J Korean Surg Soc.
2012 Jun;82(6):365-369.
Ten year outcomes after bypass surgery in aortoiliac occlusive disease
- Affiliations
-
- 1Division of Vascular Surgery, Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. dikim@skku.edu
- 2Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
Abstract
- PURPOSE
Most outcome studies of bypass surgery are limited to five years of follow-up. However, as human life expectancy has increased, analyses of more long-term outcomes are needed. The aim of this study is to evaluate 10-year outcomes of anatomical bypasses in aortoiliac occlusive disease.
METHODS
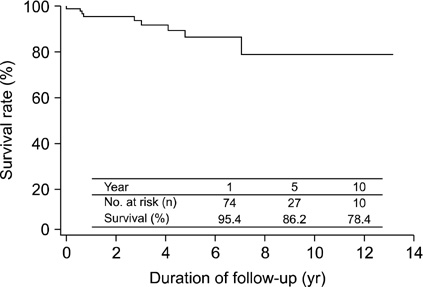
From 1996 to 2009, 92 patients (82 males and 10 females) underwent aortic anatomical bypasses to treat aortoiliac occlusive disease at Samsung Medical Center. The patients were reviewed retrospectively. Kaplan-Meier survival analyses were performed using PASW ver. 18.0 (IBM Co).
RESULTS
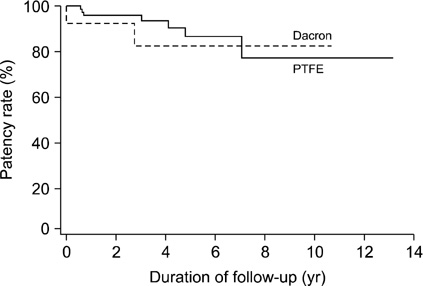
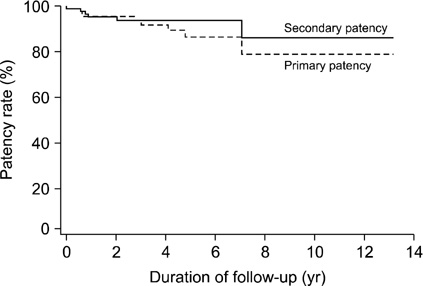
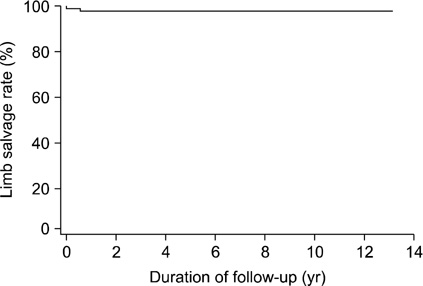
A total of 72 patients (78.3%) underwent aorto-femoral bypasses (uni- or bi-femoral), 15 patients (16.3%) underwent aorto-iliac bypasses (uni- or bi-iliac), and 5 patients (5.4%) underwent aorto-iliac and aorto-femoral bypasses. The overall primary patency rates of the 92 patients were 86.2% over 5 years and 77.6% over 10 years. The 10-year limb salvage rate and overall survival rate were 97.7% and 91.7%, respectively.
CONCLUSION
The overall patency rates of bypass graft and limb salvage rates decreased as time passed. The analysis of results after bypass surgery to treat arterial occlusive disease will be needed to extend for 10 years of follow-up.
MeSH Terms
Figure
Reference
-
1. Szilagyi DE, Elliott JP Jr, Smith RF, Reddy DJ, McPharlin M. A thirty-year survey of the reconstructive surgical treatment of aortoiliac occlusive disease. J Vasc Surg. 1986. 3:421–436.2. Leriche R, Morel A. The syndrome of thrombotic obliteration of the aortic bifurcation. Ann Surg. 1948. 127:193–206.3. Park UJ, Kim DI. Thromoboagiitis obliterans (TAO). Int J Stem Cells. 2010. 3:1–7.4. de Vries SO, Hunink MG. Results of aortic bifurcation grafts for aortoiliac occlusive disease: a meta-analysis. J Vasc Surg. 1997. 26:558–569.5. Brewster DC. Current controversies in the management of aortoiliac occlusive disease. J Vasc Surg. 1997. 25:365–379.6. Kashyap VS, Pavkov ML, Bena JF, Sarac TP, O'Hara PJ, Lyden SP, et al. The management of severe aortoiliac occlusive disease: endovascular therapy rivals open reconstruction. J Vasc Surg. 2008. 48:1451–1457.e3.7. Kim IH, Kim DI, Huh SH, Lee BB, Kim DK, Do YS, et al. Clinical experiences of the arterial bypass in aortoiliac occlusive disease. J Korean Surg Soc. 2001. 61:600–603.8. Di Centa I, Coggia M, Cerceau P, Javerliat I, Alfonsi P, Beauchet A, et al. Total laparoscopic aortobifemoral bypass: short- and middle-term results. Ann Vasc Surg. 2008. 22:227–232.9. Novotny T, Dvorak M, Staffa R. The learning curve of robot-assisted laparoscopic aortofemoral bypass grafting for aortoiliac occlusive disease. J Vasc Surg. 2011. 53:414–420.10. Davidovic L, Vasic D, Maksimovic R, Kostic D, Markovic D, Markovic M. Aortobifemoral grafting: factors influencing long-term results. Vascular. 2004. 12:171–178.11. Takagi H, Goto SN, Matsui M, Manabe H, Umemoto T. A contemporary meta-analysis of Dacron versus polytetrafluoroethylene grafts for femoropopliteal bypass grafting. J Vasc Surg. 2010. 52:232–236.12. Miles JR Jr, Miles DG, Johnson G Jr. Aortoiliac operations and sexual dysfunction. Arch Surg. 1982. 117:1177–1181.13. Cormio L, Edgren J, Lepantalo M, Lindfors O, Nisen H, Saarinen O, et al. Aortofemoral surgery and sexual function. Eur J Vasc Endovasc Surg. 1996. 11:453–457.14. Flanigan DP, Schuler JJ, Keifer T, Schwartz JA, Lim LT. Elimination of iatrogenic impotence and improvement of sexual function after aortoiliac revascularization. Arch Surg. 1982. 117:544–550.15. Hertzer NR, Beven EG, Young JR, O'Hara PJ, Ruschhaupt WF 3rd, Graor RA, et al. Coronary artery disease in peripheral vascular patients: a classification of 1000 coronary angiograms and results of surgical management. Ann Surg. 1984. 199:223–233.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The accidental renal artery embolism in patient with aortoiliac occlusive disease with unilateral renal atrophy during aortobifemoral bypass graft: A case report
- Surgical Treatment of Aortoiliac Occlusive Disease
- Outcomes of Unibody Bifurcated Endograft and Aortobifemoral Bypass for Aortoiliac Occlusive Disease
- Endovascular Revascularization for Aortoiliac Occlusive Disease
- Single Tract Aortic Revascularization Technique in the Treatment of Aortoiliac Occlusive Disease