World J Mens Health.
2012 Aug;30(2):123-130.
Strong Impact of Nocturia on Sleep Quality in Patients with Lower Urinary Tract Symptoms
- Affiliations
-
- 1Department of Urology, Soon Chun Hyang University College of Medicine, Seoul, Korea. yssong@schmc.ac.kr
- 2Medical Research Institute, Chung-Ang University School of Medicine, Seoul, Korea.
- 3Division of Neurology, Department of Medicine, University of British Columbia, Vancouver, Canada.
Abstract
- PURPOSE
Nocturia is a bothersome symptom that impacts sleep quality in patients with lower urinary tract symptoms (LUTS)/benign prostatic hyperplasia (BPH). This study was performed to evaluate the impact of nocturia on sleep quality.
MATERIALS AND METHODS
A total of 58 male patients with LUTS/BPH were enrolled. LUTS/BPH patients without nocturia were included in the control group. The inclusion criteria were eight or more points on the International Prostate System Score (IPSS) including more than one episode of nocturia and a prostate volume larger than 20 ml. IPSS, prostate volume, uroflowmetry, and the Pittsburgh Sleep Quality Index (PSQI) from each patient were recorded.
RESULTS
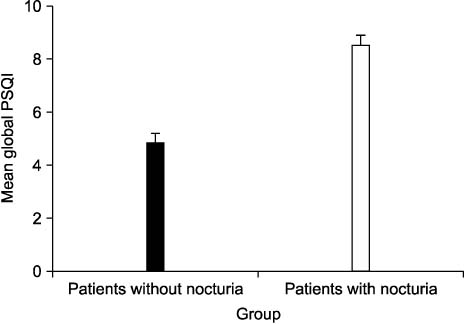
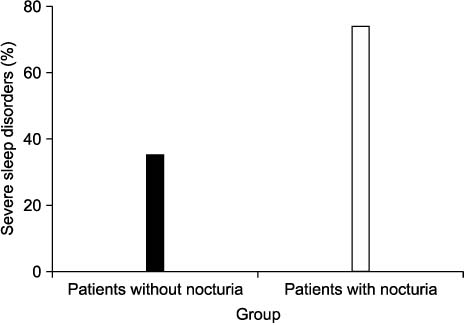
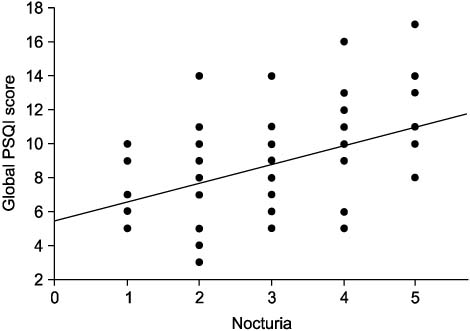
Patients with nocturia showed a higher mean global PSQI (8.5+/-0.4) than patients without nocturia (4.82+/-0.4) (p<0.01). Patients with nocturia showed a higher percentage of severe sleep disorders (74.1%) than patients without nocturia (35.3%) (p<0.01). The regression coefficient between the number of episodes of nocturia and mean global PSQI was 0.42 (p<0.01).
CONCLUSIONS
Patients with nocturia showed poor sleep quality, and this was related to the number of episodes of nocturia. This suggests that nocturia has a strong impact on sleep quality in patients with LUTS/BPH.
Keyword
MeSH Terms
Figure
Reference
-
1. Eckhardt MD, van Venrooij GE, van Melick HH, Boon TA. Prevalence and bothersomeness of lower urinary tract symptoms in benign prostatic hyperplasia and their impact on well-being. J Urol. 2001. 166:563–568.
Article2. Jolleys JV, Donovan JL, Nanchahal K, Peters TJ, Abrams P. Urinary symptoms in the community: how bothersome are they? Br J Urol. 1994. 74:551–555.
Article3. Abrams P. Nocturia: the major problem in patients with lower urinary tract symptoms suggestive of benign prostatic obstruction (LUTS/BPO). Eur Urol. 2005. 3:Suppl. 8–16.
Article4. Stanley N. The underestimated impact of nocturia on quality of life. Eur Urol. 2005. 4:Suppl. 17–19.
Article5. Kim BS, Lee JW, Kim YT, Park HY, Kwon SW, Lee TY. The prevalence and risk factors of nocturia for males participating in a prostate examination survey. Korean J Urol. 2008. 49:818–825.
Article6. van Kerrebroeck P, Abrams P, Chaikin D, Donovan J, Fonda D, Jackson S, et al. Standardisation Sub-committee of the International Continence Society. The standardisation of terminology in nocturia: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002. 21:179–183.
Article7. Chapple CR. Night time symptom control with Omnic (Tamsulosin) Oral Controlled Absorption System (OCAS®). Eur Urol. 2005. 4:Suppl. 14–16.
Article8. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989. 28:193–213.
Article9. De Gennaro L, Martina M, Curcio G, Ferrara M. The relationship between alexithymia, depression, and sleep complaints. Psychiatry Res. 2004. 128:253–258.
Article10. Abraham L, Hareendran A, Mills IW, Martin ML, Abrams P, Drake MJ, et al. Development and validation of a quality-of-life measure for men with nocturia. Urology. 2004. 63:481–486.
Article11. Jackson S. Lower urinary tract symptoms and nocturia in men and women: prevalence, aetiology and diagnosis. BJU Int. 1999. 84:Suppl 1. 5–8.
Article12. Asplund R. The nocturnal polyuria syndrome (NPS). Gen Pharmacol. 1995. 26:1203–1209.
Article13. Coyne KS, Zhou Z, Bhattacharyya SK, Thompson CL, Dhawan R, Versi E. The prevalence of nocturia and its effect on health-related quality of life and sleep in a community sample in the USA. BJU Int. 2003. 92:948–954.
Article14. Stewart RB, Moore MT, May FE, Marks RG, Hale WE. Nocturia: a risk factor for falls in the elderly. J Am Geriatr Soc. 1992. 40:1217–1220.
Article15. Kobelt G, Borgström F, Mattiasson A. Productivity, vitality and utility in a group of healthy professionally active individuals with nocturia. BJU Int. 2003. 91:190–195.
Article16. Asplund R. Nocturia: consequences for sleep and daytime activities and associated risks. Eur Urol. 2005. 3:Suppl. 24–32.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nocturia is the Lower Urinary Tract Symptom With Greatest Impact on Quality of Life of Men From a Community Setting
- Impact of Nocturia on Health-Related Quality of Life and Medical Outcomes Study Sleep Score in Men
- Testosterone Deficiency and Nocturia: A Review
- Lower Urinary Tract Symptoms in Chronic Stroke Survivors: Frequency and Impact on Quality of Life
- Nocturia: The circadian voiding disorder