World J Mens Health.
2015 Apr;33(1):1-7. 10.5534/wjmh.2015.33.1.1.
Sperm DNA Fragmentation and Standard Semen Parameters in Algerian Infertile Male Partners
- Affiliations
-
- 1Department of Natural and Life Sciences, Faculty of Sciences, Hadj Lakhdar University, Batna, Algeria.
- 2Department of Medicine, Faculty of Medicine, Hadj Lakhdar University, Batna, Algeria. contact_genetique@yahoo.fr
- KMID: 2320733
- DOI: http://doi.org/10.5534/wjmh.2015.33.1.1
Abstract
- PURPOSE
To date, standard semen parameters have been the only parameters investigated in sperm samples of infertile men in Algeria. We investigated, for the first time, semen parameters according to sperm DNA fragmentation (SDF) in these subjects.
MATERIALS AND METHODS
SDF was determined by a validated sperm chromatin dispersion test in 26 infertile men. Patients were split into two groups according to the SDF level estimated by the DNA fragmentation index (DFI): the low fragmentation group (LFG; LFG with DFI < or =18%) and high fragmentation group (HFG; HFG with DFI >18%). The standard semen parameters were measured in both groups.
RESULTS
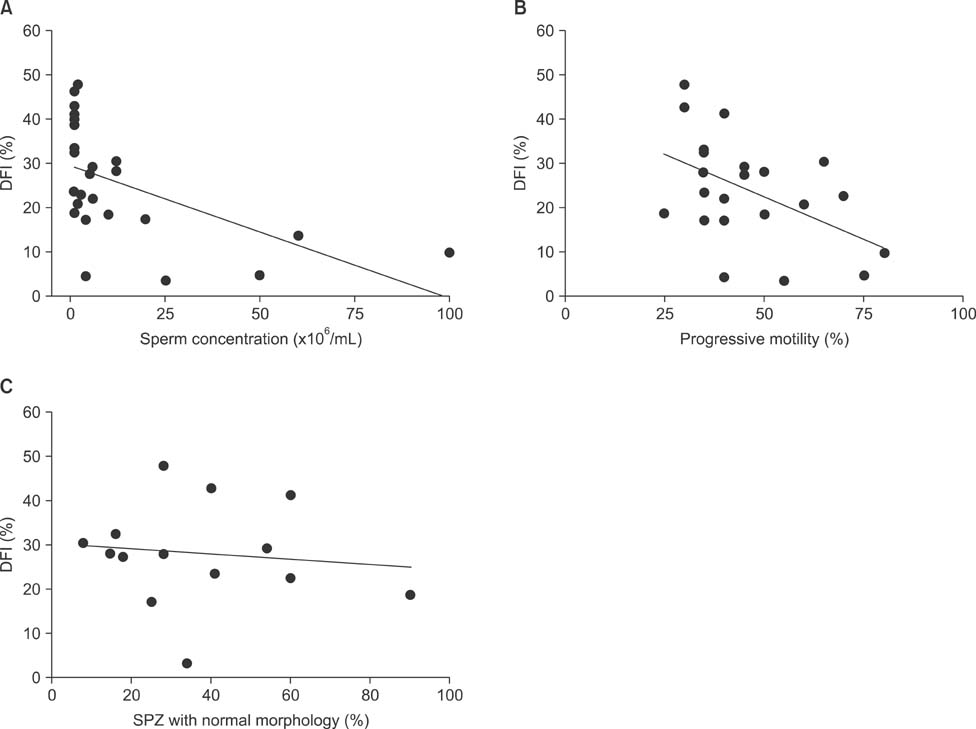
We found that semen concentration and motility were negatively correlated with DFI (r=-0.65, r=-0.45, respectively; p<0.05), while morphology and semen volume were not correlated with it (r=0.24, r=-0.18, respectively; p>0.05). Comparison of the sperm concentration revealed that it was significantly higher in LFG than in HFG (37.57%+/-13.16% vs. 7.32%+/-3.59%, respectively; p<0.05), whereas no significant difference was observed regarding sperm motility and morphology.
