Ann Rehabil Med.
2016 Jun;40(3):432-439. 10.5535/arm.2016.40.3.432.
Characteristics of Dysphagia in Severe Traumatic Brain Injury Patients: A Comparison With Stroke Patients
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Rehabilitation Medicine, Gangwon-Do Rehabilitation Hospital, Chuncheon, Korea. tairyoon@snu.ac.kr
- KMID: 2327604
- DOI: http://doi.org/10.5535/arm.2016.40.3.432
Abstract
OBJECTIVE
To compare the swallowing characteristics of dysphagic patients with traumatic brain injury (TBI) with those of dysphagic stroke patients.
METHODS
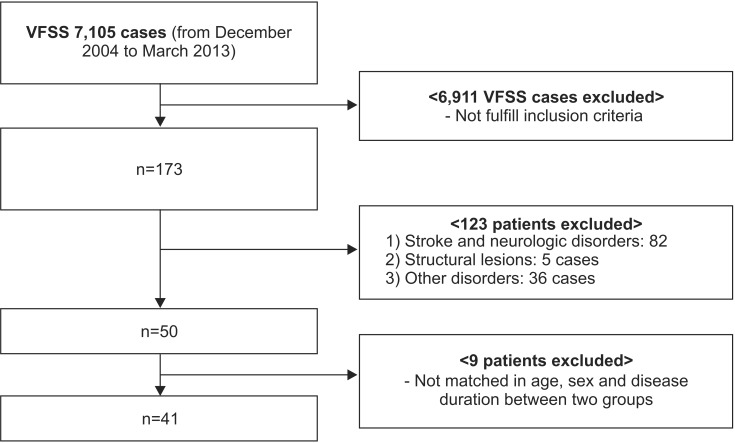
Forty-one patients with TBI were selected from medical records (between December 2004 to March 2013) and matched to patients with stroke (n=41) based on age, sex, and disease duration. Patients' swallowing characteristics were analyzed retrospectively using a videofluoroscopic swallowing study (VFSS) and compared between both groups. Following thorough review of medical records, patients who had a history of diseases that could affect swallowing function at the time of the study were excluded. Dysphagia characteristics and severity were evaluated using the American Speech-Language-Hearing Association National Outcome Measurement System swallowing scale, clinical dysphagia scale, and the videofluoroscopic dysphagia scale.
RESULTS
There was a significant difference in radiological lesion location (p=0.024) between the two groups. The most common VFSS finding was aspiration or penetration, followed by decreased laryngeal elevation and reduced epiglottis inversion. Swallowing function, VFSS findings, or quantified dysphagia severity showed no significant differences between the groups. In a subgroup analysis of TBI patients, the incidence of tube feeding was higher in patients with surgical intervention than in those without (p=0.011).
CONCLUSION
The swallowing characteristics of dysphagic patients after TBI were comparable to those of dysphagic stroke patients. Common VFSS findings comprised aspiration or penetration, decreased laryngeal elevation, and reduced epiglottis inversion. Patients who underwent surgical intervention after TBI were at high risk of tube feeding requirement.
MeSH Terms
Figure
Cited by 2 articles
-
Characteristics and Clinical Course of Dysphagia Caused by Anterior Cervical Osteophyte
Hee Eun Choi, Geun Yeol Jo, Woo Jin Kim, Hwan Kwon Do, Jun Koo Kwon, Se Heum Park
Ann Rehabil Med. 2019;43(1):27-37. doi: 10.5535/arm.2019.43.1.27.Predictors for Failed Removal of Nasogastric Tube in Patients With Brain Insult
Shih-Ting Huang, Tyng-Guey Wang, Mei-Chih Peng, Wan-Ming Chen, An-Tzu Jao, Fuk Tan Tang, Yu-Ting Hsieh, Chun Sheng Ho, Shu-Ming Yeh
Ann Rehabil Med. 2024;48(3):220-227. doi: 10.5535/arm.230011.
Reference
-
1. Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006; 21:375–378. PMID: 16983222.2. Winstein CJ. Neurogenic dysphagia. Frequency, progression, and outcome in adults following head injury. Phys Ther. 1983; 63:1992–1997. PMID: 6647555.3. Mackay LE, Morgan AS, Bernstein BA. Factors affecting oral feeding with severe traumatic brain injury. J Head Trauma Rehabil. 1999; 14:435–447. PMID: 10653939.
