Tuberc Respir Dis.
2015 Jul;78(3):196-202. 10.4046/trd.2015.78.3.196.
Clinical Characteristics of Community-Acquired Viridans Streptococcal Pneumonia
- Affiliations
-
- 1Department of Internal Medicine, Kyungpook National University School of Medicine, Daegu, Korea. sicha@knu.ac.kr
- 2Department of Radiology, Kyungpook National University School of Medicine, Daegu, Korea.
- KMID: 2320643
- DOI: http://doi.org/10.4046/trd.2015.78.3.196
Abstract
- BACKGROUND
Viridans streptococci (VS) are a large group of streptococcal bacteria that are causative agents of community-acquired respiratory tract infection. However, data regarding their clinical characteristics are limited. The purpose of the present study was to investigate the clinical and radiologic features of community-acquired pneumonia (CAP) with or without parapneumonic effusion caused by VS.
METHODS
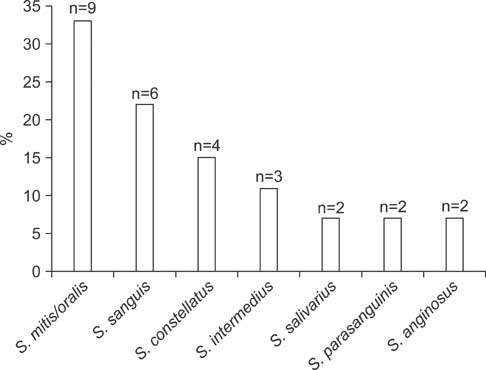
Of 455 consecutive CAP patients with or without parapneumonic effusion, VS were isolated from the blood or pleural fluid in 27 (VS group, 5.9%) patients. Streptococcus pneumoniae was identified as a single etiologic agent in 70 (control group) patients. We compared various clinical parameters between the VS group and the control group.
RESULTS
In univariate analysis, the VS group was characterized by more frequent complicated parapneumonic effusion or empyema and bed-ridden status, lower incidences of productive cough, elevated procalcitonin (>0.5 ng/mL), lower age-adjusted Charlson comorbidity index score, and more frequent ground glass opacity (GGO) or consolidation on computed tomography (CT) scans. Multivariate analysis demonstrated that complicated parapneumonic effusion or empyema, productive cough, bed-ridden status, and GGO or consolidation on CT scans were independent predictors of community-acquired respiratory tract infection caused by VS.
CONCLUSION
CAP caused by VS commonly presents as complicated parapneumonic effusion or empyema. It is characterized by less frequent productive cough, more frequent bed-ridden status, and less common CT pulmonary parenchymal lesions. However, its treatment outcome and clinical course are similar to those of pneumococcal pneumonia.
MeSH Terms
Figure
Reference
-
1. Doern CD, Burnham CA. It's not easy being green: the viridans group streptococci, with a focus on pediatric clinical manifestations. J Clin Microbiol. 2010; 48:3829–3835.2. Tunkel AR, Sepkowitz KA. Infections caused by viridans streptococci in patients with neutropenia. Clin Infect Dis. 2002; 34:1524–1529.3. Waitkins SA, Ratcliffe JG, Roberts C. Streptococcus milleri found in pulmonary empyemas and abscesses. J Clin Pathol. 1985; 38:716–717.4. Sugihara E, Kido Y, Okamoto M, Koyanagi T, Niizeki T, Hirota N, et al. Clinical features of acute respiratory infections associated with the Streptococcus milleri group in the elderly. Kurume Med J. 2004; 51:53–57.5. Sarkar TK, Murarka RS, Gilardi GL. Primary Streptococcus viridans pneumonia. Chest. 1989; 96:831–834.6. Molina JM, Leport C, Bure A, Wolff M, Michon C, Vilde JL. Clinical and bacterial features of infections caused by Streptococcus milleri. Scand J Infect Dis. 1991; 23:659–666.7. Hocken DB, Dussek JE. Streptococcus milleri as a cause of pleural empyema. Thorax. 1985; 40:626–628.8. Shinzato T, Saito A. The Streptococcus milleri group as a cause of pulmonary infections. Clin Infect Dis. 1995; 21:Suppl 3. S238–S243.9. Porta G, Rodriguez-Carballeira M, Gomez L, Salavert M, Freixas N, Xercavins M, et al. Thoracic infection caused by Streptococcus milleri. Eur Respir J. 1998; 12:357–362.10. Jerng JS, Hsueh PR, Teng LJ, Lee LN, Yang PC, Luh KT. Empyema thoracis and lung abscess caused by viridans streptococci. Am J Respir Crit Care Med. 1997; 156:1508–1514.11. Wang JL, Chen KY, Fang CT, Hsueh PR, Yang PC, Chang SC. Changing bacteriology of adult community-acquired lung abscess in Taiwan: Klebsiella pneumoniae versus anaerobes. Clin Infect Dis. 2005; 40:915–922.12. Takayanagi N, Kagiyama N, Ishiguro T, Tokunaga D, Sugita Y. Etiology and outcome of community-acquired lung abscess. Respiration. 2010; 80:98–105.13. Ishida T, Hashimoto T, Arita M, Ito I, Osawa M. Etiology of community-acquired pneumonia in hospitalized patients: a 3-year prospective study in Japan. Chest. 1998; 114:1588–1593.14. American Thoracic Society. Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005; 171:388–416.15. Oh MG, Han MA, Park J, Ryu SY, Park CY, Choi SW. Health behaviors of cancer survivors: the Fourth Korea National Health and Nutrition Examination Survey (KNHANES IV, 2007-09). Jpn J Clin Oncol. 2013; 43:981–987.16. Chalmers JD, Taylor JK, Singanayagam A, Fleming GB, Akram AR, Mandal P, et al. Epidemiology, antibiotic therapy, and clinical outcomes in health care-associated pneumonia: a UK cohort study. Clin Infect Dis. 2011; 53:107–113.17. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–383.18. Fine MJ, Auble TE, Yealy DM, Hanusa BH, Weissfeld LA, Singer DE, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997; 336:243–250.19. Lim WS, van der Eerden MM, Laing R, Boersma WG, Karalus N, Town GI, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003; 58:377–382.20. Cha SI, Shin KM, Jeon KN, Yoo SS, Lee J, Lee SY, et al. Clinical relevance and characteristics of pleural effusion in patients with Mycoplasma pneumoniae pneumonia. Scand J Infect Dis. 2012; 44:793–797.21. Luo YF, Robbins IM, Karatas M, Brixey AG, Rice TW, Light RW. Frequency of pleural effusions in patients with pulmonary arterial hypertension associated with connective tissue diseases. Chest. 2011; 140:42–47.22. Lee SJ, Cha SI, Kim CH, Park JY, Jung TH, Jeon KN, et al. Septic pulmonary embolism in Korea: Microbiology, clinicoradiologic features, and treatment outcome. J Infect. 2007; 54:230–234.23. Christ-Crain M, Muller B. Procalcitonin in bacterial infections: hype, hope, more or less? Swiss Med Wkly. 2005; 135:451–460.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Clinical Characteristics of Pneumococcal and non-Pneumococcal Streptococcal Pneumonia
- Respiratory Review of 2010: Pneumonia
- Community Acquired Pneumonia
- Clinical Significance of Viridans Streptococcal Bacteremia
- A case of fulminant community-acquired Acinetobacter baumannii pneumonia in Korea