CONCLUSIONS
Our findings suggest that SDF correlates well with both sperm motility and concentration but not with morphology. Thus, we conclude that SDF evaluation provides additional information regarding sperm quality, and should be used as a complementary test for assessing semen characteristics in infertile males.
Keyword
MeSH Terms
Figure
Reference
-
1. World Health Organization (WHO). WHO laboratory manual for the examination and processing of human semen. 5th ed. Geneva: WHO;2010.2. Gao J, Gao ES, Walker M, Yang Q, Wu JQ, Zhu QX, et al. Reference values of semen parameters for healthy Chinese men. Urol Int. 2008; 81:256–262.
Article3. Nallella KP, Sharma RK, Aziz N, Agarwal A. Significance of sperm characteristics in the evaluation of male infertility. Fertil Steril. 2006; 85:629–634.
Article4. Barratt CL, Björndahl L, Menkveld R, Mortimer D. ESHRE special interest group for andrology basic semen analysis course: a continued focus on accuracy, quality, efficiency and clinical relevance. Hum Reprod. 2011; 26:3207–3212.
Article5. Guzick DS, Overstreet JW, Factor-Litvak P, Brazil CK, Nakajima ST, Coutifaris C, et al. Sperm morphology, motility, and concentration in fertile and infertile men. N Engl J Med. 2001; 345:1388–1393.
Article6. Lewis SE. Is sperm evaluation useful in predicting human fertility? Reproduction. 2007; 134:31–40.
Article7. Barratt CL, Aitken RJ, Björndahl L, Carrell DT, de Boer P, Kvist U, et al. Sperm DNA: organization, protection and vulnerability: from basic science to clinical applications: a position report. Hum Reprod. 2010; 25:824–838.8. Nijs M, Creemers E, Cox A, Franssen K, Janssen M, Vanheusden E, et al. Chromomycin A3 staining, sperm chromatin structure assay and hyaluronic acid binding assay as predictors for assisted reproductive outcome. Reprod Biomed Online. 2009; 19:671–684.
Article9. Swan SH, Brazil C, Drobnis EZ, Liu F, Kruse RL, Hatch M, et al. Study For Future Families Research Group. Geographic differences in semen quality of fertile U.S. males. Environ Health Perspect. 2003; 111:414–420.
Article10. Iwamoto T, Nozawa S, Yoshiike M, Namiki M, Koh E, Kanaya J, et al. Semen quality of fertile Japanese men: a cross-sectional population-based study of 792 men. BMJ Open. 2013; 3:doi: 10.1136/bmjopen-2012-002223.
Article11. World Health Organization (WHO). WHO laboratory manual for the examination of human semen and sperm-cervical mucus interaction. 4th ed. Cambridge: Cambridge University Press;1999.12. David G. Editorial: sperm banks in France. Arch Fr Pediatr. 1975; 32:401–404.13. Fernández JL, Muriel L, Rivero MT, Goyanes V, Vazquez R, Alvarez JG. The sperm chromatin dispersion test: a simple method for the determination of sperm DNA fragmentation. J Androl. 2003; 24:59–66.14. Halotech DNA [Internet]. Madrid: Halotech DNA;accessed 2014 Dec 10. Available from: http://www.halotechdna.com/productlist/.15. Velez de la Calle JF, Muller A, Walschaerts M, Clavere JL, Jimenez C, Wittemer C, et al. Sperm deoxyribonucleic acid fragmentation as assessed by the sperm chromatin dispersion test in assisted reproductive technology programs: results of a large prospective multicenter study. Fertil Steril. 2008; 90:1792–1799.
Article16. Chohan KR, Griffin JT, Lafromboise M, De Jonge CJ, Carrell DT. Comparison of chromatin assays for DNA fragmentation evaluation in human sperm. J Androl. 2006; 27:53–59.
Article17. Brahem S, Mehdi M, Landolsi H, Mougou S, Elghezal H, Saad A. Semen parameters and sperm DNA fragmentation as causes of recurrent pregnancy loss. Urology. 2011; 78:792–796.