Article4. Terre R, Mearin F. Prospective evaluation of oro-pharyngeal dysphagia after severe traumatic brain injury. Brain Inj. 2007; 21:1411–1417. PMID: 18066943.6. Hansen TS, Larsen K, Engberg AW. The association of functional oral intake and pneumonia in patients with severe traumatic brain injury. Arch Phys Med Rehabil. 2008; 89:2114–2120. PMID: 18996240.
Article7. Hansen TS, Engberg AW, Larsen K. Functional oral intake and time to reach unrestricted dieting for patients with traumatic brain injury. Arch Phys Med Rehabil. 2008; 89:1556–1562. PMID: 18674990.
Article8. Terre R, Mearin F. Videofluoroscopy quantification of laryngotracheal aspiration outcome in traumatic brain injury-related oropharyngeal dysphagia. Rev Esp Enferm Dig. 2007; 99:7–12. PMID: 17295592.9. Ward EC, Green K, Morton AL. Patterns and predictors of swallowing resolution following adult traumatic brain injury. J Head Trauma Rehabil. 2007; 22:184–191. PMID: 17510594.
Article10. Geeganage C, Beavan J, Ellender S, Bath PM. Interventions for dysphagia and nutritional support inacute and subacute stroke. Cochrane Database Syst Rev. 2012; 10:CD000323. PMID: 23076886.11. Rogus-Pulia N, Robbins J. Approaches to the rehabilitation of dysphagia in acute poststroke patients. Semin Speech Lang. 2013; 34:154–169. PMID: 24166190.
Article12. Chang YC, Chen SY, Lui LT, Wang TG, Wang TC, Hsiao TY, et al. Dysphagia in patients with nasopharyngeal cancer after radiation therapy: a videofluoroscopic swallowing study. Dysphagia. 2003; 18:135–143. PMID: 12825907.
Article13. Paik NJ, Kim IS, Kim JH, Oh BM, Han TR. Clinical validity of the functional dysphagia scale based on videofluoroscopic swallowing study. J Korean Acad Rehabil Med. 2005; 29:43–49.14. Jung SH, Lee KJ, Hong JB, Han TR. Validation of clinical dysphagia scale: based on videofluoroscopic swallowing study. J Korean Acad Rehabil Med. 2005; 29:343–350.15. Juneja G, Czyrny JJ, Linn RT. Admission balance and outcomes of patients admitted for acute inpatient rehabilitation. Am J Phys Med Rehabil. 1998; 77:388–393. PMID: 9798829.16. Eng JJ, Rowe SJ, McLaren LM. Mobility status during inpatient rehabilitation: a comparison of patients with stroke and traumatic brain injury. Arch Phys Med Rehabil. 2002; 83:483–490. PMID: 11932849.
Article17. Mackay LE, Morgan AS, Bernstein BA. Swallowing disorders in severe brain injury: risk factors affecting return to oral intake. Arch Phys Med Rehabil. 1999; 80:365–371. PMID: 10206596.
Article18. Tandon PN. Brain stem hemorrhage in cranio-cerebral trauma. Acta Neurol Scand. 1964; 40:375–385. PMID: 14215769.
Article19. Doty RW, Richmond WH, Storey AT. Effect of medullary lesions on coordination of deglutition. Exp Neurol. 1967; 17:91–106. PMID: 4959819.
Article20. Jean A. Brain stem control of swallowing: neuronal network and cellular mechanisms. Physiol Rev. 2001; 81:929–969. PMID: 11274347.
Article21. Albanese J, Leone M, Alliez JR, Kaya JM, Antonini F, Alliez B, et al. Decompressive craniectomy for severe traumatic brain injury: evaluation of the effects at one year. Crit Care Med. 2003; 31:2535–2538. PMID: 14530763.22. Stevens RD, Sutter R. Prognosis in severe brain injury. Crit Care Med. 2013; 41:1104–1123. PMID: 23528755.
Article23. Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005; 36:2756–2763. PMID: 16269630.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Application of Non-invasive Brain Stimulation on Dysphagia after Stroke
- Short-term Prognosis of Dysphagia in Acute Ischemic Brain Stroke
- Animal Models of Traumatic Brain Injury
- Epidemiology, Natural Recovery, Long-term Outcome of Post Stroke Dysphagia
- Post-Stroke Dysphagia: Incidence, Complications and Pattern Relates to Brain Lesion