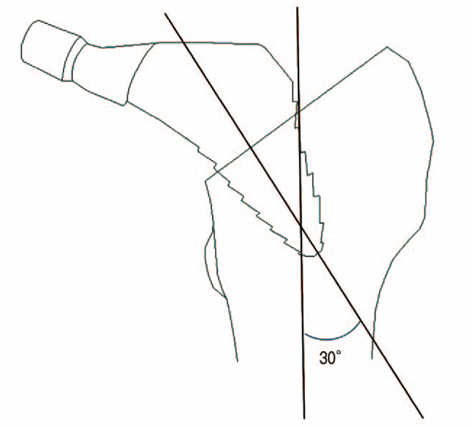
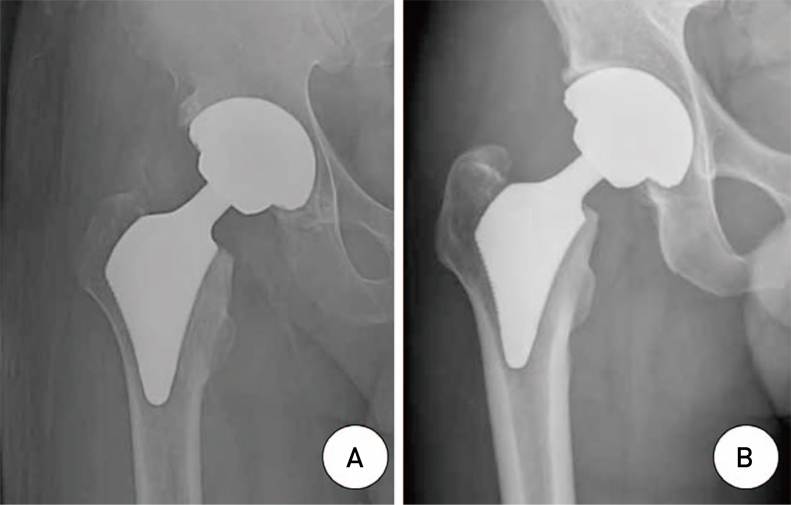
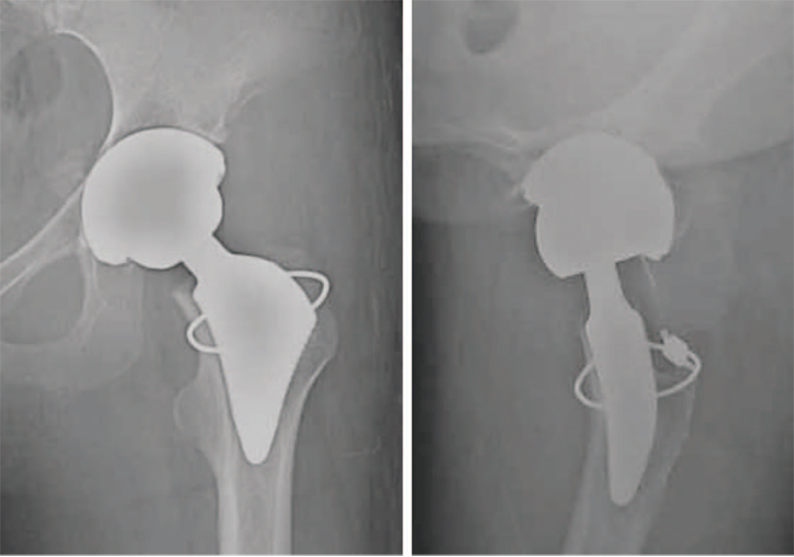
The Short-term Clinical Outcome of Total Hip Arthroplasty Using Short Metaphyseal Loading Femoral Stem
- Affiliations
-
- 1Department of Orthopaedic Surgery, Yonsei Sarang Hospital, Seoul, Korea.
- 2Department of Orthopaedic Surgery, Daegu Catholic University Medical Center, Daegu, Korea. p10001@hanmail.net
- KMID: 2328343
- DOI: http://doi.org/10.5371/hp.2016.28.2.82
Abstract
- PURPOSE
The purpose of this study was to retrospectively evaluate the short-term clinical and radiological outcomes of total hip arthroplasty (THA) with short metaphyseal loading femoral stem.
MATERIALS AND METHODS
We retrospectively reviewed the records of 56 cases in 47 patients who had undergone THA with short metaphyseal loading femoral stem from April 2010 to December 2011. There were 20 males and 27 females. The mean age was 54 years (range, 26-77 years). The average follow up period was 4.6 years. Clinical results were evaluated by Harris hip scores (HHS) before the operation and at the last follow-up. Radiographic analysis was done by evaluating osteolysis, loosening, stress shielding, and alignement.
RESULTS
The mean HHS significantly improved from 45 (range, 15-58) preoperatively to 98 (range, 85-100) at the last follow-up. In radiographic analyses, there was no evidence of osteolysis or loosening around the stems and the acetabuluar components. All cases showed rounding off of the calcar, grade 1 bone resorption of the proximal femur. With regard to implant alignment, 51 femoral component (91.1%) were in neutral position, and 5 (8.9%) were in varus position. There was 1 intraoperative fracture treated by cerclage wiring and no case was revised during follow-up period.
CONCLUSION
Although longer follow-up is needed to confirm the durability of the short metaphyseal loading femoral stem, this short stem might provide stable fixation without diaphyseal fixation and demonstrated good clinical result at mean 4.6 year short term follow-up.
MeSH Terms
Figure
Reference
-
1. Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005; 87:1487–1497.
Article2. Ulrich SD, Seyler TM, Bennett D, et al. Total hip arthroplasties: what are the reasons for revision? Int Orthop. 2008; 32:597–604.
