Tuberc Respir Dis.
2014 Oct;77(4):188-192. 10.4046/trd.2014.77.4.188.
New-Onset Malignant Pleural Effusion after Abscess Formation of a Subcarinal Lymph Node Associated with Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration
- Affiliations
-
- 1Department of Internal Medicine, Pusan National University School of Medicine, Busan, Korea. ejspulm@gmail.com
- 2Department of Thoracic and Cardiovascular Surgery, Pusan National University School of Medicine, Busan, Korea.
- 3Department of Radiology, Pusan National University School of Medicine, Busan, Korea.
- 4Department of Pathology, Pusan National University School of Medicine, Busan, Korea.
- KMID: 2320577
- DOI: http://doi.org/10.4046/trd.2014.77.4.188
Abstract
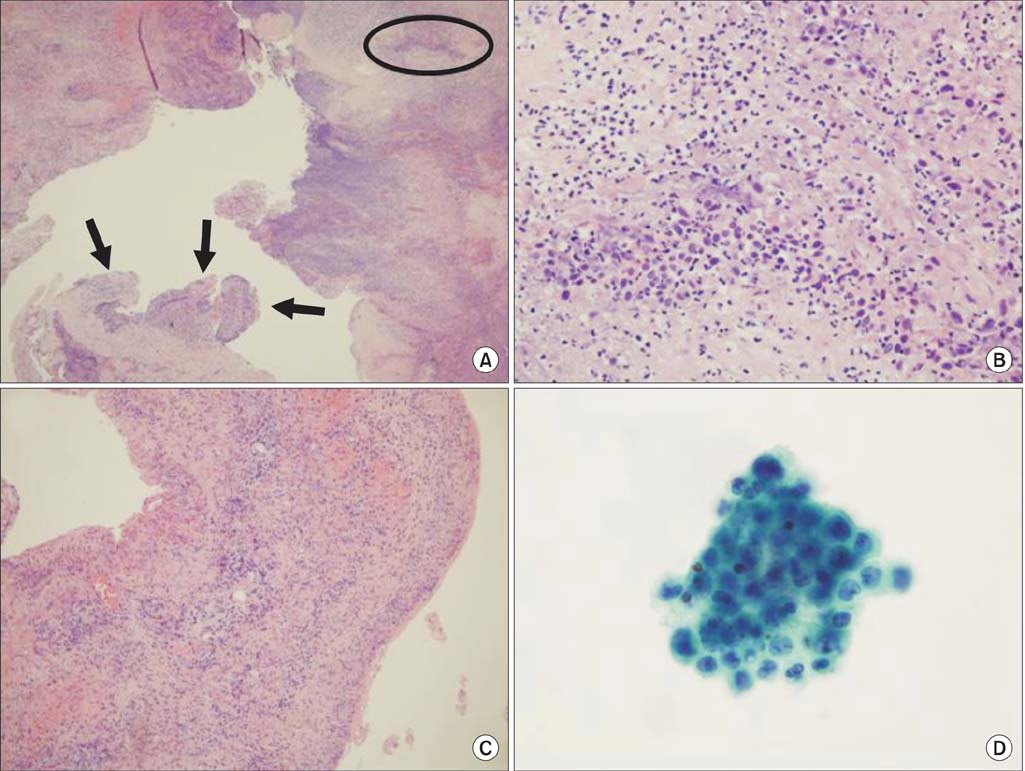
- We present a case of an unusual infectious complication of a ruptured mediastinal abscess after endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA), which led to malignant pleural effusion in a patient with stage IIIA non-small-cell lung cancer. EBUS-TBNA was performed in a 48-year-old previously healthy male, and a mediastinal abscess developed at 4 days post-procedure. Video-assisted thoracoscopic surgery was performed for debridement and drainage, and the intraoperative findings revealed a large volume pleural effusion that was not detected on the initial radiographic evaluation. Malignant cells were unexpectedly detected in the aspirated pleural fluid, which was possibly due to increased pleural permeability and transport of malignant cells originating in a ruptured subcarinal lymph node from the mediastinum to the pleural space. Hence, the patient was confirmed to have squamous cell lung carcinoma with malignant pleural effusion and his TNM staging was changed from stage IIIA to IV.
Keyword
MeSH Terms
Figure
Reference
-
1. Gomez M, Silvestri GA. Endobronchial ultrasound for the diagnosis and staging of lung cancer. Proc Am Thorac Soc. 2009; 6:180–186.2. Evison M, Crosbie PA, Martin J, Bishop P, Doran H, Joseph L, et al. EBUS-TBNA in elderly patients with lung cancer: safety and performance outcomes. J Thorac Oncol. 2014; 9:370–376.3. Kokkonouzis I, Strimpakos AS, Lampaditis I, Tsimpoukis S, Syrigos KN. The role of endobronchial ultrasound in lung cancer diagnosis and staging: a comprehensive review. Clin Lung Cancer. 2012; 13:408–415.4. Asano F, Aoe M, Ohsaki Y, Okada Y, Sasada S, Sato S, et al. Complications associated with endobronchial ultrasound-guided transbronchial needle aspiration: a nationwide survey by the Japan Society for Respiratory Endoscopy. Respir Res. 2013; 14:50.5. Detterbeck FC, Lewis SZ, Diekemper R, Addrizzo-Harris D, Alberts WM. Executive Summary: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013; 143:5 Suppl. 7S–37S.6. Lee JW, Kim WJ, Park CW, Kang HW, Ban HJ, Oh IJ, et al. Endotracheal tuberculous granuloma formation following endobronchial ultrasound transbronchial needle aspiration. Intern Med. 2013; 52:1207–1210.7. Kinsey CM, Arenberg DA. Endobronchial ultrasound-guided transbronchial needle aspiration for non-small cell lung cancer staging. Am J Respir Crit Care Med. 2014; 189:640–649.8. Mohammed KA, Nasreen N, Hardwick J, Logie CS, Patterson CE, Antony VB. Bacterial induction of pleural mesothelial monolayer barrier dysfunction. Am J Physiol Lung Cell Mol Physiol. 2001; 281:L119–L125.9. Mohammed KA, Nasreen N, Hardwick J, Van Horn RD, Sanders KL, Antony VB. Mycobacteria induces pleural mesothelial permeability by down-regulating beta-catenin expression. Lung. 2003; 181:57–66.10. Kang HJ, Hwangbo B. Technical aspects of endobronchial ultrasound-guided transbronchial needle aspiration. Tuberc Respir Dis. 2013; 75:135–139.11. Polkowski M, Larghi A, Weynand B, Boustiere C, Giovannini M, Pujol B, et al. Learning, techniques, and complications of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Technical Guideline. Endoscopy. 2012; 44:190–206.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Malignant Pleural Mesothelioma Diagnosed by Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration
- Is there enough support for endobronchial ultrasound-guided transbronchial needle aspiration as an initial diagnostic tool?
- Technical Aspects of Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration
- The First Pediatric Case of Intrathoracic Tuberculosis Lymphadenitis Diagnosed by Endobronchial Ultrasound Guided Transbronchial Needle Aspiration
- Clinical Implication of Microscopic Anthracotic Pigment in Mediastinal Staging of Non-Small Cell Lung Cancer by Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration