J Korean Soc Radiol.
2013 Jan;68(1):9-16.
Comparison of Diagnostic Usefulness of Multi-Channel CT Perfusion and Conventional Brain CT in the Acute Pontine Infarct
- Affiliations
-
- 1Department of Radiology, Wonju Christian Hospital, Wonju College of Medicine, Yonsei University, Wonju, Korea. kim0328@yonsei.ac.kr
Abstract
- PURPOSE
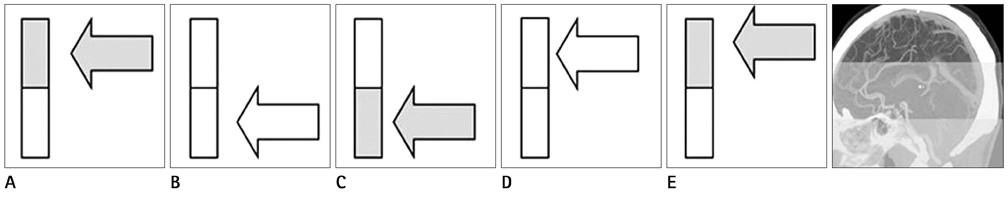
CT perfusion (CTP) is an important modality in the diagnosis of acute stroke, and the range of its use is gradually expanding from supratentorial to whole brain stroke. We assessed the diagnostic value of multichannel CTP in comparison with conventional CT (CT) in acute pontine infarct.
MATERIALS AND METHODS
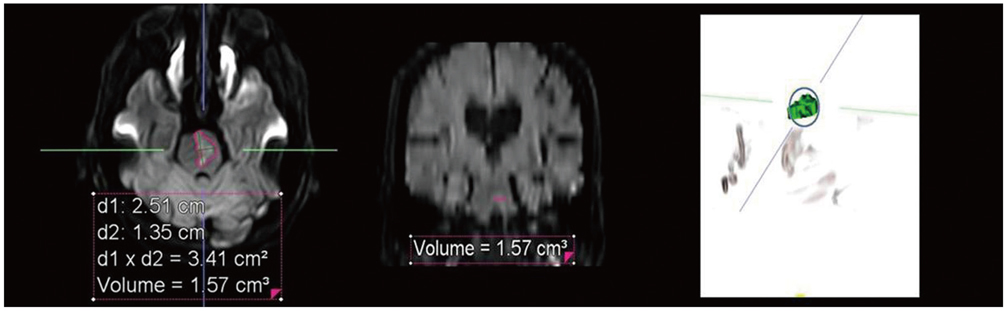
CTP and follow-up diffusion weighted magnetic resonance imaging were performed in 74 patients diagnosed with acute pontine infarct among 178 suspicious ones. Diagnostic accuracy of CTP and CT was evaluated and quantitative analysis was performed to define the factors that may influence the detection rate.
RESULTS
In the diagnosis of acute pontine infarct, the sensitivity, specificity, and accuracy of CTP was 56.8%, 91.4%, and 77.0% and of conventional CT scan was 47.3%, 93.3%, and 74.2%, respectively. There was no statistically significant difference. Receiver operation characteristic curve revealed both types of imaging to have diagnostic usefulness (p < 0.01) in acute pontine infarct. Among the factors that may affect the detection rate, infarct volume was found to be statistically significant (CTP: p < 0.01, CT: p = 0.01).
CONCLUSION
This is the first study that analyzed the difference between CTP and CT in the diagnostic accuracy of acute pontine infarction. Both CTP and CT are useful diagnostic tools although CTP seems to have a slightly higher detection rate than CT.
MeSH Terms
Figure
Reference
-
1. Ledezma CJ, Wintermark M. Multimodal CT in stroke imaging: new concepts. Radiol Clin North Am. 2009. 47:109–116.2. Lee IH, You JH, Lee JY, Whang K, Kim MS, Kim YJ, et al. Accuracy of the detection of infratentorial stroke lesions using perfusion CT: an experimenter-blinded study. Neuroradiology. 2010. 52:1095–1100.3. Roberts HC, Roberts TP, Smith WS, Lee TJ, Fischbein NJ, Dillon WP. Multisection dynamic CT perfusion for acute cerebral ischemia: the "toggling-table" technique. AJNR Am J Neuroradiol. 2001. 22:1077–1080.4. Koenig M, Klotz E, Luka B, Venderink DJ, Spittler JF, Heuser L. Perfusion CT of the brain: diagnostic approach for early detection of ischemic stroke. Radiology. 1998. 209:85–93.5. Axel L. Tissue mean transit time from dynamic computed tomography by a simple deconvolution technique. Invest Radiol. 1983. 18:94–99.6. Wintermark M, Fischbein NJ, Smith WS, Ko NU, Quist M, Dillon WP. Accuracy of dynamic perfusion CT with deconvolution in detecting acute hemispheric stroke. AJNR Am J Neuroradiol. 2005. 26:104–112.7. Youn SW, Kim JH, Weon YC, Kim SH, Han MK, Bae HJ. Perfusion CT of the brain using 40-mm-wide detector and toggling table technique for initial imaging of acute stroke. AJR Am J Roentgenol. 2008. 191:W120–W126.8. Röther J, Jonetz-Mentzel L, Fiala A, Reichenbach JR, Herzau M, Kaiser WA, et al. Hemodynamic assessment of acute stroke using dynamic single-slice computed tomographic perfusion imaging. Arch Neurol. 2000. 57:1161–1166.9. Nabavi DG, Cenic A, Craen RA, Gelb AW, Bennett JD, Kozak R, et al. CT assessment of cerebral perfusion: experimental validation and initial clinical experience. Radiology. 1999. 213:141–149.10. Choi JH, Seo JJ, Kim JK, Chung TW, Jeong YY, Park JG, et al. The usefulness of perfusion CT in acute cerebral ischemic infarction. J Korean Radiol Soc. 2003. 49:7–14.11. Mayer TE, Hamann GF, Baranczyk J, Rosengarten B, Klotz E, Wiesmann M, et al. Dynamic CT perfusion imaging of acute stroke. AJNR Am J Neuroradiol. 2000. 21:1441–1449.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Usefulness of Perfusion CT in Acute Cerebral Ischemic Infarction
- Clinical Usefulness of Perfusion CT in Acute Ischemic Stroke
- Imaging Diagnosis of Occlusive Cerebrovascular Diseases and Cerebral Infarction
- Multiphasic Perfusion CT in Acute Middle Cerebral Artery Ischemic Stroke: Prediction of Final Infarct Volume and Correlation with Clinical Outcome
- Early Diagnosis of Acute Ischemic Stroke by Using 16 row Multi-slice Computed Tomography