Article18. Erenpreiss J, Elzanaty S, Giwercman A. Sperm DNA damage in men from infertile couples. Asian J Androl. 2008; 10:786–790.
Article19. Khalili MA, Aghaie-Maybodi F, Anvari M, Talebi AR. Sperm nuclear DNA in ejaculates of fertile and infertile men: correlation with semen parameters. Urol J. 2006; 3:154–159.20. Cohen-Bacrie P, Belloc S, Ménézo YJ, Clement P, Hamidi J, Benkhalifa M. Correlation between DNA damage and sperm parameters: a prospective study of 1,633 patients. Fertil Steril. 2009; 91:1801–1805.
Article21. Marchiani S, Tamburrino L, Forti G, Baldi E, Muratori M. M540 bodies and their impact on flow cytometric analyses of human spermatozoa. Soc Reprod Fertil Suppl. 2007; 65:509–514.22. Muratori M, Marchiani S, Tamburrino L, Tocci V, Failli P, Forti G, et al. Nuclear staining identifies two populations of human sperm with different DNA fragmentation extent and relationship with semen parameters. Hum Reprod. 2008; 23:1035–1043.
Article23. Nuñez-Calonge R, Caballero P, López-Fernández C, Guijarro JA, Fernández JL, Johnston S, et al. An improved experimental model for understanding the impact of sperm DNA fragmentation on human pregnancy following ICSI. Reprod Sci. 2012; 19:1163–1168.
Article24. Ribas-Maynou J, García-Peiró A, Fernández-Encinas A, Abad C, Amengual MJ, Prada E, et al. Comprehensive analysis of sperm DNA fragmentation by five different assays: TUNEL assay, SCSA, SCD test and alkaline and neutral Comet assay. Andrology. 2013; 1:715–722.
Article25. Bungum M, Humaidan P, Spano M, Jepson K, Bungum L, Giwercman A. The predictive value of sperm chromatin structure assay (SCSA) parameters for the outcome of intrauterine insemination, IVF and ICSI. Hum Reprod. 2004; 19:1401–1408.
Article26. Duran EH, Morshedi M, Taylor S, Oehninger S. Sperm DNA quality predicts intrauterine insemination outcome: a prospective cohort study. Hum Reprod. 2002; 17:3122–3128.
Article27. Erenpreiss J, Spano M, Erenpreisa J, Bungum M, Giwercman A. Sperm chromatin structure and male fertility: biological and clinical aspects. Asian J Androl. 2006; 8:11–29.
Article28. Hikim AP, Wang C, Leung A, Swerdloff RS. Involvement of apoptosis in the induction of germ cell degeneration in adult rats after gonadotropin-releasing hormone antagonist treatment. Endocrinology. 1995; 136:2770–2775.
Article29. Barroso G, Morshedi M, Oehninger S. Analysis of DNA fragmentation, plasma membrane translocation of phosphatidylserine and oxidative stress in human spermatozoa. Hum Reprod. 2000; 15:1338–1344.
Article30. Høst E, Lindenberg S, Kahn JA, Christensen F. DNA strand breaks in human sperm cells: a comparison between men with normal and oligozoospermic sperm samples. Acta Obstet Gynecol Scand. 1999; 78:336–339.
Article31. Zini A, Kamal K, Phang D, Willis J, Jarvi K. Biologic variability of sperm DNA denaturation in infertile men. Urology. 2001; 58:258–261.
Article32. Smit M, Dohle GR, Hop WC, Wildhagen MF, Weber RF, Romijn JC. Clinical correlates of the biological variation of sperm DNA fragmentation in infertile men attending an andrology outpatient clinic. Int J Androl. 2007; 30:48–55.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Microsurgical Varicocelectomy on Human Sperm Nucleus DNA Integrity
- Standard Semen Parameters vs. Sperm Kinematics to Predict Sperm DNA Damage
- Correlations between abnormalities of morphological details and DNA fragmentation in human sperm
- Advanced Paternal Age and Sperm DNA Fragmentation: A Systematic Review
- Effects of a short abstinence period on sperm quality in oligozoospermic men