Article3. Morrey BF. Short-stemmed uncemented femoral component for primary hip arthroplasty. Clin Orthop Relat Res. 1989; (249):169–175.
Article4. Tóth K, Mécs L, Kellermann P. Early experience with the Depuy Proxima short stem in total hip arthroplasty. Acta Orthop Belg. 2010; 76:613–618.5. Judet J, Judet R. The use of an artificial femoral head for arthroplasty of the hip joint. J Bone Joint Surg Br. 1950; 32-B:166–173.
Article6. Fink B, Wessel S, Deuretzbacher G, Protzen M, Ruther W. Midterm results of "thrust plate" prosthesis. J Arthroplasty. 2007; 22:703–710.
Article7. Fottner A, Schmid M, Birkenmaier C, Mazoochian F, Plitz W, Volkmar J. Biomechanical evaluation of two types of short-stemmed hip prostheses compared to the trust plate prosthesis by three-dimensional measurement of micromotions. Clin Biomech (Bristol, Avon). 2009; 24:429–434.
Article8. Morrey BF, Adams RA, Kessler M. A conservative femoral replacement for total hip arthroplasty. A prospective study. J Bone Joint Surg Br. 2000; 82:952–958.9. Learmonth ID. Conservative stems in total hip replacement. Hip Int. 2009; 19:195–200.
Article10. Kim YH, Kim JS, Joo JH, Park JW. A prospective short-term outcome study of a short metaphyseal fitting total hip arthroplasty. J Arthroplasty. 2012; 27:88–94.
Article11. Santori N, Lucidi M, Santori FS. Proximal load transfer with a stemless uncemented femoral implant. J Orthop Traumatol. 2006; 7:154–160.
Article12. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969; 51:737–755.
Article13. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976; (121):20–32.
Article14. Dorr LD, Absatz M, Gruen TA, Saberi MT, Doerzbacher JF. Anatomic Porous Replacement hip arthroplasty: first 100 consecutive cases. Semin Arthroplasty. 1990; 1:77–86.15. Martell JM, Pierson RH 3rd, Jacobs JJ, Rosenberg AG, Maley M, Galante JO. Primary total hip reconstruction with a titanium fiber-coated prosthesis inserted without cement. J Bone Joint Surg Am. 1993; 75:554–571.
Article16. Tanzer M, Maloney WJ, Jasty M, Harris WH. The progression of femoral cortical osteolysis in association with total hip arthroplasty without cement. J Bone Joint Surg Am. 1992; 74:404–410.
Article17. Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH. Structural and cellular assessment of bone quality of proximal femur. Bone. 1993; 14:231–242.
Article18. Ghera S, Pavan L. The DePuy Proxima hip: a short stem for total hip arthroplasty. Early experience and technical considerations. Hip Int. 2009; 19:215–220.
Article19. Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979; (141):17–27.20. Kim YH, Kim JS, Oh SH, Kim JM. Comparison of porous-coated titanium femoral stems with and without hydroxyapatite coating. J Bone Joint Surg Am. 2003; 85-A:1682–1688.
Article21. Engh CA Jr, Claus AM, Hopper RH Jr, Engh CA. Long-term results using the anatomic medullary locking hip prosthesis. Clin Orthop Relat Res. 2001; (393):137–146.
Article22. Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973; 55:1629–1632.23. McMinn DJ, Daniel J, Pradhan C, Ziaee H. Avascular necrosis in the young patient: a trilogy of arthroplasty options. Orthopedics. 2005; 28:945–947.
Article24. Thomas W, Lucente L, Mantegna N, Grundei H. ESKA (CUT) endoprosthesis. Orthopade. 2004; 33:1243–1248.25. Walker PS, Culligan SG, Hua J, Muirhead-Allwood SK, Bentley G. Stability and bone preservation in custom designed revision hip stems. Clin Orthop Relat Res. 2000; (373):164–173.
Article26. Yoo JH, Kim SG, Han CD, Oh HC, Yoon HK. Cementless total hip arthroplasty using VerSys fiber metal midcoat stem: a minimum 3-years follow-up. J Korean Hip Soc. 2010; 22:45–51.
Article27. Kim YH, Oh SH, Kim JS. Primary total hip arthroplasty with a second-generation cementless total hip prosthesis in patients younger than fifty years of age. J Bone Joint Surg Am. 2003; 85-A:109–114.
Article28. Westphal FM, Bishop N, Honl M, Hille E, Püschel K, Morlock MM. Migration and cyclic motion of a new short-stemmed hip prosthesis--a biomechanical in vitro study. Clin Biomech (Bristol, Avon). 2006; 21:834–840.
Article29. Santori FS, Manili M, Fredella N, Tonci Ottieri M, Santori N. Ultra-short stems with proximal load transfer: clinical and radiographic results at five-year follow-up. Hip Int. 2006; 16:Suppl 3. 31–39.
Article30. Kim YH, Kim VE. Early migration of uncemented porous coated anatomic femoral component related to aseptic loosening. Clin Orthop Relat Res. 1993; (295):146–155.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultra-Short Bone Conserving Cementless Femoral Stem
- Favorable Functional Recovery and Stem Stability after Hip Arthroplasty with a Short Metaphyseal Stem in Elderly Patients with Osteoporotic Femoral Neck Fractures
- Short-term Results after Cementless Total Hip Arthroplasty Using a Fully Hydroxyapatite-coated Femoral Stem
- Short Term Results of Cementless Revision Total Hip Arthroplasty using an Interlocking Femoral Stem
- Porous Femoral Fixation in Total Hip Arthroplasty with Short Anatomical Stem: Radiographic Evaluation