J Korean Soc Radiol.
2011 Sep;65(3):235-240.
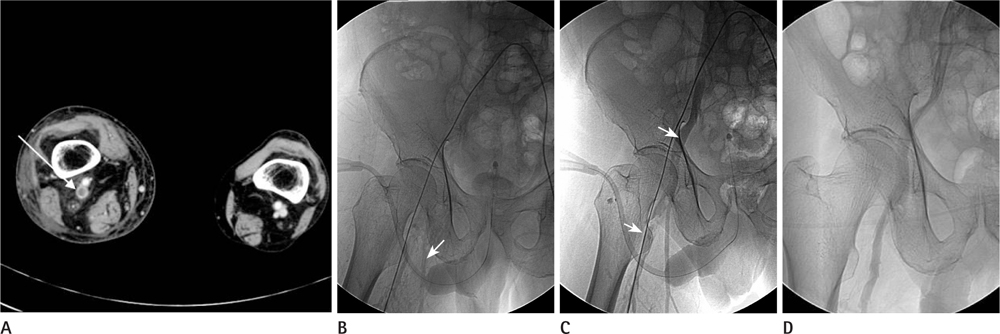
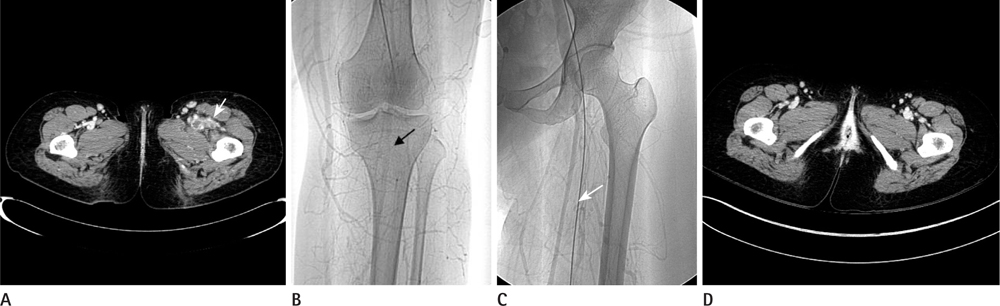
Intra-Arterial Thrombolysis for Deep Vein Thrombosis of the Lower Extremity: Case Report
- Affiliations
-
- 1Department of Radiology, Wonkwang University School of Medicine, Iksan, Korea. bsroh@wonkwang.ac.kr
Abstract
- If the appropriate catheterization of the affected vein was not possible because of a narrowed or thrombus-filled venous lumen, successful treatment gets into trouble during catheter directed regional thrombolysis for treatment of deep vein thrombosis. In this situation, intra-arterial thrombolysis can be considered as an alternative treatment, but to the best of our knowledge, only two reports have been described. We present here cases of successful intra-arterial thrombolysis in patients with deep vein thrombosis.
MeSH Terms
Figure
Reference
-
1. Sharafuddin MJ, Sun S, Hoballah JJ, Youness FM, Sharp WJ, Roh BS. Endovascular management of venous thrombotic and occlusive diseases of the lower extremities. J Vasc Interv Radiol. 2003; 14:405–423.2. Lee KH, Han H, Lee KJ, Yoon CS, Kim SH, Won JY, et al. Mechanical thrombectomy of acute iliofemoral deep vein thrombosis with use of an Arrow-Trerotola percutaneous thrombectomy device. J Vasc Interv Radiol. 2006; 17:487–495.3. Roh BS. Endovascular management of deep venous thrombotic diseases of the lower extremity. J Korean Radiol Soc. 2004; 51:1–12.4. Wlodarczyk ZK, Gibson M, Dick R, Hamilton G. Low-dose intra-arterial thrombolysis in the treatment of phlegmasia caerulea dolens. Br J Surg. 1994; 81:370–372.5. Garg SK, Yadav KS. Developing venous gangrene in deep vein thrombosis: intraarterial low-dose burst therapy with urokinase--case reports. Angiology. 1999; 50:157–162.6. Henao EA, Bohannon WT, Silva MB Jr. Treatment of portal venous thrombosis with selective superior mesenteric artery infusion of recombinant tissue plasminogen activator. J Vasc Surg. 2003; 38:1411–1415.7. Paques M, Vallée JN, Herbreteau D, Aymart A, Santiago PY, Campinchi-Tardy F, et al. Superselective ophthalmic artery fibrinolytic therapy for the treatment of central retinal vein occlusion. Br J Ophthalmol. 2000; 84:1387–1391.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Upper Extremity Deep Vein Thrombosis after Clavicle Fracture and Immobilization
- The Incidence of Deep Vein Thrombosis in the Lower Extremity
- A Case of Upper Extremity Deep Vein Thrombosis and Pulmonary Thromboembolism in a Severely Obese Man
- Vascular Interventional Procedures Often Encountered by Primary Physicians
- Catheter Directed Thrombolysis for Deep Vein Thrombosis during the First Trimester of Pregnancy: Two Case Reports