Ann Surg Treat Res.
2016 Jul;91(1):29-36. 10.4174/astr.2016.91.1.29.
Initial experience with radical antegrade modular pancreatosplenectomy in a single institution
- Affiliations
-
- 1Department of Hepato-biliary and Pancreas Surgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. gshth@catholic.ac.kr
- KMID: 2327414
- DOI: http://doi.org/10.4174/astr.2016.91.1.29
Abstract
- PURPOSE
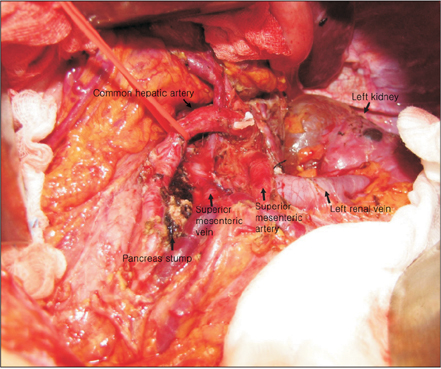
Radical antegrade modular pancreatosplenectomy (RAMPS) is expected to be favorable for obtaining the negative tangential margin with oncologic feasibility through the horizontal dissection in a right-to-left fashion for radical lymph node dissections.
METHODS
From January 2007 to February 2015, a total of 30 RAMPS and 19 conventional distal pancreatectomy (DP) cases were enrolled. The demographics, perioperative and survival outcomes were compared according to the type of surgery.
RESULTS
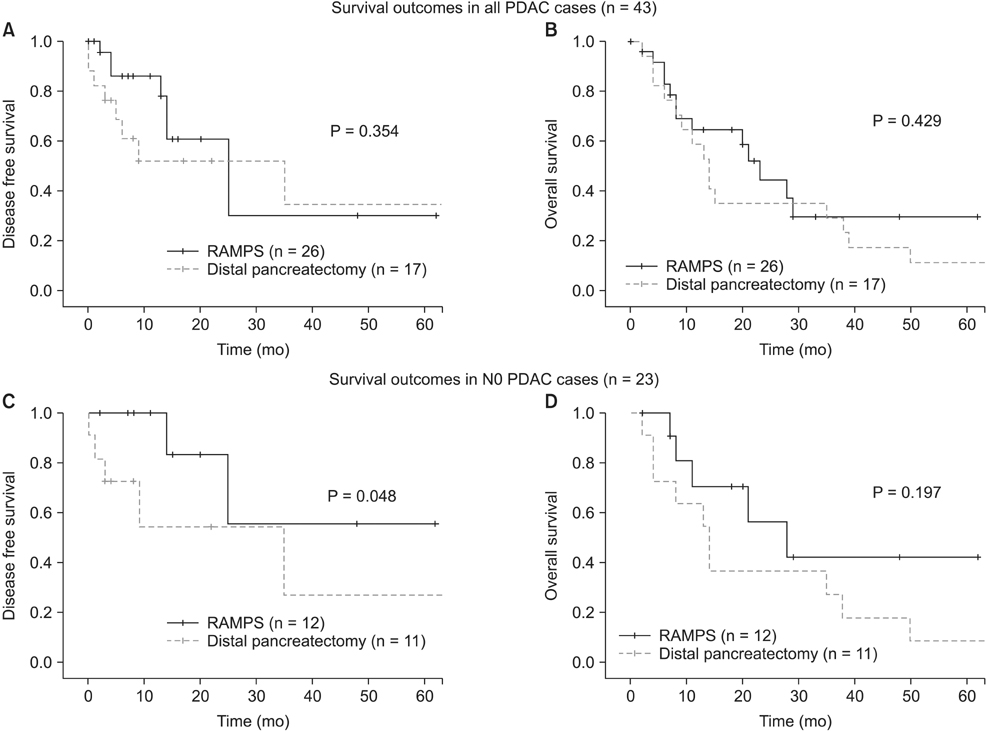
The mean operative time, blood loss and length of hospital stay were similar between 2 groups. Morbidities were reported in 14 cases of RAMPS (46.7%) and 8 cases of DP (42.1%) (P = 0.777). The rate of negative tangential margin (96.2%) and the number of harvested lymph nodes (mean ± standard deviation, 21.5 ± 8.3) were significantly higher in RAMPS group (P = 0.011, P = 0.003, respectively). In terms of survival outcomes, there was no significant difference in regard to the overall 3-year disease-free survival (DFS; 30.4% in RAMPS vs. 35.0% in DP, P = 0.354) or overall survival (OS; 29.9% vs. 29.4%, P = 0.429) between the 2 groups. After exclusion of cases with nodal invasion, however, the RAMPS group had a longer DFS than the DP group (55.6% vs. 27.3%, P = 0.048) although OS was similar without significant difference (42.4% vs. 27.3%, P = 0.197).
