Tuberc Respir Dis.
2013 Dec;75(6):238-243.
Causes and Predictive Factors Associated with "Diagnosis Changed" Outcomes in Patients Notified as Tuberculosis Cases in a Private Tertiary Hospital
- Affiliations
-
- 1Department of Pulmonary and Critical Care Medicine, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. shimts@amc.seoul.kr
Abstract
- BACKGROUND
The aim of our study was to evaluate the "diagnosis changed" rate in patients notified as tuberculosis (TB) on the Korean TB surveillance system (KTBS).
METHODS
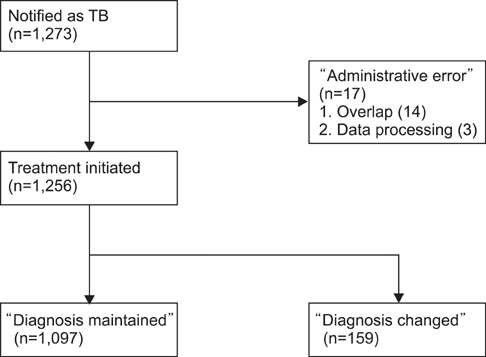
A total of 1,273 patients notified as TB cases on the KTBS in one private tertiary hospital in 2011 were enrolled in the present study. Patients were classified into three groups: "diagnosis maintained", "diagnosis changed" (initially notified as TB, but ultimately diagnosed as non-TB), and "administrative error" (notified as TB due to administrative errors).
RESULTS
Excluding 17 patients in the "administrative error" group, the "diagnosis maintained" and "diagnosis changed" groups included 1,097 (87.3%) and 159 patients (12.7%), respectively. Common causes of "diagnosis changed" were nontuberculous mycobacterial (NTM) disease (51.7%, 61/118), and pneumonia (17.8%) in cases notified as pulmonary TB, and meningitis (19.5%, 8/41) and Crohn's disease (12.2%) in cases notified as extrapulmonary TB. Being older than 35 years of age (odds ratio [OR], 2.18) and a positive acid-fast bacilli stain (OR, 1.58) were positive predictors and a TB-related radiological finding (OR, 0.42) was a negative predictor for a "diagnosis changed" result via multivariate logistic regression analysis in pulmonary TB cases.
CONCLUSION
Because of a high "diagnosis changed" rate in TB notifications to the KTBS, the TB incidence rate measured by the KTBS may be overestimated. Considering the worldwide trend toward increased NTM disease, the "diagnosis changed" rate may increase over time. Thus, when reporting the annual TB notification rate in Korea, the exclusion of "diagnosis changed" cases is desirable.
MeSH Terms
Figure
Reference
-
1. Catanzaro A, Perry S, Clarridge JE, Dunbar S, Goodnight-White S, LoBue PA, et al. The role of clinical suspicion in evaluating a new diagnostic test for active tuberculosis: results of a multicenter prospective trial. JAMA. 2000; 283:639–645.2. Lauzardo M, Ashkin D. Phthisiology at the dawn of the new century. Chest. 2000; 117:1455–1473.3. World Health Organization. Global tuberculosis control 2011. Geneva: World Health Organization;2011.4. Park KD. Tuberculosis management of private health care institution: current situation and task. Tuberc Respir Dis. 2002; 52:579–589.5. Joint Committee for the Development of Korean Guidelines for Tuberculosis, Korea Centers for Disease Control and Prevention. Korean guidelines for tuberculosis. Seoul: Joint Committee for the Development of Korean Guidelines for Tuberculosis, Korea Centers for Disease Control and Prevention;2011.6. Hong YP, Kim SJ, Lew WJ, Lee EK, Han YC. The seventh nationwide tuberculosis prevalence survey in Korea, 1995. Int J Tuberc Lung Dis. 1998; 2:27–36.7. Lew WJ, Lee EG, Bai JY, Kim HJ, Bai GH, Ahn DI, et al. An Internet-based surveillance system for tuberculosis in Korea. Int J Tuberc Lung Dis. 2006; 10:1241–1247.8. Korea Centers for Disease Control & Prevention. Annual report on the notified tuberculosis patients in Korea 2010. Cheongwon: Korea Centers for Disease Control & Prevention;2011.9. Pillaye J, Clarke A. An evaluation of completeness of tuberculosis notification in the United Kingdom. BMC Public Health. 2003; 3:31.10. Jelastopulu E, Alexopoulos EC, Venieri D, Tsiros G, Komninou G, Constantinidis TC, et al. Substantial underreporting of tuberculosis in West implications for local and national surveillance. Euro Surveill. 2009; 14:pii: 19152.11. Cojocaru C, van Hest NA, Mihaescu T, Davies PD. Completeness of notification of adult tuberculosis in Iasi County, Romania: a capture-recapture analysis. Int J Tuberc Lung Dis. 2009; 13:1094–1099.12. Heo E, Oh SY, Jeong I, Lee JS, Lim HJ, Park YS, et al. The diagnostic accuracy of notified new culture-negative pulmonary tuberculosis patients in public healthcare centers. Korean J Med. 2009; 76:44–51.13. Jeong I, Kim HJ, Kim J, Oh SY, Lee JB, Bai JY, et al. Diagnostic accuracy of notified cases as pulmonary tuberculosis in private sectors of Korea. J Korean Med Sci. 2012; 27:525–531.14. World Health Organization. Treatment of tuberculosis guidelines. 4th ed. Geneva: World Health Organization;2010.15. National Tuberculosis Association. Diagnostic standards and classification of tuberculosis. 11th ed. New York: National Tuberculosis Association;1961.16. Koh WJ, Jeong YJ, Kwon OJ, Kim HJ, Cho EH, Lew WJ, et al. Chest radiographic findings in primary pulmonary tuberculosis: observations from high school outbreaks. Korean J Radiol. 2010; 11:612–617.17. Baussano I, Bugiani M, Gregori D, van Hest R, Borraccino A, Raso R, et al. Undetected burden of tuberculosis in a low-prevalence area. Int J Tuberc Lung Dis. 2006; 10:415–421.18. Hong SJ, Park YS, An H, Kang SM, Cho EH, Shin SS. Factors leading to under-reporting of tuberculosis in the private sector in Korea. Int J Tuberc Lung Dis. 2012; 16:1221–1227.19. Olivier KN, Weber DJ, Wallace RJ Jr, Faiz AR, Lee JH, Zhang Y, et al. Nontuberculous mycobacteria. I: multicenter prevalence study in cystic fibrosis. Am J Respir Crit Care Med. 2003; 167:828–834.20. Jeon K, Koh WJ, Kwon OJ, Suh GY, Chung MP, Kim H, et al. Recovery rate of NTM from AFB smear-positive sputum specimens at a medical centre in South Korea. Int J Tuberc Lung Dis. 2005; 9:1046–1051.21. Koh WJ, Kwon OJ, Kim CH, Ahn YM, Lim SY, Yun JW, et al. Clinical characteristics and treatment outcomes of patients with pulmonary tuberculosis at a private general hospital. Tuberc Respir Dis. 2003; 55:154–164.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnostic Accuracy of Notified Cases as Pulmonary Tuberculosis in Private Sectors of Korea
- Is the Tuberculosis Case Reporting Rate of Medical Care Institutions in Private Sector low?
- The Clinical Characteristics, Diagnosis, Treatment, and Outcomes of Patients with Tuberculosis at a Private University Hospital in Korea
- Increased Tuberculosis Burden Due to Demographic Transition in Korea from 2001 to 2010
- Clinical Characteristics and Treatment Outcomes of Patients with Pulmonary Tuberculosis at a Private General Hospital