CONCLUSION
RAMPS is a safe and oncologically feasible procedure in left-sided pancreatic cancer by obtaining a successful negative tangential margin and radical lymph node dissection. The authors suggest it could also be useful for local control, especially for the limited left-sided pancreatic cancer without nodal invasion.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Korean Surgical Practice Guideline for Pancreatic Cancer 2022: A summary of evidence-based surgical approaches
Seung Eun Lee, Sung-Sik Han, Chang Moo Kang, Wooil Kwon, Kwang Yeol Paik, Ki Byung Song, Jae Do Yang, Jun Chul Chung, Chi-Young Jeong, Sun-Whe Kim
Ann Hepatobiliary Pancreat Surg. 2022;26(1):1-16. doi: 10.14701/ahbps.22-009.
Reference
-
1. Christein JD, Kendrick ML, Iqbal CW, Nagorney DM, Farnell MB. Distal pancreatectomy for resectable adenocarcinoma of the body and tail of the pancreas. J Gastrointest Surg. 2005; 9:922–927.2. Shoup M, Conlon KC, Klimstra D, Brennan MF. Is extended resection for adenocarcinoma of the body or tail of the pancreas justified? J Gastrointest Surg. 2003; 7:946–952.3. Niederhuber JE, Brennan MF, Menck HR. The National Cancer Data Base report on pancreatic cancer. Cancer. 1995; 76:1671–1677.4. Andren-Sandberg A, Wagner M, Tihanyi T, Lofgren P, Friess H. Technical aspects of left-sided pancreatic resection for cancer. Dig Surg. 1999; 16:305–312.5. Strasberg SM, Drebin JA, Linehan D. Radical antegrade modular pancreatosplenectomy. Surgery. 2003; 133:521–527.6. Chang YR, Han SS, Park SJ, Lee SD, Yoo TS, Kim YK, et al. Surgical outcome of pancreatic cancer using radical antegrade modular pancreatosplenectomy procedure. World J Gastroenterol. 2012; 18:5595–5600.7. Strasberg SM, Linehan DC, Hawkins WG. Radical antegrade modular pancreatosplenectomy procedure for adenocarcinoma of the body and tail of the pancreas: ability to obtain negative tangential margins. J Am Coll Surg. 2007; 204:244–249.8. O'Morchoe CC. Lymphatic system of the pancreas. Microsc Res Tech. 1997; 37:456–477.9. Strasberg SM, Fields R. Left-sided pancreatic cancer: distal pancreatectomy and its variants: radical antegrade modular pancreatosplenectomy and distal pancreatectomy with celiac axis resection. Cancer J. 2012; 18:562–570.10. DeOliveira ML, Winter JM, Schafer M, Cunningham SC, Cameron JL, Yeo CJ, et al. Assessment of complications after pancreatic surgery: a novel grading system applied to 633 patients undergoing pancreaticoduodenectomy. Ann Surg. 2006; 244:931–937.11. Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005; 138:8–13.12. Ohtsuka T, Tanaka M, Miyazaki K. Gastrointestinal function and quality of life after pylorus-preserving pancreatoduodenectomy. J Hepatobiliary Pancreat Surg. 2006; 13:218–224.13. Rashid L, Velanovich V. Symptomatic change and gastrointestinal quality of life after pancreatectomy. HPB (Oxford). 2012; 14:9–13.14. Hirano S, Kondo S, Tanaka E, Shichinohe T, Tsuchikawa T, Kato K, et al. Postoperative bowel function and nutritional status following distal pancreatectomy with en-bloc celiac axis resection. Dig Surg. 2010; 27:212–216.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally invasive radical antegrade modular pancreatosplenectomy: routine vs. modified
- A Five-Year Survivor without Recurrence Following Robotic Anterior Radical Antegrade Modular Pancreatosplenectomy for a Well-Selected Left-Sided Pancreatic Cancer
- Transfusion free radical antegrade modular pancreaticosplenectomy of metastatic neuroendocrine tumor of the pancreas in Jehovah's Witness patient
- Port-site metastasis after laparoscopic radical pancreatosplenectomy in left-sided pancreatic cancer
- ERRATUM: Correction of the 1st and 2nd authors' affiliation: Transfusion free radical antegrade modular pancreaticosplenectomy of metastatic neuroendocrine tumor of the pancreas in Jehovah's Witness patient